Location: 80 % extremities. Lower limb (60 %: thigh, knee, foot, ankle) and upper limb (23 %: forearm, wrist, shoulder). Only 10 % within a joint. Usually, close to a major joint, intimately related to tendons, tendon sheaths, bursae, and beyond the confines of the joint capsule.
Clinical: A palpable deep-seated mass with pain. Pain may be the first symptom of the disease. Tumor grows slowly and insidiously, and the duration of symptoms ranges from 2 to 4 years, although in some cases they have been noted for as long as 20 years.
Imaging: On x-ray: a round or oval, lobulated swelling of moderate density near a joint. Usually, bone is uninvolved. Periosteal reaction, bone erosion, or bone invasion (15–20 %). Multiple, small and spotty calcifications, or cloudy and faded shadow or massive and dense radiopacities of bone formation (40 %). Radiopacities more frequent in the periphery. On angiography: richly hypervascularized. On CT: infiltrating ST mass with slightly higher density than muscle, markedly enhanced, with easily detected calcifications, cortical erosion, and joint invasion when tendons or ligaments are involved. On MRI: 90 % hypointense on T1, hyperintense on T2. Fluid levels (15 %). Marked inhomogeneity, enhancement, and septation on T2. A triple-signal pattern on T2 (30 %): white-like fluid, gray-like fat, and dark-like fibrous tissue. Small high signal areas on T1 (45 %) are foci of hemorrhage. This and the triple pattern are suggestive of SS.
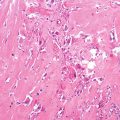
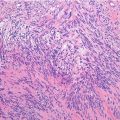
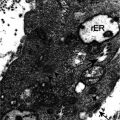
Histopathology: 1–20 cm. Slow-growing lesions are a firm, lobular mass fairly well circumscribed, attached to surrounding tissues, from yellow to gray-white. More rapidly growing lesions are a soft, globose mass poorly encapsulated, with a variegated, friable, or shaggy appearance, from mottled pink-yellow to light brown, with frequent necrosis, hemorrhage, and cystic areas. Calcifications can be seen. Two different types of cells: epithelial and spindle cells. (1) Biphasic type: two cellular components; (2) monophasic fibrous type: only spindle cells; (3) rare monophasic epithelial type: only epithelioid cells; and (4) poorly differentiated type (20 %). In type (1), there is a balanced distribution of the two components. Epithelioid cells are globose, cubic, or cylindrical, with large vesicular nuclei, abundant pale cytoplasm, and with well-defined limits. They are disposed in solid cords, whorls, nests, islands, and border irregular pseudoglandular, cleft-like or cyst-like spaces with granular or homogeneous secretions. Fibrous cells are well-oriented, plump, and spindle-shaped and have a uniform appearance, with scant and indistinct cytoplasm and oval, dark nuclei. They form solid, compact masses with irregular nodular arrangement. A fine net of collagen fibers surrounds the single cells of the fibrous component. Mitotic figure infrequent. In type (2), spindle cells are often arranged in a herringbone or HPC-like pattern. In type (3), a pseudoglandular feature with a poorly developed spindle cells pattern prevails. In type (4), hypercellular areas with round (similar to Ewing’s sarcoma) or spindle or epithelioid cells with severe nuclear atypia and high mitotic activity.
Synovial sarcoma shows cytokeratin and/or EMA expression, although it can be quite focal and confined to only rare cells in an entire section. There is nuclear expression of TLE-1 protein. The balanced reciprocal translocation t(X;18)(p11.2;q11.2) is found in more than 95 % resulting in fusion of the SYT gene on chromosome 18 with the SSX1, SSX2, or rarely SSX4 gene on the X chromosome.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree