Understanding Why Imaging Matters After Surgery
Recovering from orthopaedic surgery can feel both hopeful and uncertain. Patients naturally expect some soreness and stiffness, but when symptoms linger or seem unusual, it can be hard to know what’s normal healing and what might require attention. That’s where radiologic imaging becomes incredibly important—it helps clinicians see below the surface and understand exactly what’s happening within the recovering area.

Even follow-up care with specialists or a top-rated physical therapy clinic often depends on precise imaging, because it provides clarity on how well the body is healing and whether additional support may be needed. Radiologic imaging plays a major role in confirming that surgical repairs are staying in place, tissues are healing properly, and no new complications have developed. This gives patients peace of mind and gives clinicians the information they need to guide a safe and smooth recovery journey.
Why Radiologic Imaging Is Essential in Postoperative Orthopaedics
Radiologic imaging is more than a diagnostic tool—it is a roadmap for recovery. After surgery, patients may experience swelling, pain, or discomfort, and imaging helps distinguish expected healing from warning signs. Without it, identifying complications would rely heavily on guesswork, which could delay treatment.
Imaging also helps clinicians track progress over time. By comparing postoperative scans with earlier images, they can monitor how tissues, bones, and surgical hardware continue to heal. This long-term perspective supports better decision-making and helps prevent minor issues from evolving into larger concerns.
The Most Common Imaging Methods After Orthopaedic Surgery
X-Ray
X-rays are often the first imaging tool used after surgery because they provide clear pictures of bones and surgical hardware. They are excellent for checking alignment, ensuring implants are secure, and confirming that fractures are healing as expected. Because X-rays are quick and widely available, they are usually the initial step in evaluating new postoperative symptoms.
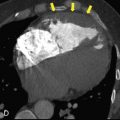
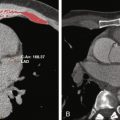
CT Scan
A CT scan provides more detailed, three-dimensional images of bone structures. This is especially helpful for complex fractures or areas where small changes can make a big difference. CT imaging is also useful for diagnosing subtle complications that might not show up on a standard X-ray.
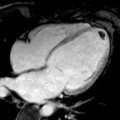
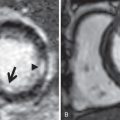
MRI
MRIs are the best imaging option for soft tissues such as muscles, ligaments, tendons, and cartilage. After surgery, MRI helps identify swelling, tears, or unexpected tissue changes. It is also an important tool when clinicians suspect infection or inflammation that may not be visible on an X-ray or CT scan.
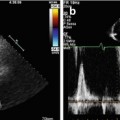
Ultrasound
Ultrasound imaging is often used to examine soft-tissue issues, especially when fluid buildup is suspected. It can reveal hematomas, cysts, or swelling around surgical sites. In some cases, ultrasound is used to guide procedures like fluid aspiration, helping clinicians treat complications with greater accuracy.
Postoperative Complications That Imaging Helps Detect
Hardware Problems
Surgical hardware such as plates, rods, screws, or joint replacements must stay firmly in place to support healing. Imaging helps identify loosening, shifting, or breaking, which may cause discomfort or interfere with recovery. Early detection allows surgeons to address these issues before they worsen or affect long-term function.
Infection
Postoperative infection is a serious complication that requires prompt treatment. MRI, CT, and ultrasound can reveal fluid collections, abscesses, or signs of bone infection. By identifying the source of infection early, clinicians can act quickly with antibiotics or procedures to prevent further damage.
Fracture or Re-Fracture
Sometimes, new fractures or stress fractures can occur near a surgical site. Imaging helps determine whether new pain is part of normal healing or a sign of a new injury. This distinction is critical for choosing the right treatment plan and preventing additional harm.
Soft-Tissue Complications
Soft-tissue problems such as tendon irritation, ligament injury, or excessive swelling are common after surgery. MRI and ultrasound provide detailed images that show how tissues are responding to the operation and whether additional care is needed. Addressing soft-tissue issues early can prevent long-term stiffness or discomfort.
Vascular or Nerve Concerns
Although less common, vascular or nerve complications can occur after surgery. Advanced imaging helps identify blood-flow problems or nerve compression before they lead to lasting symptoms. This quick insight supports fast, targeted treatment.
How Imaging Guides Team-Based Recovery
Supporting Surgeons
Imaging allows surgeons to confirm that their repairs are stable and healing as intended. If complications arise, the images guide decisions about whether additional surgery, medication changes, or activity adjustments are needed. This ensures that treatment plans remain safe and effective.
Helping Rehabilitation Teams
Physical therapists rely on imaging results to tailor exercises and activities. By understanding the exact condition of bones, joints, and soft tissues, they can design a program that strengthens the body without putting the healing area at risk. This leads to smoother progress and fewer setbacks.
Improving Communication Across Care Providers
Radiologists, surgeons, and rehabilitation specialists use imaging to coordinate care. When everyone understands the full picture of recovery, patients receive more consistent guidance and feel more confident in their healing journey.

What Patients Gain from Radiologic Imaging
Peace of Mind
Knowing how healing is progressing gives patients reassurance and reduces unnecessary worry. Even when discomfort occurs, imaging helps answer questions clearly and accurately.
Earlier Treatment and Better Outcomes
Identifying complications early means they can be treated before they escalate. Quick action often leads to shorter recovery times and better long-term results.
A Clearer Path Forward
Imaging supports informed decision-making. Patients and clinicians can discuss options with confidence, knowing that decisions are backed by clear visual information.
When Patients Should Ask About Imaging
Imaging is recommended when symptoms worsen or fail to improve. Red flags include sudden swelling, persistent fever, unexpected weakness, or significant changes in pain. Surgeons may also schedule routine imaging to monitor healing milestones, even when recovery seems normal. Asking about imaging is always appropriate if a patient feels unsure about new or changing symptoms.
Seeing Clearly Leads to Healing Confidently
Radiologic imaging is one of the most valuable tools in postoperative orthopaedic care. It helps ensure that both the surgical repair and the recovery process stay on track, offering crucial insight when questions or concerns arise.
By combining expert imaging with skilled surgical care and thoughtful rehabilitation, patients can move through recovery with greater confidence, knowing that potential complications can be detected and addressed early. In the end, clear visuals lead to clearer decisions—and a safer, smoother return to everyday life.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree