Fig. 33.1
Marking the incision in a naturally occurring skin crease while the patient is in an upright position ensures optimal positioning of the scar. Reproduced with permission from: Terris DJ. Novel surgical maneuvers in modern thyroid surgery. Operative Techniques in Otolaryngology. 2009;20:23–28
Since the ideal location of the scar is primarily determined by the patient’s skin creases, the ultrasonographic findings do not generally alter the recommended position of the thyroidectomy incision. Although a slightly higher incision may be contemplated to improve the exposure of the superior aspect of the gland, it is often more cosmetically favorable to extend the incision within an ideal skin crease than to increase the visibility of the scar by creating a shorter incision higher in the neck in an unfavorable skin crease.
Ultrasound is more helpful in determining the type of surgical approach utilized and the length of the incision [10], particularly when directly performed by the surgeon [11]. Patients with small nodules (≤30 mm) and normal size glands (volume ≤ 20 mL) with no substernal or extrathyroidal extension on ultrasound may be candidates for a minimally invasive video-assisted thyroidectomy approach (Fig. 33.2) [12]. This procedure is routinely performed through a 20 mm incision, and is associated with less postoperative pain, a faster recovery, and improved cosmetic outcomes when compared to conventional thyroid surgery [13, 14]. Depending on their body habitus and associated conditions such as thyroiditis (Fig. 33.3) or prior central neck surgery, patients with larger nodules or glands, or with extrathyroidal or substernal extension on ultrasound may need larger incisions.


Fig. 33.2
Thyroid nodule (white arrow) that is suitable for minimally invasive video-assisted thyroidectomy approach
Fig. 33.3
Ultrasound appearance of Hashimoto’s thyroiditis . This condition makes minimally invasive video-assisted and remote access thyroidectomy approaches challenging
Ultrasound is also particularly useful in evaluating for metastatic lymphadenopathy in the central and lateral neck in patients with known or suspected thyroid cancer. Suspicious lymph nodes can be biopsied using ultrasound guidance, and if metastatic disease is confirmed the incision can be adjusted as necessary to permit dissection of these nodal compartments at the time of the initial thyroid surgery .
33.2.2 Parathyroid
Parathyroid surgery has historically necessitated a long cervical incision and bilateral neck exploration to evaluate all four parathyroid glands, even though the majority of cases of primary hyperparathyroidism are caused by a solitary adenoma. Advances in intraoperative parathyroid hormone (PTH) assessment and preoperative imaging techniques have rendered many patients with primary hyperparathyroidism eligible for minimally invasive, single gland surgery.
This image-directed approach relies largely on complementary information provided by technetium-99m (99mTc)-sestamibi (sestamibi) scanning and ultrasound (Fig. 33.4). If both the sestamibi and ultrasound co-localize an abnormal parathyroid gland in the same central neck quadrant, the operation may be performed through an inconspicuous 20 mm (or less) midline incision [15, 16]. As in thyroid surgery, this small incision is hidden in a preexisting neck crease to optimize the long-term cosmetic outcome of the procedure. Both sides of the neck are accessible through these small central incisions, so failure to localize the adenoma with preoperative ultrasound is not a contraindication to small incision surgery.
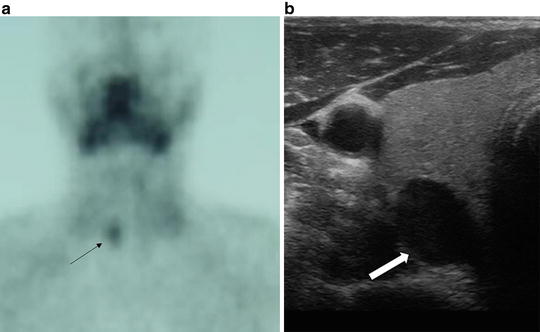
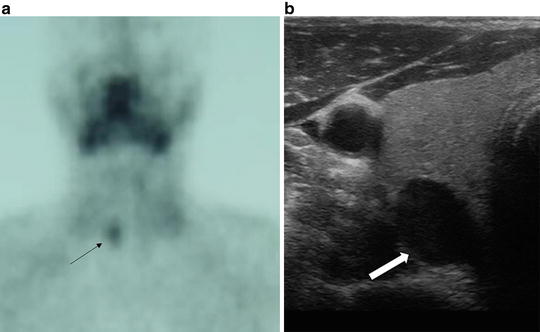
Fig. 33.4
Concordant sestamibi (a) and ultrasound (b) imaging showing a right inferior parathyroid adenoma (arrow), appropriate for minimally invasive parathyroid surgery
Alternatively, some authors prefer a laterally based incision for parathyroid surgery depending on the imaging results [17]. While this incision placement may offer a more direct approach for superior adenomas and avoid some of the central scar tissue when pursuing reoperative procedures, it sacrifices the cosmetic symmetry of a centrally placed incision, and requires a second incision if contralateral disease is suggested by intraoperative PTH assessment .
33.3 Ultrasound for Remote Access Approaches
Remote access thyroid surgery removes the incision from the visible portion of the anterior neck, concealing the scar in a distant, hidden location. These approaches generally access the thyroid compartment using axillary, chest, or postauricular incisions. While these procedures were initially performed using endoscopic assistance, the application of robotic surgical technology has increased their global popularity. The two most commonly performed robotic-assisted remote access thyroid operations are the robotic axillary thyroidectomy (RAT) and the robotic facelift thyroidectomy (RFT) (Fig. 33.5) [18, 19].
Fig. 33.5
Comparison of the incision location and approach for the robotic facelift thyroidectomy (RFT) and the robotic axillary thyroidectomy (RAT). Reproduced with permission from Duke WS, Terris DJ. Alternative approaches to the thyroid gland. Endocrinol Metab Clin N Am. 2014;43:459–474
Ultrasound is critical in determining a patient’s candidacy for remote access thyroid surgery. While there are no uniform selection criteria for RAT [20, 21], the procedure was initially reserved for patients with benign nodules ≤5 cm or malignant lesions ≤2 cm [18, 22]. RFT requirements are more firmly defined, recommending that nodules be <4 cm and presumed benign for consideration [23]. For both approaches, ultrasound findings of extrathyroidal, substernal, or retropharyngeal extension exclude patients from consideration [18, 23]. A history of or ultrasound findings consistent with Hashimoto’s thyroiditis are also contraindications to remote access thyroid surgery [23], and RFT is not indicated in the setting of metastatic disease [23]. Total thyroidectomy through a single incision has been reported using RAT [24]. With RFT , bilateral thyroidectomy may be accomplished [25]; however, we prefer a staged bilateral procedure if the ultrasound shows bilateral disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree