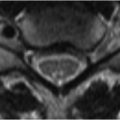
90 Temporomandibular Joint Disease The temporomandibular joint (TMJ) is a synovial joint between the mandibular condyle, glenoid fossa, and articular eminence of the temporal bone. MRI reliably evaluates joint pathology and meniscal position in most patients, with the exception of those where metallic dental hardware limits image quality secondary to susceptibility artifact. Bilateral TMJ coils are typically utilized—an important consideration given that over half of patients have bilateral dysfunction. SE T1WI are typically obtained in sagittal-oblique planes through the TMJ with both open- and closed-mouth views. FSE T2WI may be added if inflammatory disease, joint effusion, or meniscal degeneration is suspected. Coronal T1WI may be obtained to help identify meniscal displacement medially or laterally. Cine GRE images may be performed in incremental stages of mouth opening to allow for “dynamic” evaluation of joint motion. The normal appearance of the TMJ is demonstrated in the (A) closed- and (B) open-mouth FSE T1WI of Fig. 90.1. The mandibular condyle is located anterior to the external auditory meatus with its head articulating with the glenoid fossa and articular eminence of the temporal bone. The normal, biconcave meniscus is hypointense on both T1WI and T2WI. When (A) the mouth is closed, the mandibular condyle lies centered in the glenoid fossa with the meniscus (black arrow) lying along its anterosuperior aspect. With (B
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree