Fig. 7.1
Normal granular-appearing trochlear ossification center (arrow) in a 9-year-old boy
Supracondylar Process
The supracondylar process of the humerus occurs in approximately one percent of patients. This bony spur projects anteriorly and toward the elbow, 5–7 cm above the medial epicondyle (Fig. 7.2). Unlike an osteochondroma, the supracondylar process arises directly from the cortex [1]. Occasionally a fibromuscular band connects this to the medial epicondyle, giving rise to an anomalous origin of the pronator teres muscle. Bone may form within this ligament, resulting in an osseous tunnel; the median artery and nerve may become compressed. The supracondylar process is more common in Cornelia de Lange syndrome.


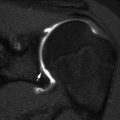
Fig. 7.2
Supracondylar process of the humerus (arrow), an uncommon normal variant
Fat Pads
Fat pads at the elbow are well-recognized normal anatomic features that are useful for determining the presence of joint fluid. Two rest in the radial and coronoid fossae anterior to the distal humerus, and the third lies in the olecranon fossa posterior to the distal humerus. Enveloped by leaflets of the joint capsule, they are intracapsular but extrasynovial. They are evident in essentially all children 2 years of age or older, with the two anterior fat pads superimposed on the lateral projection of the humerus. In a right-angle flexion view of the elbow, the normal anterior fat pad has a triangular or teardrop shape, whereas the normal posterior fat pad is hidden within the olecranon fossa and therefore inapparent (Fig. 7.3). In extension, however, the anterior fat pad is flattened somewhat by the brachialis muscle, and the normal posterior fat pad may become visible as the muscles posterior to it relax.


Fig. 7.3
Normal anterior fat pad (black arrow) in a 12-year-old boy. Also note the supinator fat plane (white arrows). No posterior fat pad is visible
The application of the elbow fat pad signs in diagnosis should be restricted to non-rotated radiographs performed with the elbow flexed. In the case of elbow joint effusion or hemarthrosis, the anterior fat pad is elevated and sickle-shaped, whereas the posterior fat pad becomes visible as it is pushed from its fossa by fluid expanding the intra-articular space (Figs. 7.4 and 7.5).

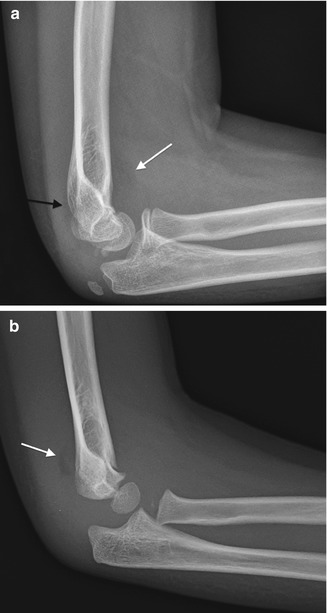

Fig. 7.4
Elevated fat pads. On this sagittal fast spin echo (FSE) fat-suppressed (FS) MR arthrogram of the elbow, the large amount of fluid within the joint elevates and clearly delineates the elevated and displaced anterior and posterior fat pads (arrows)
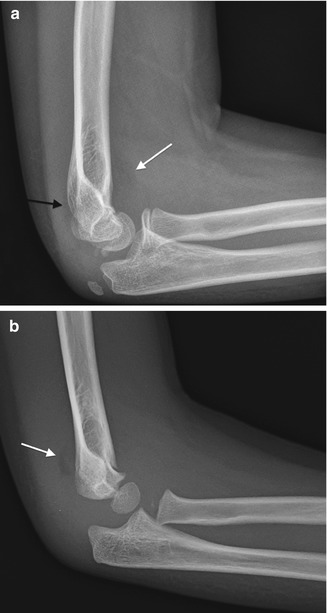
Fig. 7.5
Elevated fat pads at the elbow. (a) Anterior (white arrow) and posterior (black arrow) fat pads in a 10-year-old boy with a non-displaced supracondylar fracture. (b) Elevated posterior fat pad (arrow) in a 6-year-old boy with a supracondylar fracture and a hemorrhagic elbow effusion (note that the joint fluid is dense). The anterior fat pad has been pushed into the coronoid fossa
The supinator fat plane in the upper forearm lies anterior to the supinator muscle and proximal radius and posterior to the pronator teres and brachioradialis muscles. This is normally slightly bowed anteriorly, running roughly parallel to the proximal one third of the radius (see Fig. 7.3). The fat plane is displaced if the radial head is fractured or if there is arthritis or regional edema.
2 Congenital Limb Deficiencies
Congenital limb deficiencies occur in about 0.5 per 1,000 live births and usually affect the upper extremity. As in all birth disorders, classification is difficult and can be mired in an attempt to devise an all-inclusive system. Swanson’s classification system, adopted by the International Federation of Societies for Surgery of the Hand (IFSSH) in 1976, presents broad categories that can be adapted to either extremity and even to portions of the axial skeleton (Table 7.1) [3]. A more recent classification takes into account advances in the understanding of the molecular mechanisms of limb development (Table 7.2) [4].
Table 7.1
Swanson’s classification of congenital anomalies of the extremity
Failure of formation of parts/arrest of development |
Transverse: congenital arrested formation (amputation appearance) |
Longitudinal: deficiency in longitudinal axis |
Phocomelia |
Radial dysplasia |
Ulnar dysplasia |
Failure of differentiation or separation |
Elbow synostoses |
Radial head dislocation |
Poland deformity |
Sprengel deformity |
Duplication |
Overgrowth (gigantism) |
Undergrowth (hypoplasia) |
Congenital constriction band effects |
Generalized skeletal abnormalities |
Table 7.2
Classification of congenital anomalies of the hand and upper extremity based on developmental biology
Malformations |
Failure of axis formation/differentiation—entire upper limb |
Proximal-distal outgrowth |
Brachymelia with brachydactyly |
Symbrachydactyly |
Transverse deficiency |
Intersegmental deficiency |
Radial-ulnar (anteroposterior) axis |
Radial longitudinal deficiency |
Ulnar longitudinal deficiency |
Ulnar dimelia |
Radioulnar synostosis |
Humeroradial synostosis |
Dorsal-ventral axis |
Nail-patella syndrome |
Failure of axis formation/differentiation—handplate |
Radial-ulnar (anteroposterior) axis |
Radial polydactyly |
Triphalangeal thumb |
Ulnar polydactyly |
Dorsal-ventral axis |
Dorsal dimelia (palmar nail) |
Hypoplastic/aplastic nail |
Failure of handplate formation/differentiation—unspecified axis |
Soft tissue |
Syndactyly |
Camptodactyly |
Skeletal deficiency |
Brachydactyly |
Clinodactyly |
Kirner’s deformity |
Metacarpal and carpal synostoses |
Complex |
Cleft hand |
Synpolydactyly |
Apert hand |
Deformation |
Constriction ring sequence |
Arthrogryposis |
Trigger digits |
Not otherwise specified |
Dysplasias |
Hypertrophy |
Macrodactyly |
Upper limb |
Upper limb and macrodactyly |
Tumorous conditions |
Ossified structures as well as nerves, vessels, muscles, capsule, ligaments, and cartilage must be evaluated in order to devise the best functional remedy [5]. Magnetic resonance imaging (MRI) as well as pre- and postnatal ultrasound contributes important information.
Transverse defects are very rare and result from arrested formation, perhaps a consequence of vascular interruption. They are different from intrauterine amputation due to amniotic band formation. The most common anomaly consists of unilateral amputation of the forearm below the elbow (Fig. 7.6). Rudimentary digits may be attached to the stump. Longitudinal defects are more common and include phocomelia as well as both radial deficiency and the much rarer ulnar deficiency. Longitudinal defects are named by the bones that are completely or partially absent.


Fig. 7.6
Transverse deficiency. There is soft tissue distal to the hypoplastic radius and ulna and complete absence of formed osseous structures. As in this case, it is sometimes difficult to determine radiographically whether this appearance results from constriction bands or failure of formation, but the presence of fingernails is readily recognized clinically, helping differentiate transverse deficiency from amniotic bands (Image copyright Shriners Hospital for Children Northern California)
Examples of failure of differentiation or separation include synostoses about the elbow (radioulnar being by far the most common) as well as radial head dislocation. Sprengel deformity (see Chap. 5) and Poland deformity (see Chap. 9) also fit this category.
Defects of duplication, overgrowth, undergrowth and constriction bands are most common in the hand (Chap. 9).
The more common entities are addressed here, and for those interested standard references can be consulted for more comprehensive analysis [3, 6, 7].
2.1 Phocomelia
Phocomelia refers to a flipper-like (Greek phoke, meaning “seal”) anomaly with a distal part (also often abnormal) attached proximally with what grossly appears to be the absence of an intermediate segment [3] (Fig. 7.7). This denotation may be applied to both the upper and lower extremities. The hand may appear to be attached to the trunk, or there may be variable intervening segments of bone. Formerly considered a transverse intercalary segmental defect, phocomelia has recently been redefined as a subset of longitudinal deficiency [8]. Phocomelia is subdivided into three groups, based on whether there is proximal radial longitudinal dysplasia, proximal ulnar longitudinal dysplasia, or combined dysplasia, with an absent forearm or—occasionally—also an absent arm.
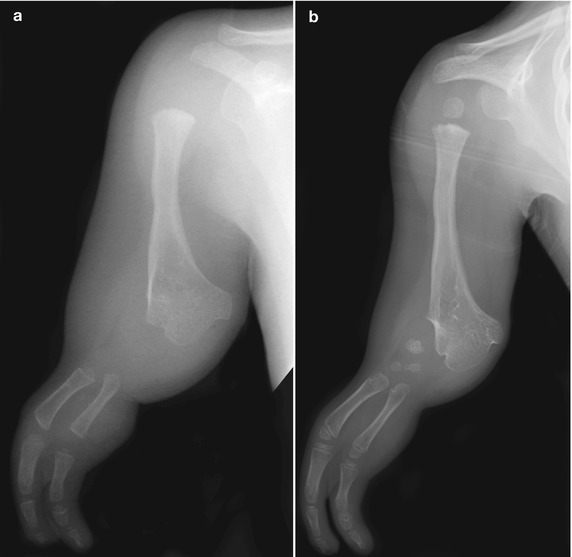
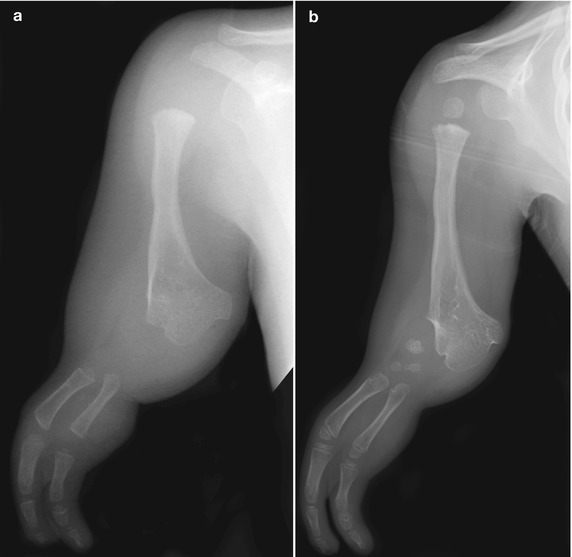
Fig. 7.7
Phocomelia. (a) The splayed distal humerus in this 2-year-old may represent a conglomeration of remnants of the proximal radius and ulna. Rays are deleted, and there is a large soft tissue gap between the bony mass and the two metacarpals. Note the flipper-like outline of the soft tissues. The parahumeral fat appears abnormal. (b) Four years later, three carpal bones have ossified, and the rays demonstrate further development. The parahumeral fat is more normal (Images copyright Shriners Hospital for Children Northern California)
The digits are frequently abnormal or missing, and the joints are unstable owing to musculoligamentous relaxation or deficit. Other skeletal and systemic anomalies are frequently present (e.g., thalidomide embryopathy, thrombocytopenia-absent radius (TAR), Holt-Oram syndrome, and others [7]). Abnormalities of all four limbs (tetra-phocomelia) are associated with facial dysmorphism in Roberts syndrome. Extreme cases of Poland syndrome may manifest phocomelia, further discussed in Chap. 9.
2.2 Radial Longitudinal Deficiency (or Radial Dysplasia, Radial Clubhand) (Box 7.1)
Box 7.1: Radial Longitudinal Deficiency
Complete or partial absence of the radius |
Short, bowed ulna |
Radioulnar synostoses common |
Radial clubhand: hand at right angle to forearm |
Navicular and thumb often absent |
Several synonyms refer to radial longitudinal deficiency, stressing various aspects of the abnormality, such as its clinical appearance (radial clubhand) or the complete (radial aplasia) or partial (radial meromelia) absence of the radius. From a strictly anatomic point of view, this is an intercalary, longitudinal, radial meromelia, but the terms radial dysplasia or radial longitudinal deficiency are more appropriate, encompassing the accompanying abnormal nerves, blood vessels, muscles, and adjacent joint anomalies or fusion as well.
Radial longitudinal deficiency is often associated with other systemic or musculoskeletal abnormalities and is indeed isolated in only 33 % of patients [9]. Syndromes are present in about 33 %, usually thrombocytopenia-absent radius (TAR) syndrome or VACTERL association (vertebral-anal-cardiac-tracheo-esophageal-renal-limb anomalies) [9, 10]. Holt-Oram syndrome occurs in about 13 %. Cardiac lesions are usually ventricular or atrial septal defects, but pulmonary artery atresia and patent ductus arteriosus are also reported.
Two types of hematologic syndromes are associated with radial longitudinal deficiency. Fanconi anemia is an autosomal recessive aplastic anemia that presents between 2 and 15 years of age. It can be fatal if not treated by bone marrow transplantation. For this reason, all children with radial longitudinal deficiency should undergo a chromosomal breakage test, which can test for Fanconi anemia before the development of any symptoms. Second, congenital amegakaryocytic thrombocytopenia has been reported in frequent association with TAR syndrome. The TAR syndrome may also be associated with dysplastic genu varum, hooking of the lateral clavicle, and primary cranial synostosis (Baller-Gerold syndrome). This is probably an autosomal recessive disorder, and it may be diagnosed by fetal ultrasound. Children with TAR syndrome tend to have normal thumbs (Fig. 7.8), whereas the thumbs of most children with an absent radius (in the absence of TAR) are absent or hypoplastic.


Fig. 7.8
Thrombocytopenia-absent radius (TAR). Neither radius is ossified. The ulnas are short and thick. The left carpus has been surgically centered on the distal ulna, whereas on the right there is still clubhand deformity. Both thumbs are present. Note the carpal bones on the left are more mature than those on the right (Image copyright Shriners Hospital for Children Northern California)
Approximately 33 % of patients have nonsyndromic additional osseous abnormalities. Scoliosis is the most commonly associated abnormality; other associated abnormalities include humeral hypoplasia, proximal radioulnar synostosis, congenitally dislocated radial head, and stiff digits. The likelihood of having associated anomalies increases with the severity of radial longitudinal deficiency. If the radius is completely absent, additional anomalies are present in 80 %, whereas if the proximal humerus is also absent, essentially all children have additional anomalies. If only the thumb is hypoplastic, 35 % of children have additional anomalies [9].
Radial dysplasia occurs in 1 in 30,000 live births and is most common in boys. It is more often sporadic than inherited [11]. Up to 50 % are bilateral. When unilateral, the right side is affected twice as frequently as the left [12]. Radial longitudinal deficiency has been classified into six types based on the extent of radial shortening and the extent to which the thumb and carpus are involved [13] (Table 7.3). The radial anomaly takes three forms. Total aplasia is most common, occurring in 60 % (Fig. 7.9). Partial aplasia occurs in about 20 % and is usually characterized by absence of the distal growth plate and epiphysis, with deformity of the proximal portion (occasionally only the proximal radius is absent). Hypoplasia is defined as diminution in size without segmental absence. More mild deficiencies can present as absence or hypoplasia of the radial carpal bones or the thumb.

Table 7.3
Classification of radial longitudinal deficiency
Type | Thumb | Carpus | Distal radius | Proximal radius |
|---|---|---|---|---|
N | Hypoplastic or absent | Normal | Normal | Normal |
0 | Hypoplastic or absent | Absence, hypoplasia, or coalition | Normal | Normal, radioulnar synostosis, or congenital dislocation of radial head |
1 | Hypoplastic or absent | Absence, hypoplasia, or coalition | >2 mm shorter than ulna | Normal, radioulnar synostosis, or congenital dislocation of radial head |
2 | Hypoplastic or absent | Absence, hypoplasia, or coalition | Hypoplasia | Hypoplasia |
3 | Hypoplastic or absent | Absence, hypoplasia, or coalition | Physis absent | Variable hypoplasia |
4 | Hypoplastic or absent | Absence, hypoplasia, or coalition | Absent | Absent |

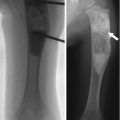
Fig. 7.9
Radial aplasia (same patient as Fig. 7.10). (a, b) There is radial aplasia with radial clubhand deformity and aplastic thumb. The ulna is hypoplastic and bowed (Images copyright Shriners Hospital for Children Northern California)
Stretching and corrective casting soon after birth may prevent further contracture. Centralization, the procedure to position the carpus on the ulna, is controversial, as it often leads to a stiff, albeit straighter, forearm and wrist, with a high likelihood of complications including growth arrest and recurrent contracture. Lengthening of the radius has been proposed but often requires several surgeries with a high risk of complications. Surgical treatment of the thumb deficiency, including tendon transfers and pollicization, is more commonly performed (Figs. 7.10 and 7.11). In pollicization, a digit (usually the second) is transferred to the position of the thumb and also rotated.



Fig. 7.10
Radial aplasia, after pollicization and centralization (same patient as Fig. 7.9). (a, b) The second finger has been transferred to the position of the thumb and rotated (arrow). Note carpal fusion (Images copyright Shriners Hospital for Children Northern California)

Fig. 7.11
Partial radial longitudinal deficiency. (a, b) The second ray has been pollicized and the carpal bones centralized (Images copyright Shriners Hospital for Children Northern California)
Imaging
Radiographs demonstrate complete or partial aplasia of the radius. The hand is positioned at a right angle to the forearm, angulated laterally due to the pull of abnormally positioned muscles or a fibrous band that may replace the radius (Fig. 7.12).


Fig. 7.12
Radial aplasia leading to radial clubhand deformity. The radius is absent, and the ulna is hypoplastic. The hand is positioned at a right angle to the forearm (Image copyright Shriners Hospital for Children Northern California)
At birth, the ulna is short, typically 60 % of normal, and this relative deficiency persists. Ossification of the distal ulnar epiphysis may be delayed, and it may fuse prematurely. The ulna is bowed with convexity posterior and medial. The humeral-ulnar articulation is frequently abnormal, and the humerus may also be shortened. Both increased laxity and contractures occur. Proximal radioulnar synostosis and congenitally dislocated radial head are commonly associated with cases of relatively mild radial longitudinal deficiency [11].
The wrist joint is often replaced by a mass of unorganized fibrous tissue. The navicular is almost always absent, and the trapezium is missing in about two thirds. However, the capitate, hamate, triquetrum, and ulnar four metacarpals and phalanges are almost always normal. The thumb is absent in up to 75 % of patients and hypoplastic in another 20 % (Fig. 7.13). Occasionally there is a fleshy rudimentary appendage.


Fig. 7.13
Radial aplasia with absent thumb. The ulna is short and dysplastic (arrow), and the texture of the fat is abnormal. The middle and distal phalanges of the first ray are duplicated (Image copyright Shriners Hospital for Children Northern California)
Cross-Sectional Imaging
Prenatal ultrasound can identify radial dysplasia. MRI is useful for surgical planning, as it may allow identification of a radiologically occult cartilaginous anlage of the radius, and if not resected such a structure may tether the ulna’s growth. MRI also allows characterization of the cartilaginous ends of the ulna.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree