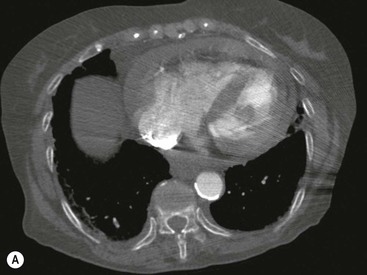
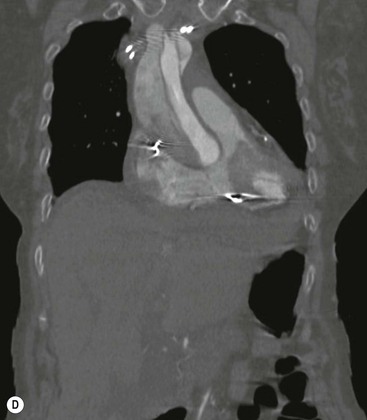
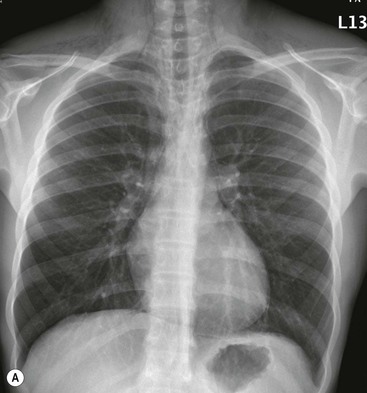
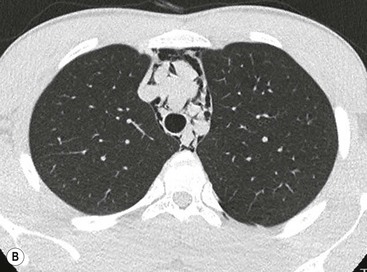
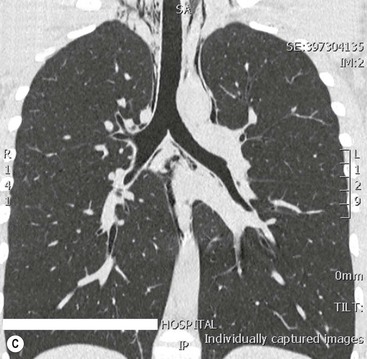
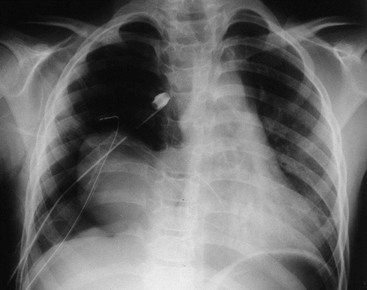
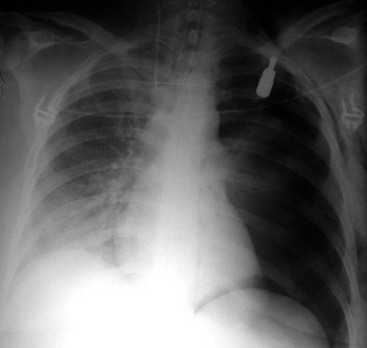
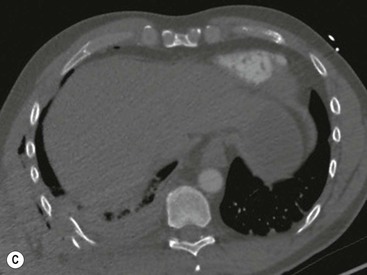
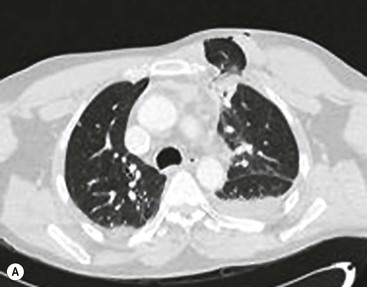
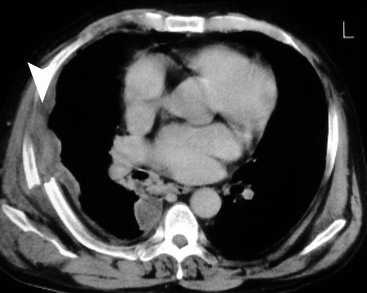
John H. Reynolds, Hefin Jones The thorax contains the organs most essential to basic life, namely the heart, lungs and the largest and most important of the blood vessels. The alveoli of the lungs allow exchange of oxygen and carbon dioxide and the heart and great vessels circulate nutrients, oxygen and carbon dioxide to and from all organs and tissues. Traumatic injury to these structures, more than many others, can precipitate death and extra-thoracic organ injury. Even relatively minor injuries to the chest’s musculoskeletal system can lead to morbidity, such as hypoventilation and subsequent pneumonia, secondary to rib fracture. In developed nations, trauma is the leading cause of death in the under-50 age group, of which 20% are directly related to thoracic injuries and up to 50% may be indirectly related to thoracic injuries.1 Significant thoracic trauma, requiring hospitalisation, is thought to have an incidence of 4 per million per day worldwide.2 Major thoracic trauma rarely occurs in isolation and other areas of injury may be present, particularly in the head, spine, abdomen and pelvis. The main cause of chest trauma is road traffic collisions (RTC) (75%); violent assault and falls are other relatively common aetiologies but with slightly different patterns of injury.3 Major trauma patients are assessed and treated according to the Advanced Trauma Life Support (ATLS) protocol,3–6 which assumes a trimodal pattern of mortality, with peaks at the time of the incident, after several hours and delayed (>1 week); the protocol was designed to reduce patient mortality in survivors of the initial injury. The initial (primary) radiological assessment includes an anteroposterior (AP) chest and AP pelvic plain radiograph but in many trauma centres, if a major injury is suggested and the patient is relatively stable, these plain radiographs may be omitted with the patient undergoing a ‘trauma series’ multidetector computed tomography (MDCT) examination.7 Experience gained in dealing with military casualties has provided a challenging cohort of patients and has helped evolve civilian medical practice in emergency departments, aided by developments such as helicopter retrieval and emergency transfer and the development of regional ‘Level I’ trauma centres in many developed countries (RCR). With advanced paramedical practice, many patients will arrive at the hospital intubated and will sometimes have prophylactic chest drains inserted, particularly if transferred via helicopter, and the primary survey will have often been completed prior to arrival. Focused assessment with sonography for trauma (FAST) can be performed in transit and with competent operators; this can also detect the presence of pleural and pericardial fluid before arrival in the emergency department.8 Once in the trauma centre, fast helical MDCT is the most useful imaging investigation in the acute setting, given its rapidity, availability and familiarity by the interpreting radiologist. Full anaesthetic and monitoring equipment can now be found in most emergency CT units, allowing even relatively unstable patients the opportunity for acute diagnostic CT. Cardiac-gated CT does reduce movement artefact of the heart and thoracic aorta but its benefits are not yet thought to outweigh the complexities of acquisition in the acute setting, particularly as there may be a decrease in image quality for assessment of lung and bone injury.9 In cases of diagnostic uncertainty, repeat cardiac-gated CT or MRI can be performed when the patient has stabilised. Protocols vary but all should include an unenhanced CT head and a contrast-enhanced thorax and abdomen, including full spine and pelvic imaging.10 Some trauma centres advocate a two-phase intravenous contrast-enhanced single CT data acquisition from the skull base to mid-femur, with more dilute contrast seen in the portovenous phase and a delayed high concentration contrast agent injected later, providing an arteriographic image within the same examination. Further advances include the use of radiolucent spinal boards or higher kilovoltage (kV) techniques to avoid the need to unnecessarily move patients with suspected spinal injuries.10 A disadvantage of modern CT is the large number of images for the radiologist to review with the potential for subsequent delay in provision of report. One solution is for the radiologist to complete a quick provisional proforma, with ‘tick-box’ entry for each injury-free body part and space for a brief description of any injuries seen, a copy of which is given to the emergency physician within 15 min, allowing early decision-making regarding immediate procedures or surgery. Subsequent, less pressured and more detailed analysis of the images can then take place in preparation of the final report.10 Radiation doses can be of concern, particularly if there is poor patient selection but a well-protocolled single CT can prevent repeated attendances for plain radiography or angiography.11 Recent evidence suggests that due to modern, urban implementation of ATLS guidelines and an increase in availability of access to acute CT imaging, the previously recognised trimodal mortality pattern may be changing.12 Thoracic injury can be broadly divided into blunt and penetrating but in any individual, one or both types can be present. Blunt trauma imparts kinetic energy to the point(s) of impact, causing both direct damage at these and at more distant sites. Shearing injuries can occur in sudden deceleration, for example, such as at the aortic isthmus, the right main bronchus or within the lung parenchyma. Penetrating trauma, such as knife, gunshot or shrapnel, also imparts kinetic energy into the tissues involved. The kinetic energy imparted is related to the square of the projectile velocity, which illustrates why high-velocity missiles, such as rifle bullets and shrapnel, are associated with more injury than their mass alone would suggest. Penetrating missiles are associated with both a permanent cavity and a surrounding temporary cavity formation, created by the shock wave of impact, proportional in size to the velocity of the projectile. This temporary cavitation causes more damage in less elastic tissues, such as liver, than in the lung parenchyma. An appreciation of this, often initially occult, penumbra of damage is vital to understanding the likely outcomes of differing injuries. Further injury can be caused by fragmentation of the missile, external armour or bone fragments, dispersing velocity but increasing the area of injury and number of projectiles.13 If the missile passes through the air-filled cavity of the lungs, and does not come into contact with a solid organ, in particular, bone, then there is a high chance of the projectile not being retained. Even so, entry and exit points may be visualised by ‘smears’ of lead remaining at hard surface borders, such as bone, suggesting a likely trajectory.14 Given its high density and radiographic attenuation, even the smallest traces left may be seen on CT. The estimated trajectory can suggest structures, such as nerves, which may have been damaged but not clinically apparent in the unconscious patient. Sometimes the site of entry wound is clinically apparent but radiographically occult, particularly an issue with long sharp weapons, such as stilettos and screwdrivers, and one solution is to ensure a radio-opaque marker is applied to the dressing overlying each suspected entry wound. A retained projectile of high-attenuation material leads to ‘beam-hardening’ artefact, which can make visualisation of surrounding injury difficult. Techniques such as high kV CT and altering the angle of acquisition, either in relation to gantry or by position of patient, may be of value in this situation. Similar problems of ‘blooming’ are encountered with magnetic resonance imaging (MRI), and although most bullets are composed of lead, and sometimes copper, thus ostensibly MRI compatible, their pathway may include non-MRI compatible material, particularly when there has been fragmentation. Ultrasound can be used for peripheral objects, to assess musculoskeletal damage and can be used for a quick estimation of injury but often is unable to confidently aid initial diagnosis otherwise. Superficial wound- related collections are a major cause for re-imaging the septic patient and such collections can be easily assessed using ultrasound. This also allows imaging, and where necessary drain insertion, to be performed in the ICU setting. A further type of injury is blast injury, caused by sudden, rapid pressure changes in either air pressure or transmitted through water to submerged areas of the body, usually as a result of an explosion. This is associated with marked damage at the air–tissue interface with air blast injuries, causing alveolar, bowel and tympanic rupture. Although the pressure wave rapidly dissipates with distance from explosion, it may be funnelled or amplified in enclosed spaces and should be considered in any indoor explosion injury.15 Generally, however, those patients more than 6 metres from the explosion source at time of injury are unlikely to suffer from significant blast injury.16 Those patients with less severe clinical presentations and those too unstable for CT should undergo plain radiography in the ED resuscitation room as part of standard ATLS procedure and be assessed for immediate surgery or subsequent CT when resuscitated. All major traumatic presentations, stable enough to attend CT, should directly undergo trauma series CT.10,17 It seems prudent to seek those injuries likely to cause most serious and immediate morbidity and mortality to the patient. This requires analysis of the heart, looking for signs of cardiac injury, pericardial effusion and the more serious finding of traumatic cardiac tamponade. This is not specific for cardiac injury, as aortic root injury can also lead to this finding. Assessment of the remainder of the mediastinum should seek evidence of mediastinal haemorrhage, in particular related to aortic injury, and the aorta should be assessed from root to below the diaphragm. Mediastinal displacement or compression by tension pneumothorax can cause haemodynamic compromise and it is this, rather than the pneumothorax itself, which represents the most immediate danger. Rapid enlargement can occur under positive pressure ventilation, leading to acute deterioration, resistant to alteration in tidal pressures. Tracheobronchial injury is relatively rare and is either seen directly or suggested by a combination of pneumothorax and pneumomediastinum. Lung parenchymal opacification is likely to represent pulmonary contusion and this may initially obscure the more serious injury of pulmonary laceration. Pulmonary contusion is usually associated with rib fractures, which generally serve as an indirect marker of further thoracic and extra-thoracic injury, rather than significant injuries in themselves. One important finding is of multiple fractures in three or more contiguous ribs, resulting in a ‘flail chest’, associated with marked contusion, atelectasis and impaired ventilation, with associated increased mortality. Diaphragmatic injuries can be often overlooked but their diagnosis and subsequent repair can prevent later bowel strangulation.18 Herniated stomach can be misdiagnosed as pneumothorax and attempted chest drain insertion can result in contamination of the pleural space. Spinal injury should be assessed both for direct consequences and as a marker of severe thoracic injury, particularly when associated with sternal fracture. Thoracic injury patterns can be suggestive of occult abdominal and neck injuries. In particular, diaphragmatic involvement is commonly associated with splenic and hepatic injury. The myocardium is more commonly affected by blunt rather than penetrating trauma, in those patients still alive on arrival to hospital. As with all blunt chest trauma, RTCs account for the vast majority but specific injuries to the heart include cardiopulmonary resuscitation. Injury occurs usually due to crushing or deceleration but cardiac damage can occur due to overdistension due to excessive hydrostatic pressure, and this, combined with a reduced myocardial mass and anterior position, is likely to explain the increased incidence of right atrial and ventricular rupture.19 Injuries can range from asymptomatic contusions and arrhythmias, to coronary artery injury, regional wall motion abnormalities, pericardial tears, papillary rupture and valve dysfunction, with the most severe septal and free wall rupture seen as perimortal findings. Acute imaging with CT may only show a pericardial effusion or haemopericardium—suggested by a higher attenuation effusion (Fig. 17-1A). It may be possible to demonstrate a focal area of hypo-enhancement of myocardium, representing contusion, but this may not be appreciated on non-cardiac-gated studies. The major differential is myocardial infarction and clinical features, ECG and biochemical markers are similar for both entities. Given a suitable history of trauma, hypotension, cardiac contusion should be suspected, particularly with evidence of mediastinal injuries or sternal fracture. Cardiac-gated CT can be performed once the patient is stable and this can demonstrate presence or absence of coronary artery occlusion. Pericardial injury is usually associated with increased pericardial fluid, with even small effusions well demonstrated on CT. Pneumopericardium is an important sign of pericardial injury and differentiated from pneumothorax by its extent limited to the reflections at the roots of the great vessels. Cardiac herniation is referred to as luxation and this can be associated with torsion of the great vessels and represents the most important, if rare, complication of pericardial injury (Fig. 17-2). Sudden increases in endocardial pressure can result in traumatic papillary muscle, chordae tendinae and mitral valve leaflet tears. Increased intra-aortic pressure can cause injury to the aortic valve, with consequent aortic regurgitation. These valvular injuries may present immediately or after several years.19 The majority of cases of acute traumatic aortic injury (ATAI), around 80%,20,21 occur as a result of RTCs. ATAI is present in 0.5–2% of all non-fatal RTCs and accounts for 10–20% of all high-speed deceleration fatalities.22,23 In a recent Scottish study, 4% of blunt ATAI cases were dead on arrival and 19% died during triage; 68% were unsuitable for repair, with a mortality of 65%; 28% underwent open aortic repair and 4% underwent endovascular repair, with similar mortality rates of between 18 and 19%.21 Studies have suggested mortality rates of up to 94% within 1 hour and 99% at 24 hours, if untreated.20 This emphasises the importance of early diagnosis and appropriate patient triage.24 The majority of ATAI cases seen on imaging are located at the aortic isthmus, around 2 cm distal to the origin of the left subclavian artery. Other sites such as the aortic root (5% of clinical cases) and distal aorta (1% of clinical cases) are seen more frequently in post-mortem series due to the high mortality in injury at such sites. An aortic root disruption, for example, may lead to rapid death due to exsanguination, pericardial haemorrhage and tamponade, or myocardial infarction. The isthmic preponderance is thought to be related to multiple factors, including relative tethering at this site by the ligamentum arteriosum. Tethering is also thought to contribute to the increased numbers of injuries to the aortic root (5%) and as the aorta crosses the diaphragm (1%). The mechanism of injury is thought to be multifactorial. A major factor is thought to be the relative movement of the heart and relatively mobile aorta arch relative to the more tethered descending aorta. ‘Osseous pinch’ is a term used to describe the mechanical compression of the aortic arch and branch vessels between the thoracic spine and the sternoclavicular junction. Increased intravascular pressure within the aorta, also known as the ‘water hammer’ effect, as a direct result of compression, has been suggested to cause injuries at the isthmus and root.18,22 Injuries may be divided into transections and non-full thickness tears, the latter being more commonly seen in survivors, as transections result in rapid exsanguination. Tears commonly involve the intima and media, leaving the adventitia intact but with overall weakening of the aorta and at risk of subsequent rupture and pseudoaneurysm. The chest radiographic signs are related to the associated mediastinal haematoma and include: mediastinal widening, with a ratio of >25% of the chest width being a useful guide; blurring of the contours of the aortic arch and loss of definition of the aortopulmonary window; left apical pleural fluid; deviation of the trachea or NG tube; and widening of the paratracheal stripe and paravertebral contours (Fig. 17-3). However, given the relative poor negative predictive value of the chest X-ray, upon which 7% of ATAI may be occult, any abnormality, in the presence of a likely history, should be further investigated, usually with contrast-enhanced MDCT, particularly as ATAI only rarely occurs in isolation.25 MDCT for ATAI has sensitivity and specificity around 98% and is generally considered the gold standard and first-line investigation.22 Direct CT signs of ATAI includes intimal flaps, pseudoaneurysms and contained ruptures, an abnormal aortic contour and a sudden change in aortic calibre (pseudocoarctation).26 True traumatic dissection is less common but is seen (Figs. 17-1B–D). The presence of mediastinal haematoma but with well-defined aortic borders should be assumed to represent non-aortic bleeding from small mediastinal veins. Periaortic haematoma, without evidence of other aortic injury, should be assumed to be due to occult intimal injury and should be followed up with further imaging depending on the patient’s status. The term minimal aortic injury has been used to describe these lesions and those of intramural haematoma and intimal thrombus. Repeat CT aortography, MR aortography or transoesophageal ultrasound should be considered over the subsequent few days but there is no consensus as to the importance of these minimal aortic injuries. The role of diagnostic catheter angiography in these cases is limited in the acute setting, as it is estimated that 50% of these injuries are not detected via this technique.27 Some centres advocate the use of intravascular ultrasound for these indeterminate abnormalities, particularly as a problem-solving adjunct to CT.28 In all cases multiplanar reformat (MPR) review should be performed, as the signs are often subtle and difficult to appreciate on axial imaging. Further difficulties arise from cardiac motion, particularly affecting the ascending aorta, which can falsely suggest intimal flap formation and from anatomical variants, such as infundibula at the origins of the branch vessels. Most centres would not require a subsequent catheter aortogram before surgical treatment and this would now be performed only as part of endovascular repair. Pneumomediastinum occurs in up to 10% of cases of blunt chest trauma, most commonly as a result of alveolar rupture, either due to trauma or positive pressure ventilation, with peribronchovascular tracking of the air into the mediastinum. Rarely, pneumomediastinum may occur as a result of tracheobronchial or oesophageal disruption. Findings on chest X-ray are of a lucency outlining the mediastinum and its structures, often extending into the neck, features better demonstrated with CT29 (Fig. 17-4). Trachiobronchial injury is seen in up to 2% of blunt chest trauma,30 mainly bronchial, right-sided and within 2.5 cm of the carina, and is associated with an overall mortality of around 30%.31 The proposed mechanism is of increased intrathoracic pressure, against a closed glottis.17 Direct signs are of trachiobronchial disruption, with surrounding extra-luminal gas.30 Indirect signs are of pneumomediastinum, and, pneumothorax, which is classically resistant to treatment with a chest drain. The ‘fallen lung sign’, where the lung parenchyma is displaced dependently indicates a complete rupture of (usually the right) main bronchus18 (Fig. 17-5). Traumatic oesophageal rupture is mostly iatrogenic in origin and may provide only indirect evidence of its presence, via pneumomediastinum and a left-sided pleural effusion. The use of oral water-soluble contrast agent will reveal the presence and site of rupture on either CT or fluoroscopic examination in over 90% of cases, allowing for prompt treatment to avoid development of mediastinitis, which is associated with greatly increased mortality.32 Pneumothorax occurs in 30% of all chest trauma and although it may be caused by increased intrathoracic pressure causing alveolar rupture into the pleural space, it is most commonly caused by either a foreign object or fractured ribs lacerating the pleural surfaces. A tension pneumothorax occurs when there is a ‘flutter valve’ allowing unidirectional flow of air into the pleural space, resulting in an increasing volume and pressure of pleural gas. This can result in displacement of mediastinal structures, leading to cardiovascular compromise which is a clinical emergency. Features on imaging reflect this displacement and can be identified on ‘scout’ views before formal CT. The phenomenon of the occult pneumothorax arises from the inherent difficulties of interpreting the supine chest radiograph, where the pleural gas accumulates in the unfamiliar, anteromedial aspect of the pleural cavity. One study demonstrated an occult pneumothorax rate of 55%.33 Signs on the supine chest radiograph include a deep costophrenic sulcus, hyperlucency over the hemidiaphragm and an abnormally well-defined mediastinal or cardiac border (Fig. 17-6). CT has a sensitivity and specificity for pneumothorax of almost 100%, with the only diagnostic difficulty arising from differentiating pneumomediastinum from medial pneumothorax, when identification of the mediastinal septation is key. Communication across the chest wall of the pleural space and the extra-corporeal space can lead to a specific type of pneumothorax, colloquially referred to as a ‘sucking chest wound’. This arises from the flutter-valve effect occurring through the chest wall. On CT, this type of injury can be suggested by the presence of a large pneumothorax, resistant to chest drain insertion and evidence of a chest wall defect or large penetrating wound. Haemothorax can be found in around 50% of all chest trauma, with the haemorrhagic source ranging from ribs, intercostal vessels, lung parenchyma, great vessels or heart and pericardium. Arterial haemothorax can accumulate rapidly and cause both lung collapse and haemodynamic compromise. The supine chest X-ray may only show increased opacification of the affected hemithorax or a subtle lamellar effusion. On CT, haemorrhage can be identified by its increased attenuation (i.e. greater than 30 HU) compared to water and may even demonstrate layering of blood products. Careful inspection of the great vessels, branch vessels and pericardium should be performed in the presence of a haemothorax. Chylous pleural effusions usually occur secondary to penetrating injury and thoracic surgery. Features on imaging are of evidence of penetrating trauma in the region of the thoracic duct and a pleural effusion. The most common parenchymal injury is of pulmonary contusion, seen in up to 70%.34 It occurs primarily at sites of change in tissue density, such as adjacent to the thoracic spine, ribs or heart (Fig. 17-7). There is often a delay of up to 6 hours before the contusion may manifest itself on chest radiograph, although immediate detection is possible with CT. Consolidation should become maximal before 24 hours and resolve within 3–10 days. Opacification that appears after 24 hours or fails to resolve as expected, may be related to infection, aspiration, fat embolism or acute respiratory distress syndrome (ARDS). Pulmonary laceration is a more severe injury, which results from compression, shearing or penetration. The lung tissue undergoes elastic recoil, creating a space, which can fill with air, creating a pneumatocele or with blood, creating a pulmonary haematoma. Both are more clearly demonstrated on CT and may initially be occult on the chest radiograph due to surrounding contusion (Figs. 17-8 and 17-9). Lung herniation is a rare consequence of chest trauma, where lung parenchyma herniates through a defect in the chest wall, such as in multiple comminuted rib fractures. Generally, it can be treated conservatively but its diagnosis is important as the volume of herniated tissue can increase with positive pressure ventilation (Fig. 17-10). The term ‘blast lung’ describes a condition seen in survivors of near-proximity explosions in which there is an acute lung injury causing alveolar rupture and haemorrhage that may manifest itself as large air embolism or pulmonary oedema/haemorrhage. The classic blast lung characteristics are those of hypoxia, respiratory distress and haemoptysis, radiologically manifested as bilateral diffuse pulmonary infiltrates, in a butterfly pattern on the chest radiograph.35 Delayed lung injury may have a similar picture to acute respiratory distress syndrome,36 but it is thought that any lung injury should be apparent within 2 hours and delayed deterioration is rare.37 The pleura and mediastinum may be disrupted and contain air or blood and the chest wall and spine may be injured by blast debris fragments. Rib fractures are common in chest trauma, occurring in around 50% of patients but around half of these are likely to remain unidentified on the chest radiograph due to superimposition and tangential orientation. Solitary rib fractures are not of direct acute concern but can be indicative of further occult injury. Of more concern are multiple fractures in three contiguous ribs, creating a section of chest wall which can move in a paradoxical manner, in relation to the surrounding chest wall. This is related to hypoventilation of the underlying lung, is indicative of likely parenchymal contusion, increased mortality, and increased likelihood of requiring surgical treatment.38 Rib fractures may be associated with haemothorax or more localised extra-pleural haematoma (Fig. 17-11). Injuries to the most superior three ribs are associated with severe trauma and, specifically, injury to the brachial plexus, subclavian vessels, trachea and spine.39 Scapular fractures serve as a similar indirect marker of severe trauma. Injuries to the inferior four ribs are associated with visceral injuries to the upper abdomen, left-sided with splenic and right-sided with hepatic.18 Rib fractures in children are rare and the possibility of non-accidental injury should be considered, particularly if the posterior aspects are involved. Children and adolescents demonstrate a greater elasticity in their ribs and subsequently may have more severe internal thoracic injuries, in the absence of rib fractures.18 Sternal fractures are associated with increased cardiac and ascending aortic injury17 and sternoclavicular joint dislocations, particularly the less common posterior dislocation, are associated with injury and compression of the brachiocephalic vessels. Spinal fractures are not only of consequence to the spinal canal and surrounding neural structures, where 62% will be associated with a neurological deficit,40 but are also an indicator of severe trauma. Spinal fractures are commonly occult on plain radiographs and, if suspected, CT should be performed to assess further.40 The diaphragm can be injured by both penetrating and blunt trauma, particularly abdominal blunt trauma, due to a sudden increase in intra-abdominal pressure. This usually leads to a radial tear in the weaker, posterolateral tendinous insertion. Left-sided tears are more commonly seen on imaging and in surgical practice41 and this was thought to be due to a ‘protective’ effect of the liver but autopsy series have demonstrated an almost equal distribution of rupture and it seems that the right-sided defects are not identified or appear to be clinically less important.18 Penetrating defects are generally associated with either upper abdominal or chest wall injuries and are suggested by these injury patterns and the likely trajectories. Up to 70% of diaphragmatic ruptures are missed on initial assessment and prompt surgical repair is essential to avoid subsequent bowel herniation, strangulation and rupture, with an estimated 30% mortality from delayed diagnosis.42 Chest radiographic signs may be delayed in appearance but include loss of clarity of the diaphragm, herniation of abdominal contents into the chest and displacement of the mediastinum away from the affected side (Fig. 17-12
Thoracic Trauma and Related Topics
Thoracic Trauma
Introduction
Types of Injury
Diagnostic Approach
Specific Thoracic Injuries Following Trauma
Heart
Acute Traumatic Aortic Injury (ATAI)
Mediastinum
Pleura
Lung Parenchyma
Chest Wall
Diaphragm
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Trauma and Related Topics
Chapter 17