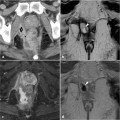
Fig. 10.1
Parks classification of anal fistulas and abscesses 1 Ischiorectal abscess, 2 supralevator abscess, 3 submucosal abscess, 4 perianal abscess, 5 intersphincteric abscess, M puborectalis muscle
The American Gastroenterological Association (AGA) proposed a simpler classification system for fistulas, comprising two groups, simple and complex [7]:
1.
Simple fistulas (low fistulas)
a.
Superficial, low intersphincteric, low intrasphincteric
b.
Single external opening
c.
No perianal abscess
d.
No connection with the vagina or bladder
e.
No rectal stenosis or macroscopic proctitis.
2.
Complex fistulas (high fistulas)
a.
High intersphincteric, high intrasphincteric, suprasphincteric, extras-phincteric
b.
Several external openings
c.
Perianal abscess
d.
Connection with the bladder or vagina
e.
Rectal stenosis or macroscopic proctitis.
10.4 Surgical Principles of EUA
In carrying out EUA, the following surgical instruments are needed (Fig. 10.2):

Anal retractor
Vaginal speculum
Probe and setons
Syringe
Methylene blue or H2O2
Anoscope

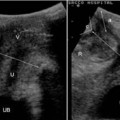
Fig.10.2
Surgical instruments of EUA
Note that it is very important to obtain an extensive informed consent from the patient, because EUA potentially comprises several different surgical procedures.
10.5 Physical Examination
The main aim of a correct perianal examination is to achieve a proper diagnosis and to classify all the abscesses and fistulas, to avoid missing hidden conditions. The surgeon should thoroughly evaluate the perineum, looking for an external opening of the fistula and spontaneous discharges from its orifices. A digital rectal exploration may lead to the detection of fibrotic tissue under the skin, representing the fistula tract, which may also be noted as an induration of the perianal tissue. As discussed above, physical examination allows definition of the type of fistula, according to either the Parks or the AGA classification, and the detection of any connections with the vagina.
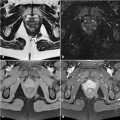
Both the anal retractor and the vaginal speculum can be very useful to identify the fistula’s internal orifice (Figs. 10.3, 10.4).
A standard probing exploration (Fig. 10.5) is mandatory to confirm the type of fistula, to identify internal orifices, and to assess the involvement of the anal sphincters. The syringe-injection of methylene blue or H2O2 (Fig. 10.6) through the orifices of the fistula will in most cases highlight the different tracts in complex fistulas.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree