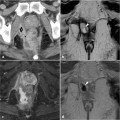
Fig. 29.1
A 55-year-old HIV-positive male patient with clinical suspicion of recurrent perianal infection following previous surgical treatment many years earlier. MRI was contraindicated because of poor patient cooperation and the presence of numerous metallic needles in both buttocks. Axial (a, b) and coronal-reformatted (c, d) images from pelvic contrast-enhanced CT provide adequate visualization of anorectal and perianal anatomic structures, without signs of abscess formation in the intersphincteric, supralevator, and ischioanal spaces
29.2 CT in the Evaluation of Perianal Disease
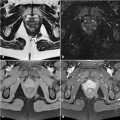
Perianal abscesses and fistulas that are filled by air or fluid can be identified on CT because of adequate contrast between their hypodense contents and the enhancing, inflamed granulation tissue present in the walls. Intrinsic CT contrast resolution limits the differentiation between different soft-tissue structures such as the pelvic muscles, active inflammatory changes, and fibrotic scar tissue (Fig. 29.2) [2, 5, 9]. Multidetector CT acquisition including routine multi- planar reconstructions enables the detection of inflammatory changes and their relationships to the anal sphincter complex and ischioanal spaces, with a reliability approaching that of MRI (Figs. 29.1, 29.2). The lower sensitivity (77%) of CT for the detection of perianal abscesses in immunosuppressed patients has been reported, probably because of a poor inflammatory response. In these patients, it is difficult to detect enhancement corresponding to active inflammation [9]. Notably, a significant limitation persists in the assessment of the thin, normal, fat-containing anovaginal and intersphincteric spaces [2, 3, 5].
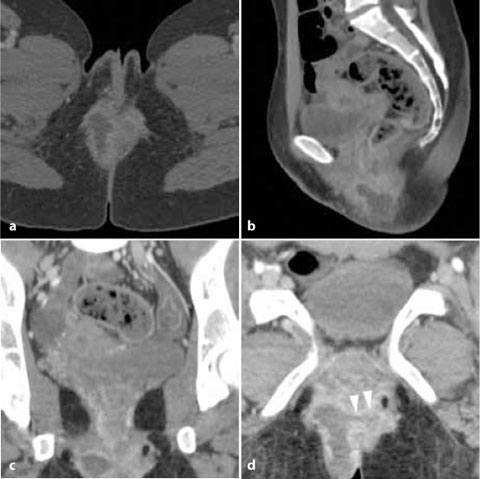
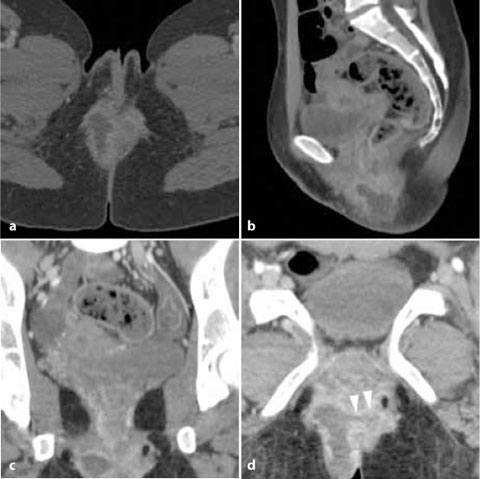
Fig. 29.2
A 27-year-old female patient with ulcerative colitis. A distal perineal abscess was detected clinically and confirmed by transperineal ultrasound. Axial (a), sagittal (b), and coronal (c) reformatted images from a contrast-enhanced volumetric MDCT acquisition visualize the entire extent of the right-sided abscess collection along three planes. The oblique reformation (d) identifies the fistulous tract with a small gas bubble, giving rise to the abscess (arrowheads)
Nonetheless, the main disadvantage of CT remains its dependence on ionizing radiation. Chronic inflammatory bowel diseases mostly affect young people, whose life expectancy will nonetheless be normal but with frequent exacerbations or complications, leading to a need for repeated diagnostic imaging studies. Therefore, patients and physicians are justifiably concerned about radiation over-exposure, with its associated increased risk of malignancy. Recently, a retrospective study addressing the total effective dose of ionizing radiation in patients with inflammatory bowel diseases over a 5-year period determined higher cumulative radiation exposure in patients with CD than in those with ulcerative colitis; some patients (7%) had been exposed to very high radiation levels (>50 mSv), the vast majority during CT scans [10




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree