Subarachnoid Hemorrhage
Bradley R. Foerster
Myria Petrou
Etiology and Epidemiology.
Intracranial aneurysm ruptures are responsible for approximately 80% of nontraumatic subarachnoid hemorrhage (SAH). Saccular aneurysms are the most common type and occur in regions of high mechanical wall shear stress like branch points (circle of Willis, etc.). Fifteen to 20% of patients with SAH have no aneurysm and typically have a perimesencephalic distribution of the clot. The source of hemorrhage is venous in these patients. Other causes of SAH include trauma (most common cause), intracranial and spinal arteriovenous malformation (AVM), hemorrhagic tumor, blood dyscrasias, amyloid angiopathy, moyamoya disease, and secondary leakage of blood from primary intraparenchymal hemorrhage.
Approximately 15-30% of patients die from their aneurysm rupture before reaching the hospital. Up to 25% of patients with an aneurysm have a second aneurysm. Between 0.5 and 1% of patients undergoing cerebral angiography for other reasons are incidentally found to have an aneurysm. The risk of aneurysm rupture in a person with no history of aneurysm rupture varies from 0.05-2% per year depending on the size and site of the aneurysm.
Risk factors for intracranial aneurysm include increasing age, female gender, hypertension, alcohol, smoking, and family history. Intracranial aneurysms are associated with fibromuscular dysplasia, autosomal dominant polycystic kidney disease, connective tissue disorders, congenitally anomalous vessels, AVMs, tumors, vasculitis, and infections.
Symptoms and Signs.
Classically, the symptoms of an intracranial aneurysm rupture include “worst headache of life,” loss of consciousness, photophobia, meningismus, nausea, and vomiting. Only 10-15% of patients who complain of “worst headache of life” will have SAH. Sentinel headaches occur in approximately one half of patients before rupture, presumably caused by transient small leak of the aneurysm. Localized headache may occur from expansion of an aneurysm before rupture, requiring imaging to exclude this diagnosis even in the absence of blood in the cerebrospinal fluid. Expanding aneurysms can also cause focal neurologic deficits including visual field cuts, oculomotor paresis, and focal weakness. Classically, an aneurysm of the posterior communicating artery can cause third cranial nerve palsy with a dilated and relative fixed pupil.
Differential diagnosis includes stroke, migraine, meningitis, and sinusitis.
Complications
Hydrocephalus can be either acute (20% of patients) or delayed. Acute hydrocephalus is related to amount of ventricular blood and usually appears within 3 days of the SAH, requiring immediate treatment. Delayed hydrocephalus occurs after 10 days and is related to amount of SAH.
Seizures occur acutely in 3-5% of patients. Fifteen percent of patients can develop epilepsy following an SAH, usually within the first 18 months.
Rebleeding occurs in up to 4-20% of patients with aneurysms.
Delayed cerebral ischemia is caused by vasospasm and usually occurs 5 days from the initial hemorrhage. Vasospasm can affect any or all of the major branches of the circle of Willis. Ischemic complications have been reported to occur in up to one third of patients, with the amount of blood on the initial head computed tomography (CT) correlating to the severity of the vasospasm.
Neurogenic pulmonary edema and syndrome of inappropriate secretion of antidiuretic hormone (SIADH) are potential systemic complications of SAH.
Overall mortality is high (one third to two thirds of cases). Most survivors have significant permanent disability.
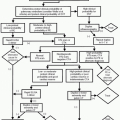
Indications.
A noncontrast head CT is the study of choice in the evaluation of a patient presenting with a severe headache in the emergency room setting. A noncontrast head CT is the fastest, easiest and most accurate test for detection of SAH. It has very high sensitivity (>96%) for the detection of SAH occurring within the last 24 hours. The sensitivity falls to 80% at 72 hours. Head CT is important for risk stratification (more blood = more complications), identification of the potential location of the aneurysm (where most blood is located), and detection of complications which can include hydrocephalus, mass, ischemia, and herniation. Occasionally, a noncontrast CT can identify a calcified aneurysm.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree