- •
Large malalignment type of ventricular septal defect
- •
Large overriding aorta
- •
Rudimentary, primitive pulmonary valve tissue with both stenosis and severe insufficiency
- •
Massively dilated, aneurysmal proximal branch pulmonary arteries
- •
Dilated right ventricular outflow tract and right ventricle
- •
Right ventricular systolic dysfunction, possible
- •
Absence of the ductus arteriosus (unless rare case of discontinuous left pulmonary artery arising from ductus arteriosus)
Anatomy and Anatomical Associations
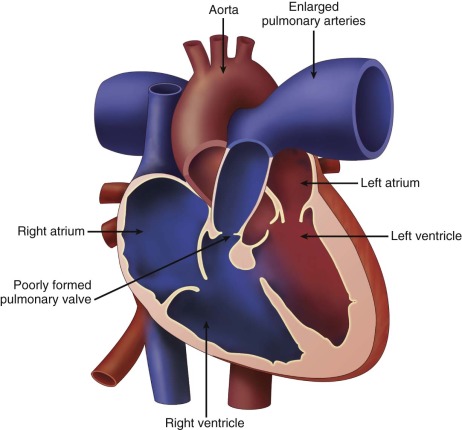
Tetralogy of Fallot with absent pulmonary valve syndrome (TOF/APVS) is a rare variant of tetralogy of Fallot (TOF) in which the pulmonary valve leaflets are extremely underdeveloped resulting in severe pulmonary insufficiency and aneurysmal dilation of the main and branch pulmonary arteries. The entity of absent pulmonary valve leaflet syndrome can exist in association with an intact ventricular septum, but is discussed elsewhere. In TOF/APVS, a large malalignment ventricular septal defect (VSD) is present, as well as an overriding aorta, and some degree of pulmonary stenosis. Malalignment of the conal septum may be difficult to appreciate because of the right ventricle, subpulmonary, infundibular, and pulmonary artery dilation. In the position of the pulmonary valve annulus, there is a thickened gelatinous ring of tissue that gives rise to very abnormal rudimentary leaflets. The pulmonary valve annulus is usually hypoplastic, but not to the same degree as seen in standard TOF. The pulmonary valve is completely incompetent, resulting in severe pulmonary insufficiency. The main pulmonary artery and branch pulmonary arteries are markedly dilated ( Figure 12-1 ). Because the branch pulmonary arteries are adjacent to the airways, these vessels can cause significant compression of the bronchi. In addition, studies have shown that the pulmonary arterioles in TOF/APVS exhibit peculiar branching patterns with dilated proximal and hypoplastic distal vessels in addition to the appearance of coiling. The abnormal vessels further cause impingement on the intraparenchymal bronchi and inhibit alveolar growth. The right ventricle is markedly dilated, and tricuspid regurgitation is common related to annular dilation. The ductus arteriosus is almost always absent in TOF/APVS, except in rare cases in which there is discontinuity between the pulmonary arteries and the ductus arteriosus connects to a discontinuous left pulmonary artery.
TOF/APVS has been associated with several other cardiac abnormalities, including anomalous origin of the branch pulmonary arteries, coarctation of the aorta, and total anomalous pulmonary venous return.
Frequency, Genetics, and Development
TOF/APVS accounts for approximately 3% to 6% of all cases of TOF. Limited data are available in the literature regarding the genetic etiology. Microdeletion of chromosome 22q11, which is present in 90% of patients with DiGeorge syndrome, is identified in 21% to 38% of patients with TOF/APVS without any specific correlation to aortic arch sidedness. Sporadic cases of other chromosome abnormalities have been reported in the literature, although these are more common in the presence of absent pulmonary valve with an intact ventricular septum.
Two main theories exist regarding the developmental abnormality resulting in TOF/APVS. In the first, because the pulmonary valve is always structurally very abnormal in this disorder, it suggests an original primary error in signaling leading to improper formation of the pulmonary valve and severe pulmonary insufficiency. If a ductus arteriosus were to be present, survival would not be possible according to this argument. The presence of a ductus arteriosus in the fetus with severe pulmonary insufficiency would seriously affect systemic perfusion because flow through such a ductus arteriosus would be retrograde, stealing from the systemic circulation and becoming part of the regurgitant flow across the pulmonary valve. It is believed that in such a scenario, fetuses suffer early demise, which may explain why a ductus arteriosus is almost always absent in TOF/APVS. A second proposed theory suggests that congenital agenesis of the ductus arteriosus is primary, which in the presence of a select group of susceptible TOF, results in altered pulmonary artery flow hemodynamics and impairs normal development of the pulmonary valve and pulmonary arteries.
Increased nuchal translucency in the first trimester has been noted in 40% of fetuses with TOF/APVS without a specific association with chromosomal abnormalities.
Fetal Physiology
Regardless of the events prompting abnormal pulmonary valve formation and absence of the ductus arteriosus, the prenatal manifestations of TOF/APVS pertain to severe pulmonary insufficiency, right ventricular dilation, and markedly dilated pulmonary arteries. In the setting of severe pulmonary insufficiency, stroke volume from the right ventricle is elevated with potential progression to right ventricular dysfunction. Moreover, in the absence of a ductus arteriosus, blood ejected out of the right ventricle is fully delivered to the pulmonary circulation and the pulmonary arteries must withstand significant increases of blood volume. Progression of pulmonary artery dilation from mid to late gestation has been documented, suggesting that vascular remodeling is a dynamic process in this anomaly. Both left and right ventricular dysfunction can be impaired in the fetus, based on qualitative inspection of systolic shortening and measures of myocardial performance index and Doppler flow reversal in the umbilical artery. The prenatal course is not based on the pulmonary aspect of the disease, but on the cardiac aspects, and in particular, the impact of severe pulmonary insufficiency on right ventricular performance. Because there is a large VSD, progressive volume loading of the right ventricle will ultimately affect the left ventricle as well. There is a high prevalence of fetal demise in TOF/APVS, which is associated with preceding fetal hydrops.
Fetal lung development, both vascular and airway, is abnormal and related to a combination of bronchi compression from dilated pulmonary arteries and right ventricle, as well as inhibition of appropriate alveolar multiplication related to aberrant branching patterns of the bronchioles.
Prenatal Management
Fetuses with TOF/APVS have a high incidence of fetal demise, but to date, there are no available prenatal interventions to improve outcomes. Serial echocardiography should be performed in all fetuses to assess for signs of ventricular failure and hydrops, although the options are limited unless the fetus is near term and delivery can be performed safely. Counseling with families should include the possibility of fetal demise as well as the risk of abnormal lung development and airway compromise, which can affect postnatal prognosis. Unfortunately, neither the degree of pulmonary insufficiency nor any other variables have been found to prognosticate for the degree of lung disease present in the fetus with TOF/APVS. Each fetus should undergo a comprehensive obstetrical fetal anatomy ultrasound, and karyotype evaluation is strongly recommended.
Postnatal Physiology
The clinical presentation of fetuses that survive to term is variable. Upon delivery, the pulmonary vascular resistance decreases after the infant takes the first breath. A drop in pulmonary vascular resistance may promote forward flow into the pulmonary arteries, achieving adequate levels of oxygenation. The pulmonary annular hypoplasia is generally not significant enough to cause severe right ventricular outflow obstruction. In the absence of respiratory symptoms related to lung disease, these infants will follow a clinical course similar to standard TOF and undergo elective surgical repair before 6 months of age. However, approximately half of newborns with TOF/APVS present with severe respiratory symptoms due to either compression of the bronchi from the severely dilated pulmonary arteries or abnormal alveolar development. These infants can be quite ill and may require urgent surgical intervention.
The physical examination reveals varying levels of hypoxemia and often tachypnea and respiratory distress. A prominent “to-and-fro” murmur is appreciated along the left sternal border, representing a harsh systolic component due to flow across the hypoplastic pulmonary annulus (and increased stroke volume) and a low-pitched diastolic component representing insufficiency. Hepatic enlargement may be present in the setting of right ventricular dysfunction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








