Radiology is rapidly emerging beyond its traditional role of diagnosing disease, as a powerful tool in cancer prevention and patient advocacy. With advancements in imaging technologies, artificial intelligence, and early detection methods, radiologists are now positioned at the forefront of proactive healthcare.
Their work extends beyond identifying tumors to guiding preventive care strategies, strongly supporting personalized treatment plans, and advocating for patient-centered decision-making. As cancer rates continue to rise, the future of radiology lies in its ability to integrate innovation with compassionate care.
In this article, we will explore how radiology is reshaping the prevention, detection, and management of cancer for better patient outcomes.
Radiology’s Expanding Role in Cancer Prevention
Radiology plays an increasingly vital role in cancer prevention by enabling early detection and intervention. It plays a critical role in decreasing cancer burden through proactive screening.
The International Atomic Energy Agency reports that around 50-70% of all patients with cancer require radiotherapy. However, more than 50% of these needy people are living in low and middle-income countries (LMICs). International efforts are being made that can address these global gaps.
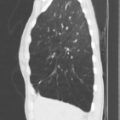
Various types of screenings, like mammography, low-dose CT screening, help in early cancer detection. Radiologic screening methods like colonoscopy and CT colonography can reduce incidence and mortality in colorectal cancer.
Patient-Centered Imaging and Advocacy
Radiologists are increasingly engaging with patients by explaining to them and supporting them in making informed decisions. By promoting transparency and shared understanding of imaging results, specialists help patients feel more empowered.
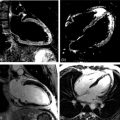
According to the American Cancer Society, doctors use imaging tests to view inside the body, detect cancer, track its spread, and monitor treatment. These tests use energy forms such as X-rays, sound waves, radioactive particles, or magnetic fields. Body tissues convert the energy to create pictures through which doctors identify changes caused by diseases like cancer.
These results can be shared with patients as part of patient advocacy. It ensures radiology is not only about detecting disease but also about guiding patients with empathy and respect.
Occupational and Environmental Cancer Risks Revealed by Imaging
Radiology not only advances early detection but also exposes patterns of cancer linked to occupational and environmental hazards. Imaging often uncovers malignancies caused by long-term exposure to diesel exhaust, asbestos, and other industrial toxins. A well-known example is the railroad lawsuit for colon cancer, where workers developed higher cancer risks after years of exposure to hazardous environments.
According to Gianaris Trial Lawyers, railroad workers are exposed to toxins such as diesel exhaust, benzene, asbestos, crude oil, creosote, and silica dust. These hazards are tied to serious illnesses, including cancers and serious lung, blood, and organ diseases.
In such cases, radiology is central to confirming diagnoses that guide both life-saving treatment and legal accountability. By providing objective medical evidence, radiology helps connect cancer outcomes to workplace conditions. Ultimately, medical imaging not only drives prevention and care but also supports advocacy for safer working conditions.
Technology Driving Accessibility and Equity in Cancer Screening
Technology now enables remote image sharing, and tele-radiology allows specialists to provide timely insights regardless of geography. These innovations reduce disparities in early detection, ensuring more people benefit from preventive screening.
According to the National Library of Medicine, about 1.9 million new cancer cases and 609,360 deaths were projected in the US in 2022. From 1991 to 2019, cancer mortality dropped 32%, preventing 3.4 million deaths. This progress is linked to reduced smoking, improved treatments, and advanced screenings, which enable earlier cancer detection.
Advances in imaging technology are making cancer screening more accessible and equitable worldwide. Portable ultrasound, low-dose CT, and AI-driven imaging tools are reaching underserved populations.
Radiology as a Partner in Legal and Ethical Advocacy
Radiology is emerging as a key partner in legal and ethical advocacy by ensuring transparency, accuracy, and fairness in patient care. Radiologists often provide expert testimony in malpractice or cancer misdiagnosis cases, reinforcing the importance of precise imaging.
Ethically, they advocate for patient rights by promoting informed consent, minimizing radiation exposure, and protecting privacy in digital imaging. This way, radiology strengthens trust in healthcare while safeguarding patients’ interests.
The Road Ahead: Empowering Patients Through Imaging
The future of radiology lies in empowering patients through accessible, transparent, and personalized imaging. Advances in AI, 3D imaging, and predictive analytics will provide a better understanding of health risks and treatment options.
According to the National Cancer Institute, predictive analytics applies mathematics and data analysis to help researchers forecast potential outcomes. It is especially important in oncology since many early-stage cancers lack noticeable symptoms. As a result, doctors often depend on these predictions to determine whether treatment is necessary.
Radiologists are moving beyond diagnosis to serve as guides to help individuals make informed choices. By combining innovation with advocacy, imaging will not only detect disease earlier but also foster patient confidence.
Frequently Asked Questions
How early can radiology detect signs of cancer?
Radiology can detect cancer at very early stages, often before symptoms appear. Techniques like low-dose CT, mammography, and MRI can identify tumors or abnormal tissue when they are just millimeters in size. Early detection significantly improves treatment outcomes and survival rates.
How do radiologists work with oncologists in cancer care?
Radiologists collaborate closely with oncologists to guide diagnosis, treatment planning, and monitoring. They interpret imaging results, track tumor progression, and assess therapy effectiveness. This partnership ensures personalized and data-driven decisions. It also helps oncologists to adjust treatments promptly, together providing coordinated care.
Is medical imaging safe for long-term monitoring?
Medical imaging is generally safe when appropriate protocols are followed. Techniques like MRI and ultrasound avoid radiation, while low-dose CT minimizes exposure. Radiologists balance frequency with patient safety to ensure benefits without much risk. Continuous monitoring helps detect changes early without compromising health.
Radiology: Shaping the Future of Cancer Care
Radiology is transforming cancer prevention and patient advocacy by combining cutting-edge technology with compassionate patient care. From early detection and personalized imaging to ethical advocacy and equitable access, radiologists play a pivotal role in empowering patients.
As innovations continue, radiology will not only enable earlier disease detection but also guide more informed medical decisions. It will further help improve outcomes and amplify the patient’s voice during treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree