Fig. 11.1
Orientation of the rectal probe. The probe is placed in the distal part of the ampulla; the anterior side is indicated by the vagina (arrows) and rectovaginal septum in women (a) and by the prostate (P) in men (b). In this 3D scan, the seminal vesicle (SV), urethra (U), and bladder (B) are seen anteriorly
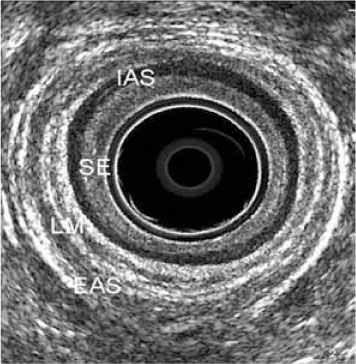
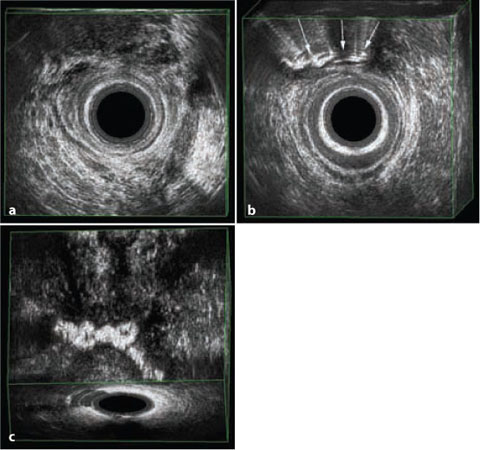
Fig. 11.2
The anal sphincter complex at transanal ultrasound. The internal anal sphincter (IAS) appears as a hypoechoic ring and the external anal sphincter (EAS) as a tissue of mixed echogenicity, with longitudinal muscle (LM) between them. SE subepithelial tissue
The investigation takes only a few minutes. Probes of several frequencies are available, from 2.5 to 16 MHz. The latter is preferably used to image the anal and rectal walls and the internal sphincter in particular, while the former allows the investigation of deeper lesions such as in the perirectal and perianal spaces. However, despite the value of 2D transanal ultrasound, it has several shortcomings. Images are normally produced only in the transaxial scanning plane. Scanning in the proximal-distal direction can be extended only by moving the probe further in or out of the anal canal or rectum.
Nowadays, it has become possible to obtain three-dimensional (3D) reconstructions of 2D images, which has vastly improved the usefulness and accuracy of anal endosonography [2]. With this technique, data from a series of closely spaced 2D images are combined to create a 3D image that can be freely rotated and sliced to allow the operator to extract the most information out of the data—freed from the time pressure of the examination itself. After a data set is acquired, coronal anterior-posterior (A-P) or posterior-anterior (P-A) as well as sagittal right-left (R-L) views can be selected (Fig. 11.3). The same endoprobe and multifrequency transducers used in 2D transanal ultrasound are also used in the 3D method. A 3D reconstruction is based on a large number of parallel transaxial images acquired using a special colorectal pullback mover (B&K Medical ultrasound probe type 1850). The B&K Medical pullback mover can be operated at different levels of resolution. For endoanal applications, the usual setting is 0.2-0.3 mm between adjacent transaxial images. Scanning the anal canal with these settings over a pullback distance of 35 mm typically yields 175 parallel images. These views constitute a source of information with which to further evaluate the patient. In patients with perianal fistula, both the fistula type and the extent of anal sphincter damage can be seen. The diagnosis is less dependent on one examiner, because the data can be reviewed by several specialists.
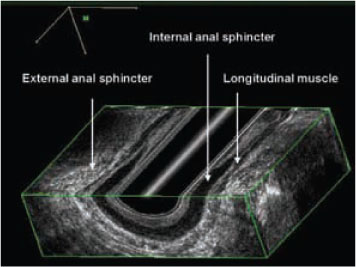
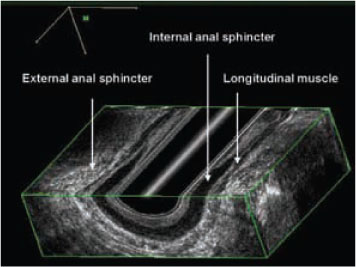
Fig. 11.3
A 3D transanal ultrasound reconstruction of the normal anorectal junction. Courtesy of Prof. Giulio A. Santoro, from [11]
Finally, the latest development is the combined use of 3D transanal ultrasound and hydrogen peroxide. If an external opening of the fistula can be identified, a flexible intravenous cannula (e.g., Venflon) can be used to introduce hydrogen peroxide into the opening immediately before a 3D data set is acquired [3], which allows better visualization of the fistulous tract. Data acquisition takes approximately 40 s for a high-resolution scan. During this short period, the hydrogen peroxide enhances the fistula tract so that it appears as a bright white structure in the ultrasound image (Fig. 11.4). Aerated and diluted lidocaine gel may also be introduced into an external opening as an ultrasound-enhancing medium. This technique is a safe, economic, and reliable procedure for the assessment of perianal fistulae [3–6]. It assists in delineating their anatomic course and is therefore of value in the planning of surgical strategies.
Get Clinical Tree app for offline access
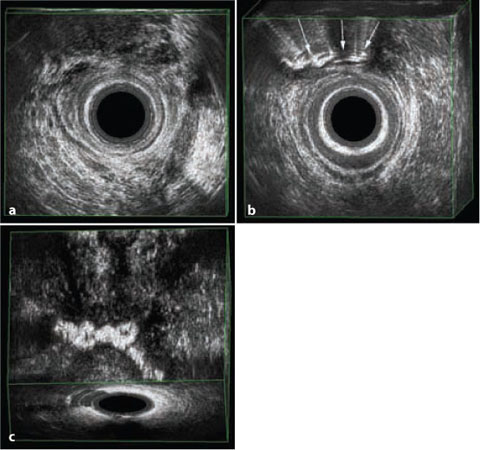
Fig. 11.4
Basal (a) and contrast-enhanced 3D transanal ultrasound (b, c




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree