Testicular Varicoceles
A varicocele is a compact pack of vessels, quite filled with melancholy blood
—Ambroise Pare 1550
A varicocele is an abnormal collection of dilated veins within the spermatic venous plexus (also called the pampiniform plexus) (Fig. 14–1). This plexus sets adjacent to the testicle and epididymis and normally drains primarily into the internal spermatic vein. Drainage also occurs through the external spermatic, external pudendal, and vasal veins (Fig. 14–2). Varicoceles can be primary or secondary. Primary varicoceles are due to retrograde venous flow within the internal spermatic vein. The precise reason for this retrograde flow is not known, but the most common theory is that it is due to incompetent valves within the internal spermatic vein.1 Secondary varicoceles are extremely uncommon and are due to compression of the venous outflow of the pampiniform plexus, usually by pelvic or renal masses.2 Most varicoceles are isolated on the left, but in 7 to 23% of cases they are bilateral.3 Isolated right-sided varicoceles can occur spontaneously but are sufficiently uncommon that a patient with only a right varicocele should have an abdominal and pelvic ultrasound to exclude situs inversus or an occluding mass.
Varicoceles are not found in boys aged younger than 9 years,4 but the incidence rises at puberty and can be as high as 22.6% in some adolescent populations.5 More importantly to interventional radiologists, their reported frequency in the general adult male population ranges from 9 to 22.9% (mean reported incidence, 13.4%), but they are found in 37% of infertile men.6 A relationship between varicoceles and testicular atrophy has been known since the first century A.D.4 In 1889 Bennett7 reported improved seminal quality after surgical repair, but it was not until 1952 when Tulloch8 reported production of sperm after varicocele ligation in an azoospermic man resulting in pregnancy that more serious interest in treatment of varicoceles developed. In 1978 Lima et al9 published the first report in the English literature of percutaneous therapy for varicocele.
 Indications for Treatment
Indications for Treatment
1. Infertility: By far the most common indication for intervention in men with varicoceles, infertility is discussed in detail later in this chapter.
2. Symptomatic varicocele: Discomfort can occur as a result of engorgement or thrombosis of varicosities in the pampiniform plexus. Typically, it is perceived as a dull ache in the scrotum or groin region worsened by physical activity or long periods of standing, relieved by lying down. Groin pain is notoriously difficult to assess, and there are many causes, all of which appear to have variable and overlapping manifestations. Because of these considerations, and the fact that varicoceles are so common in the general population, it is essential that other causes of groin pain be excluded before treatment is initiated. In this setting, 89% of men report improvement or resolution of their chronic groin pain after varicocele embolisation.10
3. Adolescent varicocele: Even if asymptomatic, the presence of a varicocele in a patient aged younger than 21 years is considered by many, but not all, urologists an indication for therapy because of the likelihood of developing testicular atrophy. Compared with older patients, the reversal of preexisting testicular atrophy is more likely after treatment in this group.11
4. Cosmesis: Rarely, patients are disturbed by the appearance or feel of an otherwise asymptomatic varicocele. Ideally, these patients should be counselled as to the benign nature of the lesion; however, in some instances, this will not suffice. In my experience, neither will treatment.
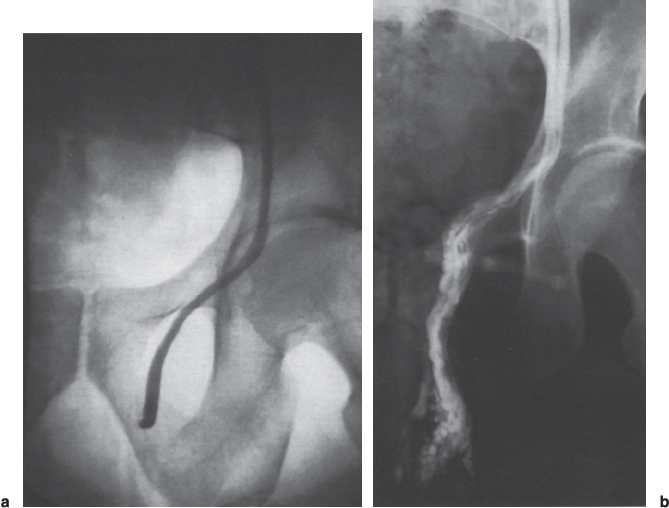
FIGURE 14–1. (a) Normal spermatic venogram. Intact valves are seen caudal to the inguinal ring, and more importantly, flow was antegrade. (b) Spermatic venogram demonstrating a varicocele. Retrograde flow opacifies dilated veins in the pampiniform plexus.
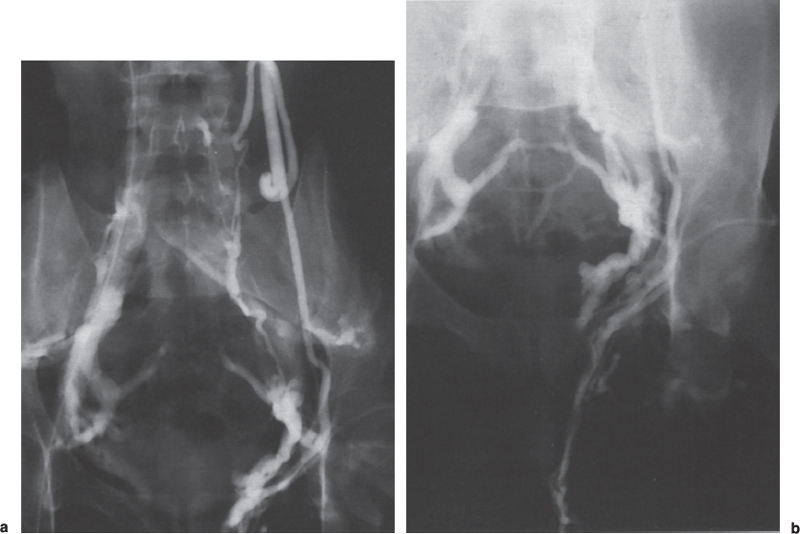
FIGURE 14–2. (a,b) Left internal spermatic venogram demonstrating collateral flow to the ascending lumbar venous system, and, after retrograde flow opacifying the pampiniform plexus, drainage of contrast via the external spermatic and the vasal veins.
 Infertility
Infertility
Background
Infertility, defined as the inability to conceive after 1 year of unprotected intercourse, affects 20 to 35% of all Western couples, and the incidence appears to be increasing.12 If the patient has never previously achieved a pregnancy with a current or any other partner, it is defined as primary infertility; if the patient has achieved previous pregnancies but has been unable to conceive after 1 year of unprotected intercourse, this is secondary infertility.
Despite the historical suspicion of the association between varicocele and male infertility, the exact nature of this relationship remains controversial. The testicle needs to be slightly lower than core body temperature to produce sperm normally,13 and therefore most researchers believe abnormal spermatogenesis in men with varicocele is due to elevated testicular temperature caused by the presence of dilated blood filled veins adjacent to the testicle or by interference with countercurrent heat exchange.14 Controversy continues on this subject, however, and other postulated mechanisms by which varicoceles cause testicular dysfunction include hormonal imbalance, hypoxia secondary to venous stasis, pressure effect on the testicle, and reflux of adrenal and renal metabolites.15
Approach to the Infertile Patient
For many couples, the inability to conceive a child may mean the dissolution of an entire life plan. Couples undergoing investigation and treatment for infertility are among the most anxious, motivated, and well-informed of patients. Therefore, any physician performing procedures to diagnose or treat fertility disorders must demonstrate compassion and respect for the patient’s privacy and sense of vulnerability and have a thorough knowledge of relevant subjects, such as semen analysis, hormonal cycles, and success of alternative fertility procedures.
Clinical Evaluation
Prior to therapy, an infertile man with a varicocele should have the benefit of consultation with an urologist or infertility specialist. It should be shown that the patient has documented infertility, that the female partner is potentially fertile, and that the patient has appropriate abnormalities of semen parameters. Evaluation should include a careful history that includes wearing tight underwear, taking hot baths, or sleeping on waterbeds, and physical examination to exclude other causes of infertility should be performed.
Varicoceles can be diagnosed by physical examination; however, nonpalpable varicoceles, also called subclinical varicoceles in the urologic literature, constitute approximately 44% of all varicoceles.16 Right-sided varicoceles are more commonly subclinical than left. The examination should be done in both the recumbent and upright positions to maximize palpation of a fluctuant serpiginous “bag of worms” adjacent to the testicle. The patient should be asked to cough and a Valsalva maneuver performed to generate a regurgitant venous thrill. The standard clinical grading system is grade I, varicocele palpable only during Valsalva maneuver; grade II, varicocele palpable without Valsalva maneuver; and grade III, varicocele visible.
Semen Analysis
Normal semen is an admixture of spermatozoa suspended in secretions from the testis and epididymis mixed, at the time of ejaculation, with secretions from the prostate, seminal vesicles, and bulbourethral glands. The final composition is a viscous fluid that constitutes the ejaculate. Varicoceles cause various combinations of low total sperm count, diminished sperm motility, or increased production of abnormal forms; this variable pattern is known as a stress pattern. This condition is evaluated by microscopic examination of the semen. At least two samples should be collected for pretreatment and posttreatment evaluations. If the results of any two assessments differ markedly, additional samples should be examined because any individual man’s sperm output can vary considerably.17 Analysis should include total count, motility, and number of abnormal forms.
The collection and analysis of semen must be undertaken by properly standardized procedures if the results are to provide valid information on the fertility of the individual patient. Ideally, the sample should be collected after a minimum of 48 hours but not after longer than 7 days of sexual abstinence. The specimen should be delivered to the laboratory within 1 hour of collection. The sample should be obtained by masturbation and ejaculated into a clean, widemouth container made of glass or plastic. The container should be warm to minimize the risk of cold shock. Ordinary condoms must not be used for semen collection because they can interfere with the viability of spermatozoa. Ideally, all pretreatment and posttreatment specimens will be examined in the same laboratory. The laboratory handling an examination of the sperm should be in the manner recommended by the WHO Laboratory Manual for the Examination of Human Semen and Sperm—Cervical Mucous Interaction.18
Scrotal Ultrasound
Sonographic examination should be performed in all men with unexplained infertility and appropriate semen abnormalities. In addition to assessment of the veins of the pampiniform plexus, comment should be made on testicular volume, the presence of dystrophic changes within the testicle, and abnormalities of the epididymis/vas complex such as cystic changes.
A varicocele is considered present when abnormally dilated veins are detected within the pampiniform plexus or when there is abnormal accentuation of flow with coughing or Valsalva manoeuvre. The literature has been ambiguous regarding the criteria for ultrasound diagnosis of varicocele and even for the proper method of detection. When scanning with grey-scale ultrasound alone, the presence of at least three veins greater than 3.0 mm in diameter is considered to constitute a varicocele19 by some, whereas others consider vessels greater than 2.0 mm abnormal.20 When duplex scanning is added, the detection of accentuated flow with Valsalva maneuver in vessels greater than 2.0 mm improves sensitivity, but it also may cause false-positive results.21–22
In our practice, we examine the patient in the upright position after 15 minutes of standing, in both quiet respiration and Valsalva maneuver using grey-scale and color duplex. If the patient is unable to perform a Valsalva maneuver, we will have the patient cough, although the examination is more difficult because of motion artifact. We classify the examination as normal if no veins in the pampiniform plexus are larger than 1.5 mm in diameter and there is normal accentuation of flow with Valsalva maneuver or coughing and as definite for varicocele if veins greater than 2 mm in diameter are present and there is abnormally brisk and prolonged accentuation of flow with Valsalva maneuver or coughing. We categorize all other combinations of findings “equivocal—requires spermatic venography to assess.”
 Spermatic Venography and Varicocele Embolization
Spermatic Venography and Varicocele Embolization
Indications for Spermatic Venography and Varicocele Embolization
The gold standard for diagnosis of varicocele is the demonstration of retrograde flow within the spermatic vein extending into the pampiniform plexus (see Fig. 14–1). In addition to those listed previously for treatment of varicocele, the indications for selective catheterisation of the spermatic vein include clarification of the diagnosis when noninvasive or clinical examinations are inconclusive or contradictory and recurrent or persistent varicoceles after surgical or embolic treatment (Table 14–1, Fig. 14–3).23
Contraindications to Spermatic Venography and Varicocele Embolization
Contraindications include the following:
• Allergy to iodinated contrast
• Disorder, such as renal failure, predisposing to complication from contrast administration or vascular catheter insertion
• Venous anatomy such that there is no absolute assurance of the embolic agent remaining within the spermatic vein once it has been deployed
• Primary disorder of semen production, for example, generation of spermatazoa without heads
Severe needle phobias or phobias to foreign bodies are relative contraindications.
It is important to remember that these men have a lifestyle problem, not a life-threatening illness; they tend to be young, healthy patients. Although it has disadvantages relative to embolization, surgery is a viable option for most men with varicocele. Therefore, the approach to these patients should be conservative compared with application of interventional techniques to other disorders.
Patients in Whom Varicocele Repair Is Less Likely to Be of Benefit
Factors that decrease the likelihood of pregnancy after spermatic vein interruption include the following24–26:
• Noncorrectable infertility in the female partner
• Significant testicular atrophic or dystrophic changes on ultrasound
• Advanced age
• Total sperm count of less than 10 million/mL
• Sperm densities greater than 40 million/mL
Infertility in man with appropriate semen abnormalities Symptomatic varicocele Adolescent varicocele Cosmesis Varicocele recurrent after treatment Diagnosis Discordance between clinical exam and ultrasound Equivocal scrotal ultrasound Unexplained infertility and appropriate semen abnormalities |
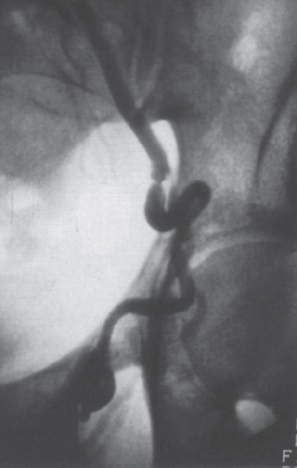
FIGURE 14–3. Varicocele recurrent after surgical ligation. A focal stenosis in the vein at the site of the failed ligature is seen. More often, no evidence of previous surgery is seen.
If a patient has any of these factors, he should be advised that the prospects for improvement after treatment are limited, and the couple might want to consider assisted-fertility techniques, particularly if the female partner is older than 37 years. Because it takes between 6 weeks and 6 months for any measurable increase in sperm quality to occur, performing an embolization might delay and even decrease the success of a therapy more likely to succeed in this clinical situation.
Informed Consent
Ideally, informed consent is obtained with the female partner in attendance. Within practical limits, I try to have scrotal ultrasound performed on these patients at a separate session and to use this as an opportunity to establish rapport as well as obtain consent. This includes reinforcement of the fact that this healthy patient is likely to receive multiple permanently implanted devices. In addition to the specifics of the procedure, other issues that require discussion at time of informed consent include the following topics.
Alternative Methods of Treatment
No Corrective Therapy
The patient should be made aware that because of the high frequency of varicocele in the general population and variability in treatment results described in the literature, there has been some debate as to the efficacy and relevance of varicocele obliteration for infertility. After reviewing all the pertinent literature between 1954 and 1994, Schlesinger et al27 concluded that there is a real improvement in fertility after correction of varicocele when performed for appropriate indications. It also appears that in infertile men, further deterioration of fertility potential is prevented. The average pregnancy rate achieved was 32.24%. Conversely, Nieschlage et al28 in a small prospective series reported no difference between counselling, surgical occlusion, or angiographic occlusion of the spermatic vein after 1 year of follow-up.28 Although cooling the scrotum with specially designed underwear incorporating an irrigation system also has been described29
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree