CHAPTER 92 Thoracic Aortic Aneurysms
Thoracic aortic aneurysms can result from a variety of causes. The underlying cause of a thoracic aortic aneurysm can typically be predicted by its location and morphologic features and by the age of the patient.1 Whereas the overarching goal of therapy remains similar (i.e., to prevent complications, notably aortic rupture), the nature, timing, and associated operative interventions can differ significantly according to the location and cause of the aneurysm. An example is that of the ascending aortic aneurysm, which by its location is associated with the additional considerations of whether to replace the aortic valve, to reimplant the coronary arteries, and to repair the arch vessels. In addition, assessment of global cardiovascular function is paramount in directing appropriate treatment strategy.
Thoracic aortic aneurysms are less common than their abdominal counterpart.2 Imaging plays a critical role in diagnosis, treatment planning (i.e., assessment of the need for intervention, urgency of intervention, and type of intervention), and postsurgical surveillance. Moreover, some complications, such as spinal cord ischemia, are germane to surgical repair of thoracic aortic aneurysms, and imaging can provide a road map that may allow prospective modification of surgical technique to reduce the chances of such complications.
THORACIC AORTIC ANEURYSM
Definition
The traditional definition of an aneurysm is dilation of a blood vessel wall so that the resulting caliber is 50% greater.3 This size-based definition does not account for morphologic characteristics such as focal saccular dilation of the aorta due to trauma, penetrating atherosclerotic ulcer, and infection. These scenarios require an “aneurysm mentality” because saccular aortic dilations are at particular risk for rupture and are thus also classified as aneurysms.
In true aneurysms, the dilation involves all layers of the blood vessel wall. False aneurysms (also known as pseudoaneurysms or saccular aneurysms) occur from disruption of one or more layers of the aortic wall.4
Prevalence and Epidemiology
Thoracic aortic aneurysms are less common than abdominal aneurysms, and the prevalence depends on the etiology (Fig. 92-1). Of note, aneurysms due to systemic arterial disease have less male preponderance and a more advanced age at presentation than abdominal aneurysms do, resulting in greater comorbid disease.2
The population incidence of detected descending thoracic and thoracoabdominal aortic aneurysms is estimated to be 5.9 new aneurysms per 100,000 person-years. The lifetime probability of rupture in these aneurysms is 75% to 80%.5
Etiology and Pathophysiology
Etiology and Pathogenesis
Atherosclerosis
Atherosclerosis affects the aortic wall in many ways, such as through erosion of the internal elastic lamina and subsequent exposure of the medial layer of the aortic wall to the pulse pressure or through ischemia of the media from reduced blood supply due to disease in the vasa vasorum. Another mechanism of aneurysm formation is through progression of atherosclerotic plaque ulceration to a penetrating atherosclerotic ulcer with breakage of the intimal layer. Penetrating atherosclerotic ulcer may result in a saccular aneurysm (Fig. 92-2). Atherosclerotic aneurysms are associated with hypertension, coronary artery disease, and abdominal aortic aneurysms.4
Cystic Medial Necrosis
As the name implies, cystic medial necrosis affects the medial layer of the arterial wall; degeneration of the smooth muscle creates “cystic spaces,” resulting in a fusiform aneurysm.4 This is the most common cause of aneurysms of the ascending aorta. The pathophysiologic process involves the aortic root, resulting in dilation of the annulus of the aortic valve. Associated aortic regurgitation may require concomitant replacement of the aortic valve.6 Cystic medial necrosis is the hallmark of the pathologic changes in Marfan syndrome (Figs. 92-3 to 92-6). Other connective tissue disorders, such as Ehlers-Danlos and Loeys-Dietz (Fig. 92-7) syndromes, also affect the medial layer of the aorta.4 These entities are both familial and have an identifiable gene leading to the abnormal biochemistry.
Marfan syndrome is the most common of the connective tissue processes, with an incidence of 1:10,000.7 Marfan syndrome is an autosomal dominant condition that results in a mutation in the gene encoding fibrillin 1,8 an essential protein for elastic properties, causing cardiovascular and musculoskeletal abnormalities. The elastin-depleted aorta is stiffer and more prone to dilation as it incurs higher pulse pressure than the normally distensible aorta does. The dilation starts in the root and extends to the mid-ascending aorta.9 Aortic rupture and dissection are the leading causes of death in patients with Marfan syndrome.7 Repair in patients with Marfan syndrome is recommended in the asymptomatic patient when the aortic root or ascending aorta exceeds 5 cm in diameter because of the high risk of aortic rupture and aortic dissection.10 Associated cardiovascular abnormalities include aortic insufficiency and mitral valve prolapse, which frequently necessitate valve repair, and pulmonary artery aneurysms.9
Loeys-Dietz syndrome has only recently been characterized as a distinct phenotype that is caused by mutations in genes encoding type 1 or type 2 transforming growth factor β.11 Aneurysms form at an earlier age than in other connective tissue disorders and tend to rupture at a smaller size, with a greater propensity for dissection. The arteriopathy tends to be more systemic than in Marfan syndrome, and the postoperative surveillance must factor both the repaired artery and the remote arteries including the intracranial circulation.
Vascular Ehlers-Danlos syndrome is an autosomal dominant disorder caused by heterozygous mutations of the COL3A1 gene. The syndrome is characterized by fragile arterial tissue that not only is prone to aneurysm, dissection, and rupture but can also make surgical repair difficult. Noninvasive imaging, such as computed tomographic angiography (CTA) and magnetic resonance angiography (MRA), is preferred because of the risk of dissection and rupture with arterial access. Unlike Marfan and Loeys-Dietz syndromes, which have a predilection for the aortic root, Ehlers-Danlos syndrome more often affects the visceral arteries.12
Dissection
Aortic dissection is different enough in pathogenesis and management to be considered separately from thoracic aortic aneurysms. The term dissecting aneurysm is discouraged. Nonetheless, a dissected aorta may become aneurysmal (Fig. 92-8), and an aneurysm may dissect; both scenarios alter the management and approach. Of note, any cause of an acute aortic syndrome can result in aneurysm formation.
Trauma
Blunt thoracic trauma with a sudden deceleration mechanism injures the aorta at its points of relative fixation (due to shear), which includes the aortic isthmus (in the region of the ligamentum arteriosum), the hiatus, and the aortic root, in descending frequency. Injury may cause transection or intimal disruption and, if unrecognized, may be manifested as a saccular aneurysm that may involve disruption of the intima and media (pseudoaneurysm or false aneurysm).13
Mild bulging of the proximal descending aorta at the attachment of the ligamentum arteriosum (ductus bump) is a common normal finding and should not be confused with aneurysms in that region, particularly those due to trauma (Fig. 92-9).
Inflammation and Infection
Infection may primarily involve the artery and secondarily lead to aneurysm, or an aneurysm may become infected. The most common site of infection is the ascending aorta near the sinus of Valsalva (Fig. 92-10).14 Infected aortic aneurysms, despite the pseudonym mycotic aneurysms, are rarely due to fungal agents and mostly caused by bacteria in an acute or chronic setting, classically due to syphilis.
Infected aortitis leading to aneurysms may occur by direct extension from endocarditis or seeding of the vasa vasorum with infected complexes from remote septic foci. These remote foci may not be clinically evident, and Salmonella and Staphylococcus are the most common etiologic agents in this situation. Predisposing factors include intravenous drug abuse and immunocompromised state.15
Vasculitides such as Takayasu arteritis and giant cell arteritis may lead to aneurysmal dilation, but mural thickening is the predominant finding in such inflammatory conditions. The mural thickening may lead to reduction in luminal caliber even if the adventitia-adventitia measurement indicates arterial enlargement.16
Post-stenotic Dilation
Aortic stenosis can cause dilation of the ascending aorta, usually the right lateral and posterior wall, from the post-stenotic jet. This is commonly seen in those with a bicuspid aortic valve (Fig. 92-11), although the dilation may be partly due to a systemic arteriopathy because this condition is also associated with coarctation of the aorta.17 Coarctation can also lead to post-stenotic dilation.
Location
Thoracoabdominal aortic aneurysms are further divided by the Crawford classification (Fig. 92-12), which is used to determine the operative approach and to counsel the patient about postoperative complications. Crawford I and II start distal to the origin of the left subclavian artery, with Crawford II extending below the renal artery origin. Crawford III starts more distal than Crawford I in the descending thoracic aorta. Crawford IV is essentially an aneurysm of the abdominal aorta that extends to the diaphragmatic hiatus.18
True and False Aneurysms
All causes of arteriopathy can cause true aneurysms. The causes of false aneurysms, on the other hand, are more typically trauma, infection (i.e., mycotic aneurysm), and penetrating atherosclerotic ulcer. False aneurysms have a saccular morphology, that is, an eccentric bulge, and can be considered a contained rupture (Fig. 92-13). They occur from the disruption of layers of the blood vessel wall and are often contained only by the adventitia and fibrous tissue. This makes them more likely than true aneurysms to rupture for any given size.1
Manifestations of Disease
Clinical Presentation
Aneurysms may be detected incidentally, be manifested through local mass effect or systemic symptoms, or cause symptoms from acute rupture.1,19
Rupture
The strongest predictor of rupture is the initial size of the aneurysm. Also, the etiology of the aneurysm must be taken into consideration as certain connective tissue disorders are associated with rupture at a smaller aneurysm size. For thoracoabdominal aortic aneurysms due to atherosclerosis, the rupture rate is 18% at 2 years for aneurysms greater than 5 cm. Another risk factor for rupture is aneurysm growth of more than 5 mm in 6 months. Aneurysm growth correlates with smoking, forced expiratory volume in 1 second (FEV1) of less than 1.5 L/ min, female sex, and advancing age.20 The diameter at which elective surgery on the ascending aorta is recommended is considered to be 5.5 cm.10 Ascending aortic aneurysms grow faster in association with a bicuspid aortic valve (0.19 cm/yr) than with a non–bicuspid valve (0.13 cm/yr).21

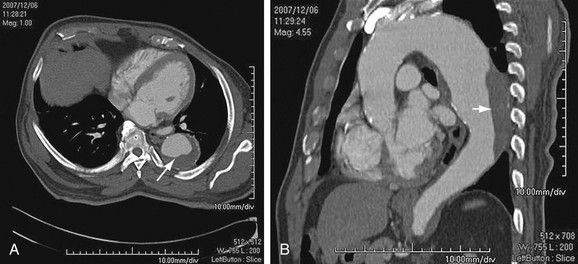
 FIGURE 92-1
FIGURE 92-1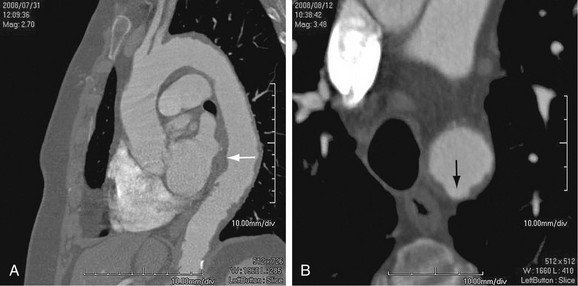
 FIGURE 92-2
FIGURE 92-2
 FIGURE 92-3
FIGURE 92-3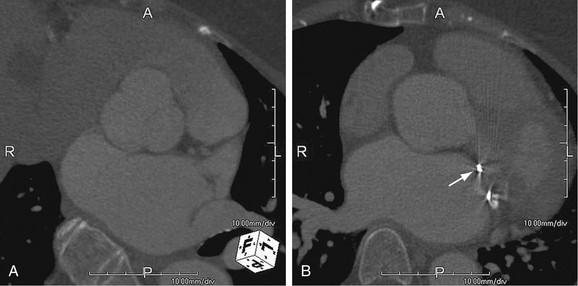
 FIGURE 92-4
FIGURE 92-4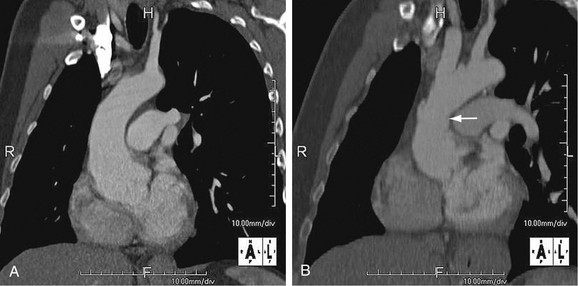
 FIGURE 92-5
FIGURE 92-5
 FIGURE 92-6
FIGURE 92-6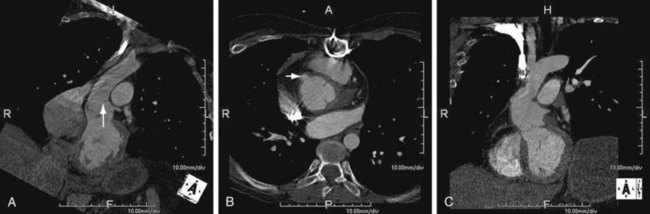
 FIGURE 92-7
FIGURE 92-7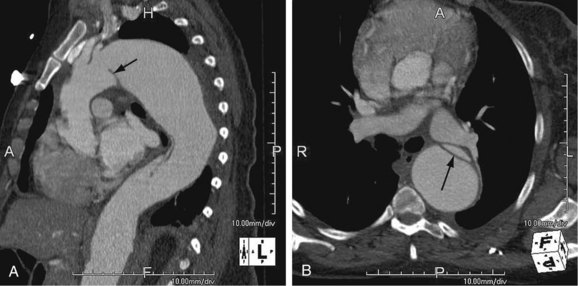
 FIGURE 92-8
FIGURE 92-8
 FIGURE 92-9
FIGURE 92-9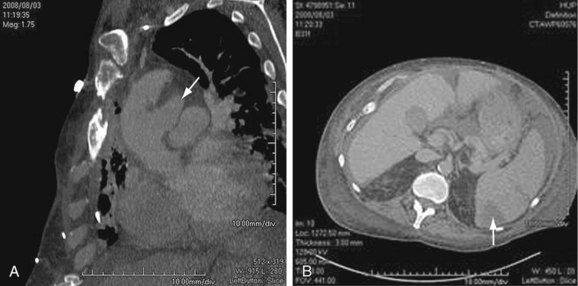
 FIGURE 92-10
FIGURE 92-10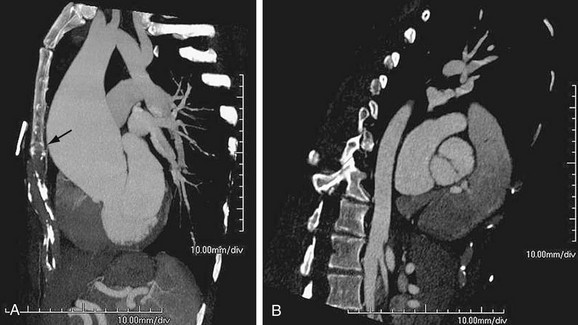
 FIGURE 92-11
FIGURE 92-11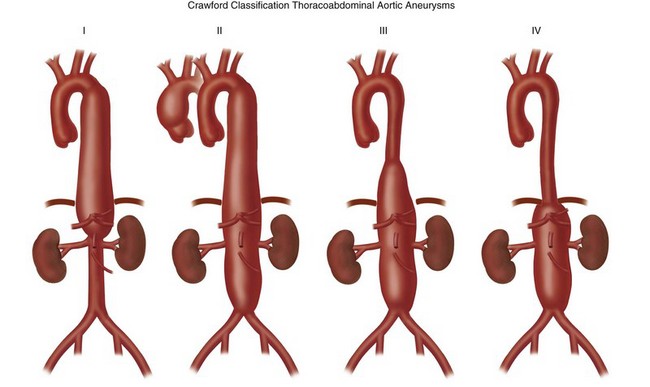
 FIGURE 92-12
FIGURE 92-12
 FIGURE 92-13
FIGURE 92-13

