Chapter 7 The shoulder girdle
The use of plain imaging is still an essential starting point when investigating shoulder trauma,1 and basic diagnostic errors may occur if other imaging modalities are used alone, without the use of conventional plain radiography.2 Guidelines still suggest that plain radiography is indicated for fractures, dislocations, shoulder instability and calcific tendonitis, with magnetic resonance imaging (MRI), ultrasound and computed tomography (CT) suggested for soft tissue injuries and ‘more complex cases’. More specifically, ultrasound is recommended for rotator cuff injuries.2
Ultrasound can be used to assess disorders such as defects in the long head of the biceps tendon.2 Subacromial and acromioclavicular joint impingement are dynamic processes and these can also be studied during ultrasound examination.
CT may be used in preoperative assessment of shoulder injuries, so that fractures are not underestimated (as can be the case in some instances with plain X-ray images) and 3D reconstruction is often used to fully demonstrate complex fractures and assist in surgical planning.1
MRI has become an increasingly important technique for evaluating rotator cuff disorders and joint instability,1,2 its effectiveness being due to high contrast sensitivity and multiplanar imaging capabilities; therefore, diagnosis and appropriate management of the complex shoulder joint is established with greater confidence.
Indications
Fracture
Fractures of the surgical neck of the humerus and the tuberosities have often been classified using Neer’s method,3 which considers the status and degree of displacement of the articular segment of the head of the humerus, the surgical neck of the humerus and the greater and lesser tuberosities. The reliability of such classification systems has been questioned and alternative classification methods suggested;4 however, it must be mentioned that new methods, however reliable, need to be widely accepted so that they can be considered rigorous.
Dislocation
The shoulder joint is the most commonly dislocated joint in the human body,5 with anterior dislocation most common; only up to 5% of dislocations occur posteriorly,6 and an estimated 60–80% of these are missed on initial examination. As many as 50% of these uncommon dislocations can often be missed in A&E, highlighting the importance of an additional projection that can identify posterior dislocations.7 Subluxation of the acromioclavicular joint can also occur.
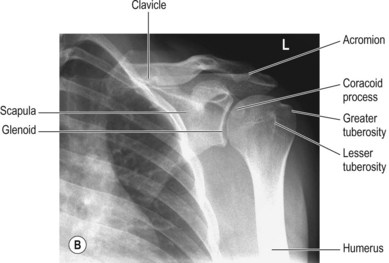
Anteroposterior (AP) shoulder (Fig. 7.1A,B)
Positioning
• A lead rubber apron is applied to the patient’s waist for radiation protection
• The patient sits or stands erect, with the posterior aspect of the shoulder under examination in contact with the vertical IR
• The arm is fully extended and slightly abducted with the palm of the hand facing forward to ensure the true anatomical position (with the greater tuberosity in profile on the lateral aspect of the humeral head)
• The patient’s trunk is rotated approximately 20° towards the side under examination, to bring the scapula parallel to the IR
• The patient’s head is turned away from the side under examination for radiation protection
Collimation
The head and proximal third of humerus, scapula, clavicle, lateral soft tissues of proximal humerus
Criteria for assessing image quality
• Head and proximal third of humerus, clavicle, acromioclavicular joint and the inferior end of the scapula are demonstrated
• Greater tuberosity is seen in profile on the lateral aspect of the head of humerus
• Glenohumeral joint is obscured by head of humerus
• Acromion is demonstrated clear of the superior border of the humeral head
• Sharp image demonstrating the bony cortex and trabeculae of the head of the humerus in contrast with the shoulder joint and surrounding soft tissues; the acromioclavicular joint is seen clearly
The AP projection does not demonstrate the glenohumeral joint space clearly and orthopaedic departments may request either a ‘True AP’ or ‘Grashey AP’3 instead of, or to complement, the AP. This projection uses the same position and centring point as the AP described here but with an obliquity of the patient at 45° instead of 20°, to open the glenohumeral joint. The view shows the glenohumeral joint tangentially, but published work varies in assessment of its effectiveness in demonstration of direction of dislocation.8–10
| Common errors | Possible reasons |
|---|---|
| Inferior end of the scapula not included on the image | The IR is often positioned in the ‘landscape’ position; putting it in the ‘portrait’ position will usually prevent this |
| Foreshortening of the clavicle | The patient is rotated too much towards the side under examination |
| The acromioclavicular joint is over-penetrated | This is due to the difference in subject contrast in this area; the use of a wedge filter will prevent this |
Axillary/axial projections of the shoulder
Evaluation of the shoulder joint, particularly for follow-up orthopaedic assessment, often requires an axillary projection to offer an image at 90° to the AP. Success of this projection will depend on the patient’s condition and cooperation. Two methods are described here: method 1 is often difficult to implement or inappropriate, particularly in trauma, owing to the extent to which the arm must be abducted. Method 2 is the method of choice for a patient with restricted movement of the humerus as there is more scope for adaptation to suit the patient’s condition. Method 2 is sometimes referred to as the Lawrence axillary.11
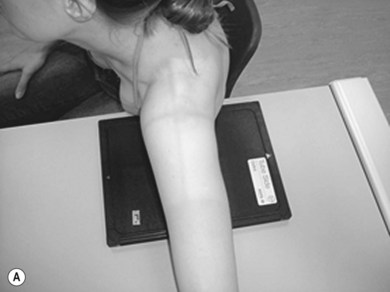
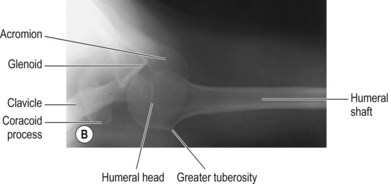
Method 1: superoinferior shoulder (Fig. 7.2A,B)
Positioning
• The patient sits with the side under examination next to and slightly away from the table
• For radiation protection purposes the legs are placed so they are not under the table and a lead rubber apron is worn around the waist
• The arm is abducted fully and the patient leans laterally over the IR; the hand is internally rotated and pronated. The axilla is positioned over the IR in a position that will ensure inclusion of the relevant anatomy, and with the axilla as close to it as possible
• The patient’s head and neck are abducted away from the shoulder under examination as far as possible to clear them from the area of interest and reduce the radiation dose to these areas
Criteria for assessing image quality
• Head and proximal end of humerus, glenoid fossa, lateral end of clavicle, acromion and coracoid process are demonstrated
• Head of humerus appears above the glenoid ‘like a golf ball on a tee’7
• Greater tuberosity should be seen in profile anteriorly
• Acromion and lateral end of clavicle are superimposed on the superoposterior aspect of the head of humerus
• Coracoid process is demonstrated anterior to the head of humerus
• Sharp image demonstrating the soft tissue margins, bony cortex and trabeculae of the head of the humerus with adequate image density to demonstrate the bony detail of the humerus in contrast to the glenohumeral joint, acromion and clavicle
| Common errors | Possible reasons |
|---|---|
| The glenohumeral joint is not demonstrated within the boundaries of the IR | The patient may not be stretching across the IR sufficiently. If the patient is capable of leaning further, try lowering the table-top to enable the patient to flex more at the waist |
| Magnification and unsharpness of the resulting image, probably accompanied by foreshortening of humeral head | The axilla is not in close enough contact with IR and the humerus may not be fully abducted, causing its shaft to lie at an angle with the IR. Try using a pad to raise the IR or consider increasing the FRD to compensate for the large ORD |
Method 2: inferosuperior shoulder; ‘Lawrence axillary projection’ (Fig. 7.3)
Positioning
• The patient lies supine on the table
• A small radiolucent pad is placed beneath the shoulder to raise it slightly
• The head and neck are abducted as much as possible away from the side under examination to clear them from the area of interest and reduce radiation dose to these areas
• The IR is supported in the erect position, its tube side against the superior aspect of the head of the humerus and in contact with the neck
• The arm is abducted to 90° or as far as the patient’s condition permits and the hand is supinated (although some internal rotation of the forearm is acceptable; supination acts mainly to help the patient maintain the correct relationship of the humerus to the IR)
• A lead rubber apron is placed over the patient’s chest and abdomen for radiation protection
This technique can be achieved with as little as 30° arm abduction,3 but the tube needs to be brought in as close to the patient’s body as possible. By lying the patient in a slightly diagonal position across the length of the table-top or trolley, access to the axilla is achievable (Fig. 7.4). Positioning the patient thus, diagonally across the table-top, requires consideration for the safety of the patient; this is directly related to table width and should only be considered in the relatively cooperative patient.
Beam direction and FRD (inferosuperior and modified inferosuperior projections)
Horizontal at 90° to the IR and coincident with the glenohumeral joint
Criteria for assessing image quality
• Head and proximal end of humerus, glenoid fossa, lateral end of clavicle, acromion and coracoid process should all be demonstrated
• Glenohumeral joint should be demonstrated
• Lesser tuberosity of humerus should be seen in profile
• Acromioclavicular joint will be superimposed on humerus
• Sharp image demonstrating the soft tissue margins, bony cortex and trabeculae of the head of humerus with adequate image density to demonstrate the bony detail of humerus in contrast to the glenohumeral joint
| Common error | Possible reason |
|---|---|
| The glenohumeral joint is not demonstrated within the boundaries of the IR | The head and neck may not be sufficiently abducted away from the side under examination to enable the IR to be positioned correctly. Always ensure the IR is closely tucked into the neck |
The inferosuperior projections can be adapted to demonstrate the classic Hill–Sachs compression fracture, seen in patients who have recurrent anterior dislocation of the shoulder.1 This adaptation involves maximum external rotation of the arm, with the patient aiming to press the thumb down towards the table or trolley top. Unfortunately, this manoeuvre can be difficult for patients to achieve and the AP shoulder with maximum internal rotation can also demonstrate this lesion adequately.2 In order to achieve the correct amount of rotation for this, the arm is medially rotated and flexed at the elbow; the dorsum of the hand is then rested on the waist. Yet another technique that can show Hill–Sachs lesions is the Stryker notch view, where the palm of the hand is placed on top of the head with the fingers toward the back of the head and the long axis of the humerus parallel to the median sagittal plane (MSP); a 10° cranial angle is centred over the coracoid process for this projection.12
Bankart lesions are also recognised as an effect of recurrent anterior dislocation13 and are best seen on the true superoinferior view; clearly, superoinferior is recognised as difficult on the traumatised patient but feasible on patients with recovered range of shoulder movement following treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree