How to Image the Temporomandibular Joint
See the temporomandibular joint (TMJ) protocols at the end of the chapter.
- •
Coils and patient position: Small surface coils are used, generally with a diameter of about 3 inches. Bilateral simultaneous examinations of the TMJs can be done with coupled surface coils. The patient is supine in the bore of the magnet, with the coils centered over the TMJs by centering the coils just anterior to the tragus of the ear. Images are obtained through the joints with the mouth closed. Images also can be obtained with the mouth open, which is done with a special device that holds the mouth open, or for the more innovative (cheap) among us, gauze can be wrapped around a syringe and placed in the mouth for the patient to bite down on. The size of the syringe is determined by the extent that the mouth can open.
- •
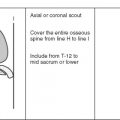
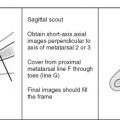
Image orientation: An axial localizer image through the TMJ condyles is obtained first. Using the axial scout image, a line is drawn between the anterior aspects of the two condyles, then sagittal images are obtained perpendicular to this line. This is essentially always the sagittal plane relative to the bore of the magnet, but is a sagittal oblique image of the TMJs. These images are obtained first with the mouth closed, and then the sagittal sequence can be repeated with the mouth open if one wishes to know if the TMJ disk reduces with mouth opening. Coronal oblique images through the TMJs are obtained as an optional sequence in some patients to show the condyles well in another plane and to show the disk in the rare event that it may displace in exclusively a medial or lateral direction relative to the condyle. These images are obtained parallel to the long axis of the condyles based on the axial scout view. Coronal oblique images are done only with the mouth closed. Our only indication for obtaining coronal oblique images is that the referring physician asks for them.
- •
Pulse sequences and regions of interest: T1W images show the pertinent anatomy well. The section thickness is 3 mm with no gap; a 6-cm field of view is used. Both TMJs generally are imaged, mainly because we have the coupled coils that allow it to be done easily, and because bilateral abnormalities are common. It is necessary only to image the symptomatic joint, however. T2W images are not necessary for evaluation of routine internal derangement, but may be valuable in patients who have had recent trauma to the joint because they may show abnormalities in the muscles surrounding the joint.
- •
Contrast: Contrast enhancement is of no value for diagnosing routine internal derangements of the TMJ.
Normal Temporomandibular Joint
OSSEOUS STRUCTURES
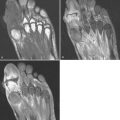
The osseous components of the TMJ are the mandibular condyle and the temporal bone at the base of the skull ( Figs. 9-1 and 9-2 ). The relevant portions of the temporal bone that articulate with the condyle are the glenoid fossa and the articular eminence. The condyle should be concentrically positioned in the glenoid fossa with the mouth closed. With the mouth open, the condyle translates anteriorly so that the condyle is positioned directly underneath the apex of the articular eminence. The articular surfaces of the TMJ are covered with a thin layer of fibrocartilage.


DISK
The soft tissue structure of interest in the TMJ is the articular meniscus or disk. The disk is interposed between the condyle and the temporal bone, completely separating the joint into superior and inferior recesses. The TMJ disk is made of fibrous tissue and has an asymmetric biconcave configuration. The disk is thicker peripherally than it is centrally. The thin central portion of the disk is called the intermediate zone . The thicker periphery of the disk is divided into anterior and posterior bands (see Figs. 9-1 and 9-2 ). The anterior band of the disk is usually smaller than the posterior band. The disk attaches to the joint capsule, pterygoid muscle, and bone. Posteriorly, the disk is continuous with collagen fibers and loose fibroelastic tissue known as the bilaminar zone or posterior attachment. The bilaminar zone functions as a rubber band, allowing the meniscus to move forward with the condyle during mouth opening, and then recoils back to its original position, bringing the disk with it, as the mouth closes.
The normal position of the TMJ disk, regardless of whether or not the mouth is open or closed, is with the thin intermediate zone interposed between the condyle and the adjacent temporal bone, wherever the two bones are most closely apposed to one another.
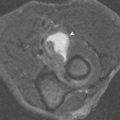
MRI of the normal TMJ in the sagittal plane shows the biconcave disk as an asymmetric bow-tie configuration. The thin intermediate zone can be seen between the two most closely apposed cortical bone surfaces of the condyle and eminence with any degree of mouth opening and with the mouth completely closed. Normally, the posterior band is located at the 12-o’clock position, directly on top of the condyle, with the mouth closed. The posterior band may not always be evident when the mouth is closed because its signal blends with the adjacent low signal intensity cortical bone of the condyle and glenoid fossa. The posterior band becomes more obvious with the mouth open, as it displaces away from adjacent bone ( Fig. 9-3 ). The disk is overall low signal intensity on all pulse sequences, but careful scrutiny shows intermediate signal intensity centrally in the anterior or posterior bands.