Temporomandibular Joint
The osseous components of the temporomandibular joint (TMJ) include the mandibular condyle, glenoid (mandibular) fossa, and, anteriorly, the articular tubercle (the bony eminence of the temporal bone). The TMJ disk is a biconcave structure, with a thick periphery and a thin center. In the sagittal plane the disk appears biconcave, in the coronal plane crescent-shaped. The anterior and posterior parts of the disk are referred to as the anterior and posterior bands. In the normal closed position, the posterior band is located at 12:00 over the condyle. In a normal joint, regardless of position (open or closed), the central thin portion of the disk remains interposed between the condyle and the articular tubercle.
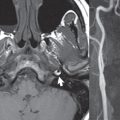
The most common internal derangement of the TMJ is disk displacement, which is usually anterior or anteromedial. Displacement (dislocation) can occur with or without reduction (the disk reverting to its normal position) on opening ( Fig. 2.84 ). A “click” heard on opening can occur due to reduction of an anterior disk displacement. In a disk displacement without reduction, the disk remains displaced anteriorly regardless of jaw position. Jaw opening may be limited, in this instance, on the affected side. Disk deformity occurs late in the disease stage, with associated degenerative bony changes including flattening of the condyle and small osteophytes. The upper and lower compartments (joint spaces, above and below the disk) normally do not communicate. TMJ arthrography is routinely performed in specialty centers, either of the lower joint space alone or of both joint spaces. CT of the TMJ is the best means of examining the osseous joint structures. On MR today, at 3T using bilateral dedicated multichannel surface coil arrays, true dynamic imaging of the TMJ can be accomplished, with a temporal resolution of one-fourth of a second. This should be supplemented by high resolution static images in both the open and closed position in the sagittal and coronal planes. Regardless of pulse sequence, the disk will have low signal intensity. T2-weighted images can also be acquired to identify abnormal joint fluid or edema in the adjacent tissues.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree