The Radius and Ulna
This chapter will focus on fractures of the radial and ulnar shafts. Monteggia and Galeazzi fractures will be included. Fractures of the radius and ulna may occur together or separately. Forearm fractures account for 10% to 14% of all skeletal fractures. The mechanisms of injury may be related to a direct blow, a fall on the outstretched hand, motor vehicle accidents, and gunshot wounds. Associated injuries of the elbow and wrist are fairly common. In a large series of adult forearm fractures, 75% involved both the radius and ulna, 15% the ulna alone, and 10% the radius alone. The incidence is also increasing in adolescents around the age of puberty when activities are increasing and bone turnover due to growth spurts is more active resulting in increased cortical porosity. In the last 30 years, the incidence of forearm fractures has increased 56% in adolescent females and 32% in males.
The incidence of fractures also varies with location in both the radius and ulna. In the ulna, 13% of fractures involve the proximal third, 59% the middle third, and 28% the distal third. In the radius, 21% involve the proximal third, 61% the middle third, and 18% the distal third. Clinical examination should include assessment of soft tissues for abrasions or open wounds and evaluation of neurovascular structure to rule out compartment syndrome.
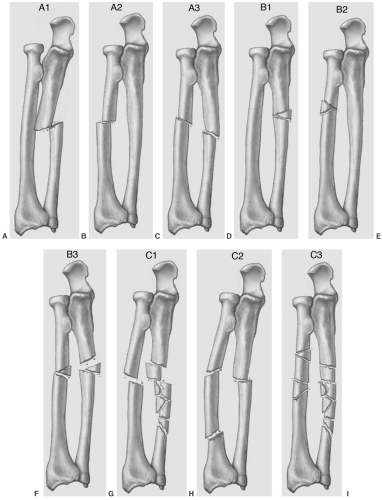
Fracture eponyms for forearm fractures such as nightstick (isolated ulnar fracture), greenstick (incomplete bowing fracture), and microfracture were reviewed in Chapter 2. The Orthopaedic Trauma Association (OTA) classification will be used in this section to facilitate discussion of treatment. Classification of diaphyseal fractures includes simple (type A), wedge or butterfly (type B), and complex (type C). The OTA has added three subcategories to each and multiple subcategories (see Fig. 12-1). The latter group addresses variations in complexity and associated dislocations of the radial head or distal radioulnar joint.
Orthopaedic Trauma Association Classification
Type A: Simple
A1—simple ulna, radius intact
A2—simple radius, ulna intact
A3—simple fractures of both bones
Type B: Wedge (butterfly fragment)
B1—wedge ulna, radius intact
B2—wedge radius, ulna intact
B3—wedge fractures of both bones
Type C: Complex
C1—Complex ulna, simple radius
C2—Complex radius, simple ulna
C3—Complex fractures of both the radius and ulna
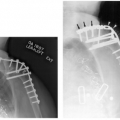
Two additional fractures are associated with articular dislocations. The Monteggia fracture (see Chapter 2) is a fracture of the proximal third of the ulna with an associated radial head dislocation. Monteggia fractures account for approximately 5% of forearm fractures. Type I Monteggia lesions (60%) present with anterior dislocation of the radial head and an ulnar fracture that is typically angulated anteriorly. Type II Monteggia lesions (15%) present with posterior or posterolateral radial head dislocation and the ulnar fracture is angulated more posteriorly (see Fig. 12-2). Type III lesions (20%) present with anterolateral or lateral dislocation of the radial head and an ulnar metaphyseal fracture (see Fig. 12-3). Type IV injuries (5%) present with anterior dislocation of the radial head and fractures of both the proximal radius and ulna.
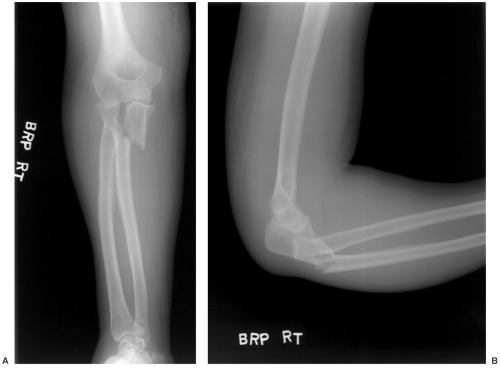 Fig. 12-2 Monteggia fracture. Anteroposterior (AP) (A) and lateral (B) radiographs of a type II fracture with posterior dislocation of the radial head and posterior angulation of the ulnar fracture. |
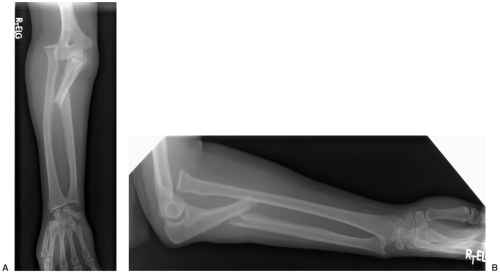 Fig. 12-3 Monteggia fracture. Anteroposterior (AP) (A) and lateral (B) radiographs of a type III lesion with anterolateral radial head dislocation and anterior angulation of the ulnar fracture. |
The Galeazzi fracture is a fracture of the distal radius with dislocation or subluxation of the distal radioulnar joint (see Fig. 12-4). This injury accounts for 5% to 7% of forearm fractures.
 Fig. 12-4 Galeazzi fracture. Anteroposterior (AP) (A) and lateral (B) radiographs of a distal radial fracture with dislocation of the distal radioulnar joint. |
Suggested Reading
Goldfarb CA, Ricci WM, Tull F, et al. Functional outcomes after fractures of both bones of the forearm. J Bone Joint Surg. 2005;87B:374–379.
Khosla S, Melton JL III, Dekutoske MB, et al. Incidence of childhood distal forearm fractures over 30 years. JAMA. 2003;290:1479–1485.
Orthopaedic Trauma Association Committee for Coding and Classification. Fracture and dislocation compendium. J Orthop Trauma. 1996;10:21–25.
Reckling FW, Cordell LD. Unstable fracture-dislocation of the forearm (Monteggia and Galeazzi lesions). J Bone Joint Surg. 1982;64A:999–1007.
Imaging of Forearm Fractures
Radiographic evaluation is essential to evaluate the position, location, and type of fracture or fracture dislocation. Images must include the elbow and wrist. Anteroposterior (AP) and lateral views are obtained at a minimum. Oblique views may add additional information. The radiocapitellar relationship must be accurately evaluated. A line drawn through the mid radial head should intersect the capitellum regardless of the radiographic projection (see Fig. 12-5). Evaluation of the distal radioulnar joint is more difficult unless completely dislocated. Subluxation of the distal radioulnar joint may be difficult to evaluate on radiographs. In this setting, axial computed tomographic (CT) images in neutral, pronation, and supination will make the diagnosis. CT imaging can be performed after the other injuries are stabilized. Magnetic resonance imaging (MRI) is rarely indicated in the acute setting but may be helpful in patients with suspected compartment syndrome or interosseous membrane injury. Injury to the interosseous membrane may
result in long-term function loss. Therefore, early diagnosis and management is important.
result in long-term function loss. Therefore, early diagnosis and management is important.
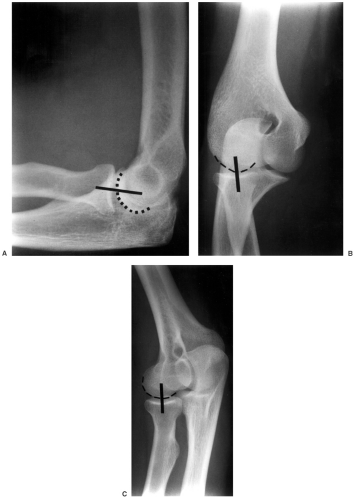 Fig. 12-5 Normal radiographic views of the elbow demonstrating the radiocapitellar line. Lateral (A) and both oblique views (B and C) show the line drawn through the mid radial head intersecting the capitellum in all projections.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|