Chapter 22 Thoracic Interlaminar Epidural Steroid Injection, Paramedian Approach
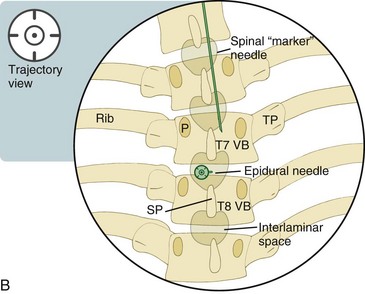
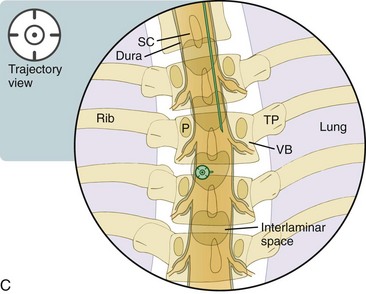
For thoracic interlaminar epidural injections, advancing the epidural needle in the lateral or contralateral oblique view provides a safe approach into the epidural space not offered by traditional AP only views. The contralateral oblique view allows for an alternative approach to the interlaminar space when it is otherwise not evident with AP imaging (see Chapter 3). This technique identifies the interlaminar space by optimizing the visualization of the laminae that border the space. This is accomplished via the radiologic superimposition of the laminar structures at an oblique angle, which produces an elliptical appearance of the laminae. The interlaminar space is easily identified in between the elliptical-appearing cranial and caudal laminae. The epidural needle is advanced through the space and beyond the spinolaminar line to engage the ligamentum flavum. The epidural space is then identified after the use of a loss-of-resistance technique with air, saline, air and saline, or the hanging drop technique. The use of saline is preferred to an “air only” technique in order to avoid a seizure or cord compression from an inadvertent subarachnoid injection of air.
Note: Please see page ii for a list of anatomical terms/abbreviations used in this book.
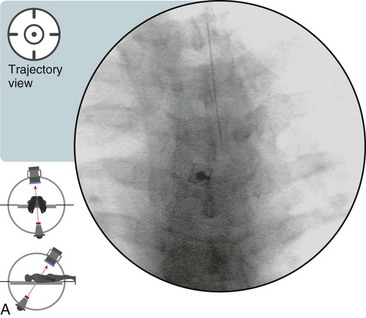
 Trajectory View (Figure 22–1)
Trajectory View (Figure 22–1)
The injection level is confirmed with the AP view.
The needle is placed parallel to the fluoroscopic beam with the use of this trajectory approach.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree