Emissary veins |
Round smooth-bordered “holes” in the calvaria, marginal sclerosis, typical anatomic location. |
An unusually large emissary vein at an atypical site is suspicious for an angioma or highly vascular intracranial tumor. Imaging best with CT or MRI. |
Diploic venous lakes |
Round, oval lucency in the diploë with corticated margins, occasional central phlebolith, single or multiple. Inner and outer tables are thinned but intact. |
Frequently parietal or occipital adjacent to the transverse sinus. Lakes of unusual size or number may signify an angioma or meningioma. Imaging best with CT or MRI. |
Pacchionian granulations |
Resemble diploic venous lakes, often with a feeding vascular channel. Erosion of the inner table. Possible central phlebolith. |
Occasional thinning and bulging of the outer table, typically in the parasagittal and frontal regions. Seldom noted before 9 y of age. |
Large cisterna magna |
Erosion of the inner table at the center of the inferior occipital squama, similar to a venous lake or larger. |
Findings similar to arachnoid cysts and superficial gliomas. |
Arachnoid cyst |
Localized bulging and thinning of the calvaria. |
Involvement of occipital squama closely resembles a large cisterna magna. |
Enlarged parietal foramina
Fig. 4.6a, b |
Paramedian defects adjacent to the posterior third of the sagittal suture. Location matches that of the parietal fontanelle. |
May communicate across the midline. Familial occurence, relatively common in patients with craniosynostoses. No correlation with brain malformations. |
Encephaloceles; cranium bifidum (accessory fontanelle) |
Round to oval defects with smooth margins, variable size, and no marginal sclerosis. Located in the midline, usually frontal or occipital, sometimes sphenoidal or frontoethmoidal, rarely in the area of the parietal fontanelle; temporal occurrence is very rare. |
The soft-tissue mass over the defect is typical. Skull defect without herniation means cranium bifidum. May coexist with dysplastic corpus callosum and Chiari malformation. |
Pneumatization of the crista galli |
Aerated crista galli should not be mistaken for a frontal encephalocele. |
|
Epidermoid and dermoid |
Indistinguishable on skull films, US, CT, or MRI. Epidermoids are more common. Round or oval defect in the diploë with smooth, well-corticated margins, often located near the lateral canthus or suture. CT and MRI best techniques to rule out intracranial extension. |
Spontaneous resolution is common, further growth rare. Together with Langerhans cell histiocytosis (LCH), the most commonly encountered skull lesions in the pediatric population. |
Langerhans cell histiocytosis
Fig. 4.7a, b
Fig. 4.8a–c |
Single or multiple defects, rounded or irregular, of highly variable size. “Geographic skull.” No marginal sclerosis. |
Bone scan shows a cold lesion with increased uptake at its edges. Other skeletal foci should be ruled out. |
Fibrous dysplasia (FD), aneurysmal bone cyst |
Cyst degeneration may occur within an existing FD lesion, manifesting as acute clinical deterioration. Cyst degeneration occurs most commonly in the sphenoid and frontal bones. Appearance ranges from a simple lesion to aneurysmal bone cyst.
In aneurysmal bone cyst, CT shows the cystic lesion in the diploë, with predominantly inward expansion. Fluid-fluid levels may be seen on both CT and MRI; the latter can also show bleeding within the cyst. |
Cyst degeneration may occur spontaneously within the FD lesion years after the initial diagnosis.
Cavarial aneurysmal bone cyst is rare, with only 3% to 6% of cases occurring in this anatomic location. |
Metastatic neuroblastoma or extension of leukemia in the diploë |
Multiple small and irregular defects with ill-defined margins; may coalesce. |
Neuroblastoma may produce isolated defects and suture widening. |
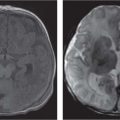
Leptomeningeal cyst (growing fracture)
Fig. 4.9a–c |
Calvarial defect after traumatic dural laceration; irregular; sharp edges with marginal sclerosis. |
Detection weeks to months after the fracture event, due to cerebrospinal fluid (CSF) pulsations. |
Older cephalhematoma |
Irregular osteolysis of the outer table. |
Best depicted on CT. |
Previous craniectomy |
Initially smooth defect that acquires irregular borders with healing. Central sequestrum may be present. |
|
Neurofibromatosis (NF) |
Extensive cranial defects associated with underlying dural ectasia. Best detected on CT. |
Besides defects in the cranium, also at the level of the sphenoid wing. |
Osteomyelitis |
Moth-eaten defects in the cranium. Sequestrum formation rarely seen. |
May be a complication of a craniectomy. |
Hyperparathyroidism |
Disseminated ill-defined lucencies mixed with faint calcifications. Generalized demineralization of the calvaria, sometimes with calcifications in the falx and tentorium. |
Generally secondary (renal osteodystrophy) resorption of the dental laminae dura. Secondary hyper-parathyroidism may cause or result in brown tumors, especially in the facial bones. |
Hemangioma
Fig. 4.10a–c |
May present as a progressive mass. A plain X-ray of the skull, cranial CT, or MRI may show an intraosseous, osteolytic lesion. |
Intraosseous cavernous hemangiomas are a rare finding in the calvarium. These are benign tumors arising from the intrinsic vasculature of the bone. |
Primary calvarial tumors |
Plain films and CT demonstrate an osteolytic mass surrounded by the sclerotic rim within the diploic space. MRI can be used for the evaluation of the intracranial and intraosseous extensions of the tumor. It can be very diff cult to differentiate it from other osteoblastic tumors or from osteoid osteoma.
Malignant tumors, like sarcomas, may also occur in the calvaria. |
Osteoblastoma is an uncommon primary bone tumor that usually involves the vertebrae and the long bones. This tumor rarely develops in the calvaria, showing a preference for the temporal and frontal bones. |
Giant cell tumor |
Can occur in the skull, principally in the sphenoid and temporal bones. Radiographically, the tumors appear osteolytic and radiolucent without a sclerotic border. |
Rarely occurs in patients under 20 y of age. |