Key Points
- ▪
The abdominal aorta is principally subject to aneurysmal disease in its infrarenal portion, to occlusive disease in its distal portion, and to dissection extending from thoracic aortic dissection.
- ▪
However, variations to these syndromes and other disorders such as aortitis, as well as concurrent branch vessel disease, confer a broad spectrum of abdominal aortic disease.
Anatomy of the Abdominal Aorta
The abdominal aorta begins at the level of the diaphragm and runs along the anterior longitudinal ligament in front of the vertebral column slightly to the left of both midline and inferior vena cava. As a result of the many branch vessels given off along its course, the aorta diminishes in size as it descends to the bifurcation. Because it lies in front of the convex-shaped vertebrae, it too is slightly curved, with the apex at the level of the third vertebra.
The branches of the aorta are divided into three sets:
- □
Visceral
- •
Celiac
- •
Superior mesenteric
- •
Inferior mesenteric
- •
Renal (paired)
- •
Middle adrenal (paired)
- •
Internal spermatic (male) (paired)
- •
Ovarian (female) (paired)
- •
- □
Parietal-inferior phrenic (paired)
- •
Middle sacral
- •
Lumbar (paired)
- •
- □
Terminal—common iliac artery (paired)
The celiac artery (axis) is a 1.25-cm long stumpy artery arising from the anterior aspect of the aorta immediately below the diaphragm. The celiac artery divides into the left gastric, splenic, and common hepatic arteries, which supply the spleen, liver, stomach, duodenum, and pancreas.
The superior mesenteric artery, a large artery, arises from the aorta approximately 1.25 cm distal to the celiac artery, supplies the whole of the small intestine, cecum, head of the pancreas, ascending colon, and half of the transverse colon. The superior mesenteric artery lies behind the pancreas where the splenic vein crosses over its proximal segment and then courses downward and forward, crossing in front of the inferior vena cava, diminishing in size to its terminus and anastomosis with one of its own branches, the ileal branch of the ileocolic artery. There are 12 to 15 branches that run down the left side of the superior mesenteric artery, divide, and then anastomose with adjacent branches to form a series of arches supplying the small intestine.
The middle, right, and ileocolic arteries arise from the right side of the superior mesenteric artery. Of particular note is the middle colic artery, which forms an anastomosis with the left colic branch of the inferior mesenteric artery to create the marginal artery, an important collateral in the presence of celiac artery occlusive disease.
The inferior mesenteric artery is smaller than the superior mesenteric artery, arising from the anterior aspect of the aorta approximately 3 cm proximal to the aortic bifurcation at the level of the third lumbar vertebra. This artery supplies the left half of the transverse colon, a greater part of the rectum, and the descending colon.
The inferior mesenteric artery lies anterior to the aorta and then runs downward on the left side, eventually crossing the left common iliac artery. After this point it continues as the superior rectal hemorrhoidal artery, an important stem artery that joins with other hemorrhoidal branches to provide a collateral network in cases of aortic obstruction.
The suprarenal arteries arise from either side of the aorta at the level of the superior mesenteric artery. They run laterally and proximally where they pass over the crura of the diaphragm to join with suprarenal branches of the renal and inferior phrenic arteries.
The lumbar arteries are a series of four paired vessels that arise from the back of the spine, passing behind the quadratus lumborum and psoas muscles. There they join with other arteries in the area and can provide collaterals as far away as the inguinal ligament.
Similarly, the subcostal arteries (intercostal arteries of the twelfth rib) can supply important collaterals in the presence of aortoiliac artery occlusion. The third lumbar artery is the most common source of collateral blood supply in the presence of renal artery stenosis or occlusion.
- ▪
A bowel “prep” is recommended before performing abdominal (vascular) ultrasound for patients who do not have diabetes:
- ▪
Low-fat meal night before
- ▪
Plenty of clear fluids throughout with medications, if necessary
- ▪
No gum chewing, caffeine, or carbonated beverages
- ▪
Bowl of flavored gelatin the morning of the test (helps abate the appetite and reduces excessive aerophagia)
- ▪
- ▪
The waveforms in the aorta vary in shape between the proximal and distal segments:
- ▪
Relatively low resistance proximal flow patterns are influenced by the low-resistance end bed of the renal and celiac arteries.
- ▪
In contrast, flow patterns in the higher resistance infrarenal segment are shaped by the high resistance of the lumbar, peripheral arteries, and (non-postprandial) superior and inferior mesenteric arteries.
- ▪
- ▪
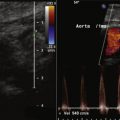
Use a small color box when imaging for endoleaks.
- ▪
Optimize settings so that the color gain is set just below speckle, then circle the circumference of the sac carefully to search for any evidence of flow within the sac or connecting channel of flow.
The internal spermatic arteries arising from the anterior aorta just below the renal arteries are small. In contrast, the paired ovarian arteries are large and join in an arcade with the uterine arteries, which are part of the internal iliac artery system.
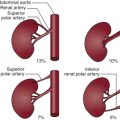
The renal arteries arise from the aorta at approximately the level of the second lumbar vertebra immediately below the superior mesenteric artery, although some variation is known. Major accessory renal arteries are usually fewer than two or three in number and most commonly arise from the aorta, but smaller arteries can originate from vessels such as the suprarenal artery. Approximately 50% of these accessory arteries extend to the hilum and the other 50% to either the upper or lower poles of the kidney.
As both renal arteries cross the crura of the diaphragm, they almost form a right angle with the aorta. The left renal artery extends superior and posterior to the left renal vein and inferior and posterior to the pancreas and splenic vein. The right renal artery is longer than the left renal artery and passes behind the inferior vena cava, right renal vein, head of the pancreas, and descending segment of the duodenum.
Before entering the hilum of the kidney, each renal artery gives off four or five branches, which extend to the adrenal gland, ureter, muscle, and neighboring tissue. Closer still to the hilum, the anterior and posterior segmental, or lobar, arteries arise and supply the various segments of the kidney.
The segmental arteries further divide into the interlobar arteries, which run alongside the renal pyramids
| ANATOMIC SEGMENT | TECHNIQUE | DUPLEX MODALITY |
|---|---|---|
| Aorta | SAX sweep Proximal Mid Distal | Grayscale, color Doppler |
| LAX Proximal Mid Distal | Grayscale, color/spectral Doppler | |
| Common iliac artery | SAX sweep Proximal Mid Distal | Grayscale |
| LAX sweep Proximal Mid Distal | Grayscale, color/spectral Doppler | |
| Internal iliac artery | SAX | Grayscale, color Doppler |
| LAX | Grayscale, color/spectral Doppler | |
| External iliac artery | SAX | Grayscale |
| LAX sweep Proximal Mid Distal | Grayscale, color/spectral Doppler |
Besides the third lumbar artery previously mentioned, the collateral circulation for the kidney is usually provided by the internal iliac, testicular, ovarian, intercostal, and inferior adrenal arteries, and the first three lumbar arteries are the main supply for an ischemic kidney.
Aneurysmal Disease of the Abdominal Aorta
Abdominal aortic aneurysms (AAAs) are common in the older population, in 3.5% of males older than 65 years of age (although most of these are small), and the incidence increases with increasing age. Unfortunately, the same is true with obesity, which is increasingly common and severe with aging. AAAs occurring within the context of familial/genetic syndromes are seen at much earlier ages.
Most aneurysms are small, but all enlarge over time and, if the patient lives long enough, eventually rupture. The risk of rupture of AAAs relates to size, which is generally expressed as the maximal transverse diameter. At diameters of more than 4.5 cm, the risk increases. FLOAT NOT FOUND
Physical diagnosis detection of AAA is at best modestly successful; in the presence of abdominal obesity, it is frankly poor. Screening for AAAs is most commonly performed by ultrasound because it is widely available, accurate, and without risk. Computed tomography aortography better and more extensively delineates aortic (and branch vessel) anatomy and pathology than ultrasound but with the potential of contrast nephropathy. Although ultrasound may image some cases of rupture or leak of an AAA, computed tomography is a far more reliable test to recognize leak.
In the era of endovascular aneurysm repair (EVAR), determination of the anatomy of the AAA relevant to EVAR repair requires the delineation of details relevant to EVAR technique such as the suitability of proximal and distal “landing zones.”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree