CHAPTER 95 Thoracic Aortitis
Aortitis is often characterized by inflammation of the media and adventitia.1 Aortitis has many causes and may be related to autoimmune diseases or noninfectious causes as well as infection by microorganisms. Aortitis belongs to the group of diseases collectively known as the large-vessel vasculitides, as defined by the Chapel Hill Consensus Conference on the classification of systemic vasculitides.2 Regardless of the source, inflammation of the aorta often results in dilation of the aortic root and aortic insufficiency. As a consequence, aortic valve replacement with aortic root reconstruction is often needed. It can be divided into an acute inflammatory phase and a chronic fibrotic phase.
Classification can be based on whether the aortitis is inflammatory. Other classification systems are based on whether the cause is associated with antineutrophil cytoplasmic antibodies. The exact cause is often difficult to define with certainty (Table 95-1).
TABLE 95-1 Classification of Aortitis
| Infectious | Noninfectious |
|---|---|
| Syphilis |
Nonspecific aortic inflammation can also be seen in atherosclerosis. Because assessment of the vessel wall is critical in these patients, magnetic resonance angiography (MRA) or computed tomographic angiography (CTA) is preferred to conventional angiography. In general, inflammatory aortitis tends to affect the thoracic aorta rather than the abdominal aorta, whereas atherosclerosis affects the abdominal aorta.3
The more common diseases are discussed in this chapter.
TAKAYASU ARTERITIS
Definition
Takayasu arteritis was first described in 1908 by a Japanese ophthalmologist. This is a chronic vasculitis of unknown etiology affecting the aorta and its primary branches that can progress to ischemia or occlusion. The inflammation causes thickening of the walls of the affected arteries. The proximal aorta may become dilated secondary to inflammatory injury. Narrowings and occlusions are more common, but dilation of involved portions of the arteries can also result in myriad symptoms. Aneurysmal disease occurs in as many as 20% of patients,4 but mostly in the descending thoracic aorta (Table 95-2).
TABLE 95-2 Classification of Takayasu Arteritis by the American College of Rheumatology Classification Criteria*
* If three of six criteria are met, patients are said to have Takayasu arteritis.
Prevalence and Epidemiology
The majority of reported cases are in Asian patients, but there is a worldwide distribution. Women are affected in 80% to 90% of cases, with an age at onset between 10 and 40 years. In Japan, up to 150 cases occur per year,5 whereas there are about 1 to 3 new cases per year per million in the United States and Europe.6
Manifestations of Disease
Clinical Presentation
Usual presenting symptoms are systemic or constitutional—fatigue, weakness, arthralgias, weight loss, and low-grade fever—probably secondary to released cytokines. Vascular symptoms are rare at presentation; when they do develop, it is secondary to dilation or stenosis of the affected vessels. Classically, the disease is characterized by stenosis, but the incidence of aneurysmal lesions is increasing (30% to 50%).7 Patients may present in heart failure secondary to aortic dilation and regurgitation. Late-phase symptoms include diminished or absent pulses, bruits, hypertension, and heart failure (Fig. 95-1). Dissection is possible, but giant cell arteritis has a higher incidence.
Subclavian artery involvement is very common and often results in a blood pressure difference between the arms of more than 10 mm Hg. Lesions proximal to the vertebral artery may result in amaurosis fugax and subclavian steal. Up to 50% of patients have involvement of the pulmonary arteries.8 Pulmonary artery involvement can give rise to chest pain, dyspnea, hemoptysis, and pulmonary hypertension,9 but pulmonary function is generally not compromised despite extensive involvement, although unilateral pulmonary artery occlusion has been reported.10 Most frequently affected arteries apart from the aorta are subclavian (90%), carotid (45%), vertebral (25%), and renal (20%).11 Angina secondary to coronary ostial narrowing or coronary involvement is also possible. Affected arteries need to have vasa vasorum and are thus muscular, a feature lacking in peripheral arteries, which explains their lack of involvement in this condition. Patients may also present with abdominal pain, diarrhea, and skin lesions such as erythema nodosum and pyoderma gangrenosum.
Imaging Techniques and Findings
Ultrasonography
Ultrasonography can detect perivasculitis, a rim of soft tissue around a great vessel, hypoechoic on ultrasound examination. One problem is that wall thickening may be indistinguishable from atherosclerotic plaque (Fig. 95-2). Intravascular ultrasound may detect subtle wall changes not seen on other techniques.
Computed Tomography
CT is usually the preferred initial examination; one can see mural calcification, and early disease detection portends a better prognosis. CT is good for detection and surveillance of arterial mural thickening, which decreases after steroid treatment. Typically, a double-ring pattern (poorly enhancing ring centrally, with a well-enhancing outside ring) can be seen. Perivasculitis, a rim of soft tissue around a great vessel that is hypodense on CT (vessel wall edema; Fig. 95-3), can also be detected. CT can also assess aortic or aortic branch vessel stenoses. The downside is ionizing radiation, especially in follow-up scans, as well as the need for iodinated contrast material, but it is a fast technique.
Magnetic Resonance
MR can detect mural thickening. It can also detect perivasculitis, a rim of soft tissue around a great vessel, along with aortic valvular thickening and pericardial effusion. Wall enhancement can be seen as an indicator of disease activity, secondary to edema and inflammation. Mural edema is seen as elevated T2 signal. Studies have shown reduced wall enhancement on follow-up, presumably secondary to reduced inflammation.12 Three-dimensional MRA does have decreased sensitivity for small vessels in comparison with conventional angiography (Figs. 95-4 and 95-5). One can do cine sequences to detect aortic regurgitation. Maximum intensity projection images should be used with caution because they can exaggerate the degree of vascular stenoses. Whereas MR is a longer examination, it benefits from its lack of ionizing radiation exposure, a feature preferable for long-term surveillance of Takayasu arteritis, which typically affects younger women.
Nuclear Medicine/Positron Emission Tomography
Increased uptake of fluorodeoxyglucose (FDG) in regions of the aorta corresponds to abnormal regions on MRI.13 Positron emission tomography (PET) should be able to distinguish mural thickening secondary to active inflammation from scar formation and can be used to assess response to treatment (Fig. 95-6).

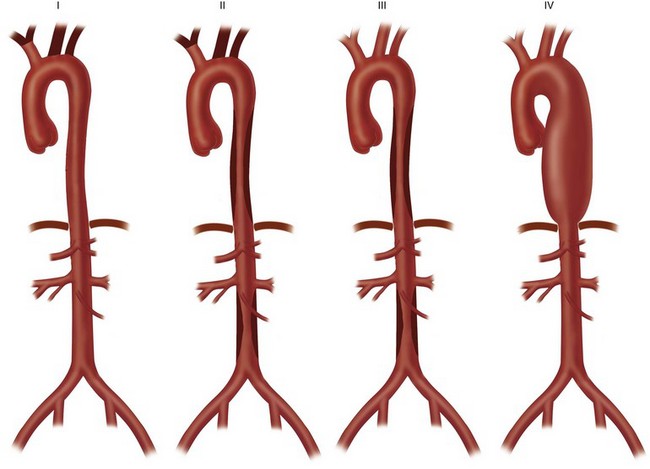
 FIGURE 95-1
FIGURE 95-1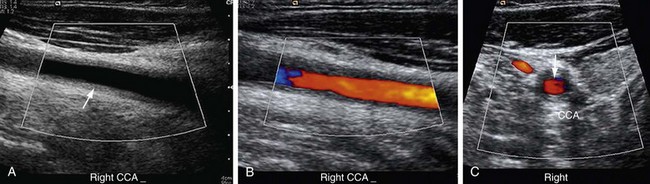
 FIGURE 95-2
FIGURE 95-2
 FIGURE 95-3
FIGURE 95-3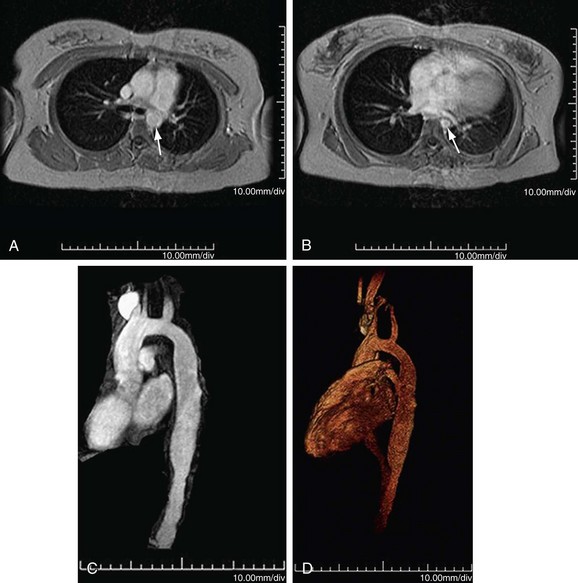
 FIGURE 95-4
FIGURE 95-4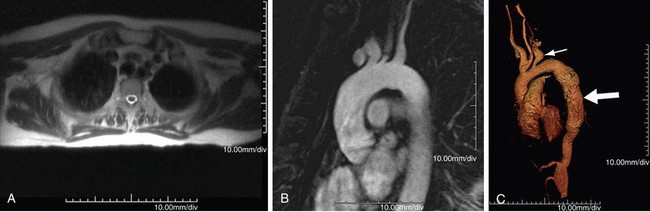
 FIGURE 95-5
FIGURE 95-5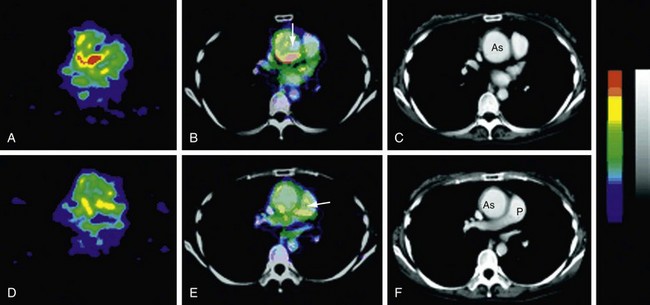
 FIGURE 95-6
FIGURE 95-6

