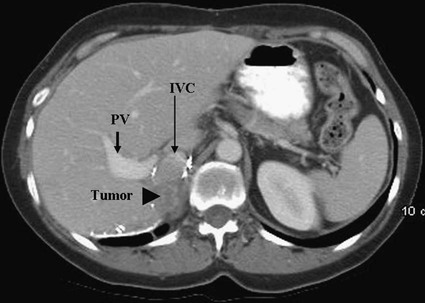
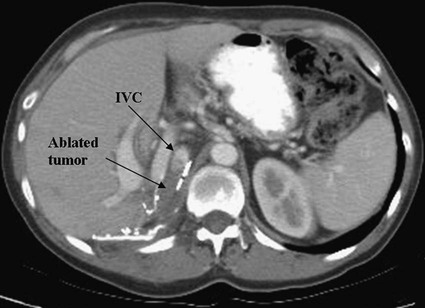
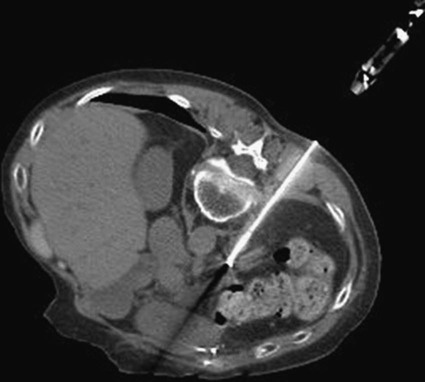
The primary treatment for adrenal gland tumors has traditionally been open or laparoscopic surgical resection. It has been suggested in a few small series that aggressive local surgical resection may improve outcomes in selected patients with isolated metastatic disease limited to one adrenal gland from nonadrenal primary tumors. Although controversial, this has been especially postulated for patients with solitary adrenal metastases and favorable tumor biology, long disease-free intervals, symptomatic disease, or specific histologic findings such as adenocarcinoma, lung carcinoma, renal cell carcinoma, colorectal carcinoma, or melanoma.1–3 In patients with adrenocortical carcinoma (ACC), there is stronger historical evidence that an aggressive surgical approach for recurrent and metastatic disease can improve survival.4 However, despite such measures, the 5-year survival rate in different series ranged between 16% and 38%, and recurrence rates of 35% to 85% after complete resection yield a poor prognosis.4–6 Adjunct therapy with mitotane, a synthetic derivative of the insecticide dichlorodiphenyltrichloroethane (DDT), has shown limited efficacy on the natural course of this disease.7,8 Newer therapies with cytotoxic chemotherapy are limited and under investigation.6 Besides the high morbidity associated with repeat surgical resections, which must be weighed against the benefits of such procedures, successive surgeries are further complicated by adhesions. However, image-guided radiofrequency ablation (RFA) may provide an alternative minimally invasive treatment option for patients who are not operative candidates and have multiple comorbid conditions, an aggressive tumor focus, and/or no other treatment options for local control of tumor. In addition to malignant adrenal disease, including pheochromocytomas, benign functioning lesions seen in patients with primary hyperaldosteronism secondary to an adrenal aldosteronoma may benefit from RFA, with its lower morbidity, shorter hospitalization, and less expense than open surgery.9 RFA can be performed for the treatment of primary and metastatic adrenal neoplasms, including ACCs, pheochromocytomas, adenomas, extraadrenal metastases from adrenal neoplasms, and palliation in selected cases. Surgical indications for adrenalectomy from solitary metastases can be found for specific histologic findings, including adenocarcinoma, lung carcinoma, renal cell carcinoma, colorectal carcinoma, or melanoma.1–3 Extrapolation to indications for RFA assumes that it is an alternate method for nonsurgical tissue destruction. Image-guided ablation can provide a safe treatment alternative for patients with painful lesions or symptoms related to catecholamine-producing neuroendocrine tumors.10 Tumor debulking by ablation can subsequently play a palliative role by the resultant decrease in catecholamine release. In addition, RFA has also been described in the treatment of primary hyperaldosteronism and metastatic pheochromocytoma.11,12 RFA can be used to treat lesions 5 cm in diameter or smaller. Larger lesions can be treated by overlapping ablations, but the success rate markedly diminishes as the size increases. Nonoperative candidates—those with high surgical risk, several comorbid conditions, unresectable tumors, multiple prior recurrent surgeries, and an aggressively growing tumor—can benefit from RFA in the appropriate clinical scenario. Patients with bilateral adrenal metastases may be well served by RFA for palliative purposes and in some cases may be treated for bilateral disease in a single sitting.13 • 200-W, 460- to 480-kHz alternating current RF generator • RF electrodes (single or cluster electrode) • 2 to 4 grounding pads or dispersive electrodes • Computed tomography (CT) and/or ultrasound guidance (microwave, cryoablation, high-intensity focused ultrasound equipment may also be used, although there is less historical experience) Thermal ablation of the adrenal gland can be performed from several approaches. When deciding which approach to use, the location of nearby organs, vessels, and nerves should be considered. Figures 151-1 and 151-2 show the intimate relationship of a right-sided adrenal tumor with the liver, portal vein, and inferior vena cava. In this instance, the close proximity of the tumor to a major vessel should warrant concern as to whether thermal ablation can be done successfully, owing to the large heat sink effect that may occur and result in inadequate treatment. Adrenal tumors are most readily accessible via a posterior or lateral approach with the patient in an ipsilateral decubitus position.14 Although the risk of ipsilateral lung injury and pneumothorax is minimized in the decubitus position, one must also take into account the organ shift that occurs with positioning. In Figure 151-3, the adrenal tumor of a patient in the prone position is near the abdominal aorta and loops of bowel. An appropriate treatment window must be selected to allow placement of the electrode without interference of the ribs and to prevent thermal injury to the nearby aorta and large bowel. Thorough planning and preprocedural imaging with multiphase contrast-enhanced CT or magnetic resonance imaging (MRI) with gadolinium can help with tumor staging and avoid intraprocedural complications. The following technical points must be considered: • Take into account organ shift when positioning the patient. • Always be aware of surrounding organ structures to prevent inadvertent thermal injury; consider a fluid blanket to protect bowel, pancreas, lung, kidney, diaphragm, chest wall (including intercostals nerves), and other adjacent structures • If hypertension develops during adrenal, renal, or lower liver thermal ablation, consider adrenal irritation or catecholamine release as a possible cause. • Ensure patient has received adequate premedication to prevent hypertensive crises during ablation of pheochromocytomas and other functional neoplasms. • Cauterize needle track to prevent tumor seeding and bleeding. Access sites very close to the edge of moving targets may add risk of organ laceration (Figs. 151-4 and 151-5
Thermal Ablation of the Adrenal Gland
Indications
Equipment
Technique
Anatomy and Approaches
Technical Aspects
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thermal Ablation of the Adrenal Gland