CHAPTER 102 The Abdominal Aorta
TECHNIQUES
CT Techniques
Using MDCT, a helical volume is acquired with a detector collimation of between 0.5 and 1.5 mm, and reconstructed with a similar thickness using a matrix size of 512 × 512 or greater. The use of tube current modulation techniques (e.g., automated exposure control) reduces radiation exposure compared to fixed-tube current techniques. For MDCT angiography, increased vascular enhancement can be achieved by reducing the kVp to 100 keV (or 80 keV in smaller patients) because this increases photon attenuation by iodinated contrast and moves the mean energy closer to the k-edge of iodine (33.2).1
MRI Techniques
Coils and Patient Position
MR Pulse Sequences
Precontrast Sequences
Steady-State Free Precession: Steady-state free precession sequences (also termed balanced-FFE, true-FISP, and FIESTA) are rapid, have high intrinsic contrast resolution, and have been shown to be accurate in evaluating renal artery stenosis,2 aneurysm sac contents (Figure 102-1),3 thoracic aortic dissection, and aneurysm.4 These sequences can be performed with breath-hold techniques or free breathing with navigator gating, and they provide an overview of the aneurysm sac and surrounding contents.
CONTRAST MEDIA
Contrast Media Dose
For abdominal aortic CTA, doses of up to 150 mL of nonionic contrast delivered at 3 to 6 mL per second have been routinely used in the past. However, with rapid acquisition techniques, doses as low as 50 mLs have been used, especially in smaller patients.5 For MRA, a typical gadolinium-chelate contrast agent dose is 0.2 mmol/kg injected at 2 mL/sec.
MRA: K-Space
By using time-resolved magnetic resonance imaging (TR-MRA) techniques, the dynamics of blood flow in the abdominal vessels can be demonstrated in a way similar to conventional angiography. In TR-MRA, there is over-sampling of central k-space, which is acquired every 2 to 8 seconds for 1 to 3 minutes after gadolinium injection, without the need of a timing bolus. Time-resolved MRA has been shown to be an effective means of classifying endoleaks following endovascular repair.6
ABDOMINAL AORTIC ANEURYSM
Abdominal aortic aneurysm (AAA) is enlargement of the abdominal aorta above a diameter of 3 cm.7
Prevalence and Epidemiology
Abdominal aortic aneurysms are nearly five times more common in men than in women and almost twice as common in people of European descent than African Americans. The prevalence of aneurysm is also increased in those with a family history of AAA, and is strongly related to a history of smoking.8 Other risk factors include age, coronary artery disease or another manifestation of atherosclerosis, high cholesterol, and hypertension. In a large ultrasound screening study,9 an abdominal aortic aneurysm was detected in approximately 5% of males older than 65 years. Ruptured AAA occurs in 1% to 3% of men per year aged 65 years or more, and mortality is 70% to 95%. Left untreated, AAA leads to death in about one third of patients.8
Etiology and Pathophysiology
Although the exact etiology of AAA remains unclear, it appears that degradation of elastin, collagen, and other structural proteins in the aortic wall is a major factor.10 Atherosclerosis is considered to play an important role in the etiology, likely via chronic inflammation in the aortic wall. An imbalance of T-helper and T-suppressor lymphocytes leads to a proliferation of B-lymphocytes. Elastin-derived peptides (EDPs), which are breakdown products of medial elastin, are thought to be the initiating and propagating antigen in this process. Chronic inflammation leads to excess matrix metalloproteinases and degradation of medial elastin and collagen.11 However, the etiology is unquestionably multifactorial. Current research suggests that genetic, environmental, hemodynamic, and immunologic factors all contribute to the development of aneurysms.
Clinical Manifestations of Disease
Most AAAs are asymptomatic and are discovered incidentally on routine physical examination or during other imaging studies. Patients with ruptured AAAs often present with an abrupt onset of back pain as well as abdominal pain and tenderness. Patients may present critically ill. Most will have a pulsatile abdominal mass. Rupture has a high mortality rate, with 25% mortality prior to arriving at the hospital and an overall 30-day survival rate of approximately 10%.12
The rate of aneurysm growth increases with increasing diameter in concordance with Laplace law. Aneurysms smaller than 4 cm grow at 2 to 4 mm/year, those measuring 4 to 5 cm grow at 2 to 5 mm per year, and aneurysms >5 cm grow at 3 to 7 mm per year.13 The risk of rupture increases with aneurysm size and rate of aneurysm expansion. In the U.K. Small Aneurysm Trial,14 aneurysms with a cross-sectional diameter of 5 to 5.9 cm in size had an annual risk of rupture of 6.5%. Elective AAA repair carries a 4% to 6% mortality. Recommendations10 suggest elective repair of aneurysms greater than 5.5 cm in males, and greater than 4.5 to 5 cm in women. Aneurysm length is not thought to be associated with rupture risk.15
Imaging Indications and Algorithm
The U.S. Preventive Services Task Force (USPSTF)16 recommends screening for AAA in men aged 65 to 75 years of age who have ever smoked. It can also be considered in patients with a strong family history of AAA. Ultrasound is the modality of choice for screening in most patients. Its advantages include the absence of intravenous contrast, absence of ionizing radiation, and relatively low cost.
For asymptomatic and smaller aneurysms, ultrasound surveillance is recommended (Table 102-1). For aneurysms >4.5 cm, CT or MRI offer the advantages of greater measurement accuracy, better depiction of the suprarenal aorta and branch vessels, and superior reproducibility versus ultrasonography.
TABLE 102-1 Rescreening Intervals for Asymptomatic AAAs
| Diameter up to | Re-image aorta in |
|---|---|
| <3.5 cm | 3 years |
| <4.0 cm | 2 years |
| <4.5 cm | 1 year |
| <5 cm | 6 months |
| 5-5.5 cm | 3-6 months* |
* Also consider referral to a vascular surgeon.
Derived from Isselbacher EM. Thoracic and abdominal aortic aneurysms. Circulation 2005; 111(6):816-828.
Imaging Techniques and Findings
Radiography
The presence of calcification in the abdominal aortic wall, although commonly present, is not invariable. Moreover, a tortuous and calcified aorta may mimic an AAA. A lateral radiograph (Fig. 102-2) may depict aortic calcification more clearly. However, radiographs are unreliable for diameter measurements of the aortic wall and are not recommended for diagnosis or surveillance.17
Ultrasonography
Examination of the abdominal aorta is an essential component of a complete abdominal ultrasound study, and should be examined in all patients presenting with acute abdominal pain. Abdominal aortic aneurysms should be detectable by sonography in up to 100% of patients.18
The aorta appears on ultrasound as a hypoechoic tubular structure with echogenic walls (Fig. 102-3A). The anterior and posterior walls of the aneurysm are usually better seen than are the lateral walls. Mural thrombus (see Fig. 102-3B) has low to medium echogenicity and is attached to the margins of the aortic wall. At times, mural thrombus will have a lamellated appearance. Thrombus that appears to “flutter” during the cardiac cycle may be at risk of embolization.
In suspected aneurysm rupture, a bedside ultrasonogram may be helpful for those patients who are too unstable for CT, or if CT is not readily available. Ultrasound scanning may assist in determining the aneurysm size and the presence of retroperitoneal or intraperitoneal fluid (Fig. 102-4), although the role of ultrasonography in identifying impending rupture is limited.19
CT and MRI
Compared to ultrasonography, CT and MRI (Fig. 102-5) provide superior depiction of the extent and shape of the aneurysm, involvement of the renal, mesenteric, and iliac arteries, and the suprarenal abdominal and thoracic aorta. On average, ultrasound underestimates aneurysm size by 3 to 9 mm compared to CT angiography.20 Due to their excellent contrast resolution and multiplanar capabilities, CT and MR angiography are now the mainstay of aneurysm characterization prior to endovascular or surgical repair. CT is the modality of choice for the evaluation of suspected rupture of the abdominal aorta19; usually it can be performed within minutes, and has clear benefits in showing alternative causes of acute abdominal pain. Contrast-enhanced CT provides information about the lumen size, location, extent, relationship to branch vessels, presence of active contrast extravasation, and complications secondary to aneurysm rupture.
Signs of Rupture, Impending Rupture, and Contained Rupture
Noncontrast CT is useful in demonstrating the presence of an abdominal aortic aneurysm, maximum aneurysm size, and the presence of retroperitoneal hemorrhage. A high attenuating crescent within the wall of aneurysm (Figs. 102-6 and 102-7) is a sign of impending or frank aneurysm rupture.21 A high attenuation crescent is denser than the psoas muscles (on enhanced CT) and the lumen (on nonenhanced CT scans).
The most common finding in aneurysm rupture is a retroperitoneal hematoma adjacent to the abdominal aortic aneurysm (see Figs. 102-4, 102-7, and 102-8). This blood usually tracks into the pararenal and perirenal spaces (Fig. 102-9). Active extravasation (Figs. 102-9 and 102-10) is frequently visualized on contrast-enhanced CT images. The “draped aorta sign,” where the abdominal aorta is closely applied to the spine with lateral “draping” of the aneurysm around the vertebral body (see Fig. 102-4), has been described as a finding of a deficient posterior wall of the aorta and a contained leak.22 Other sites of rupture include the bowel (most commonly the duodenum), and inferior vena cava (Fig. 102-11).23 Signs of AAA rupture, impending rupture, and contained rupture are (1) periaortic and retroperitoneal hemorrhage; (2) contrast extravasation; (3) high attenuating crescent sign; and (4) draped aorta sign.
FDG-PET
Recent evidence suggests that increased aortic wall metabolism, as measured by FDG-PET, may suggest increased rupture risk. Increased metabolism may represent increased activation of inflammatory cells in the aortic wall, which leads to increased degradation of elastin and collagen in the aneurysm wall.24 Pilot studies examining the role of FDG-PET-CT in asymptomatic and symptomatic AAAs,25 have demonstrated increased activity in those with symptomatic AAAs, and increased activity in focal areas of increased inflammation and collagen degradation.
Treatment Options
Medical
Medical therapy is usually instituted in patients with smaller aneurysms not treated surgically or endovascularly. Smoking cessation is paramount because smoking plays a major role in aneurysm growth.26,27 Although the effect of hypertension and dyslipidemia on aneurysm growth and rupture are unknown, treating these conditions may prolong survival. Statin therapy has been shown to reduce mortality and slow aneurysm growth.26 β-blockers may slow the expansion rate of aneurysms.28
INFLAMMATORY AORTIC ANEURYSM
Definition
Inflammatory abdominal aortic aneurysms are defined by the presence of a thickened aneurysm wall, marked peri-aneurysmal and retroperitoneal fibrosis, and dense adhesions of adjacent abdominal organs.11
Prevalence and Epidemiology
IAAAs constitute approximately 3% to 10% of abdominal aortic aneurysms. Male sex and smoking are both strong risk factors, with a male-to-female ratio ranging from 6 : 1 to 30 : 1. From 77% to 100% of patients smoke.11 Other risk factors include northern European descent and autoimmune disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


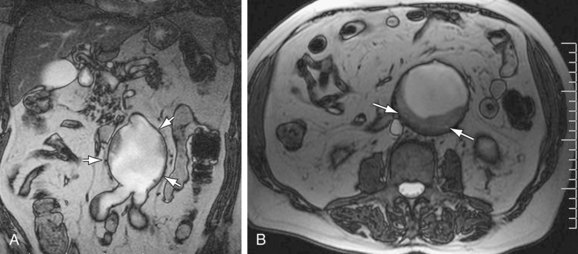
 Figure 102-1
Figure 102-1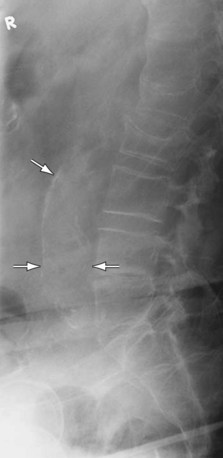
 Figure 102-2
Figure 102-2
 Figure 102-3
Figure 102-3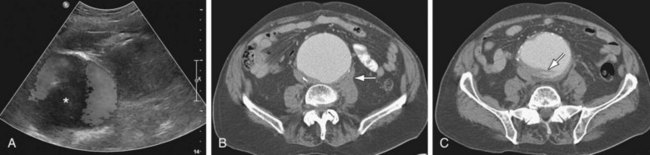
 Figure 102-4
Figure 102-4
 Figure 102-5
Figure 102-5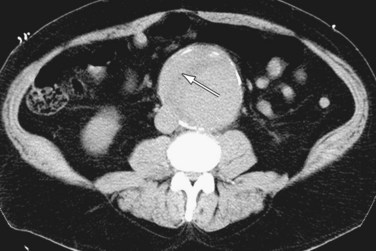
 Figure 102-6
Figure 102-6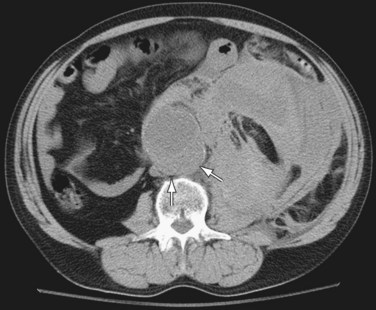
 Figure 102-7
Figure 102-7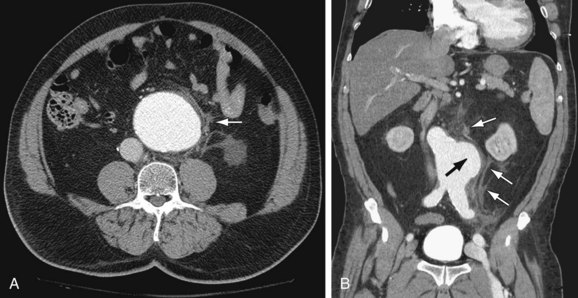
 Figure 102-8
Figure 102-8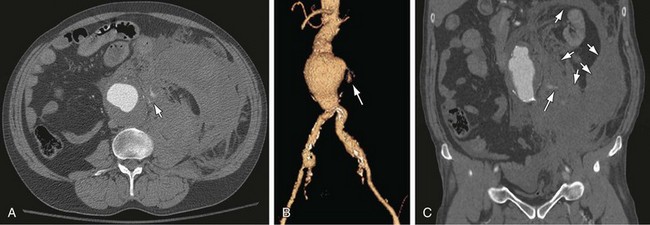
 Figure 102-9
Figure 102-9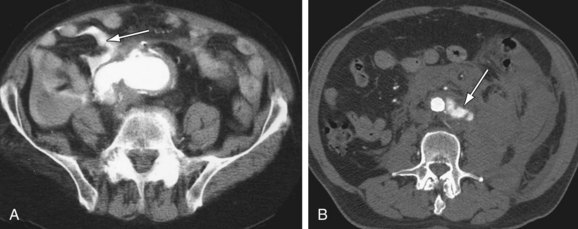
 Figure 102-10
Figure 102-10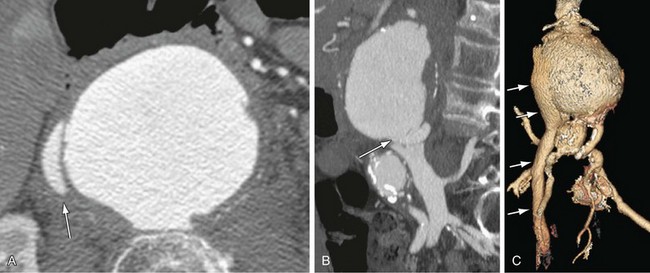
 Figure 102-11
Figure 102-11