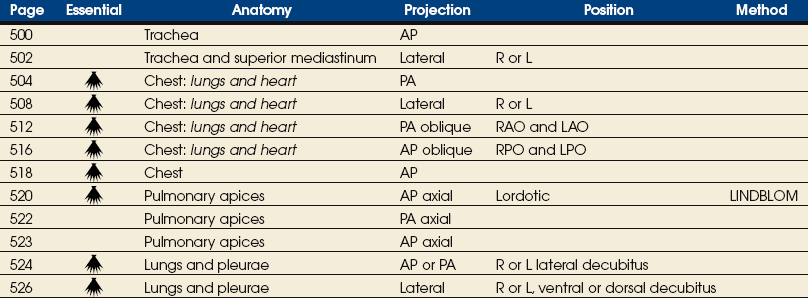
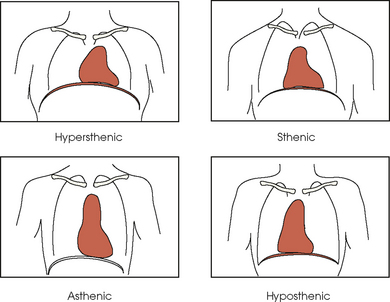
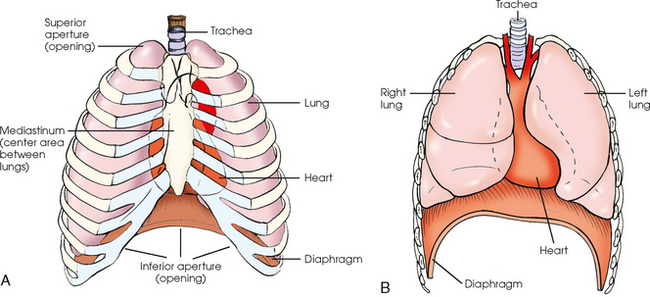
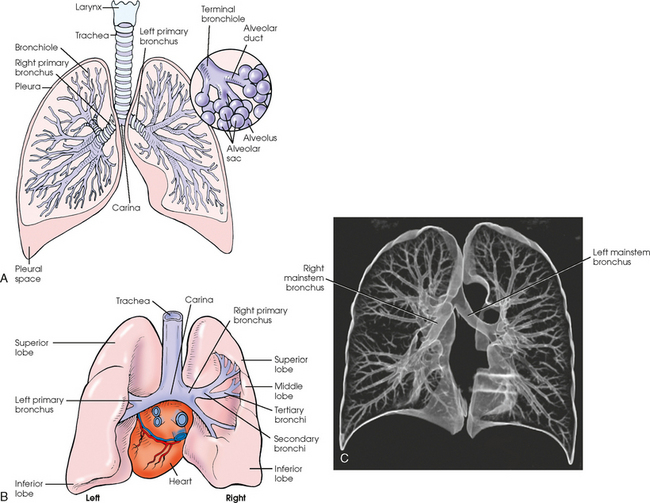
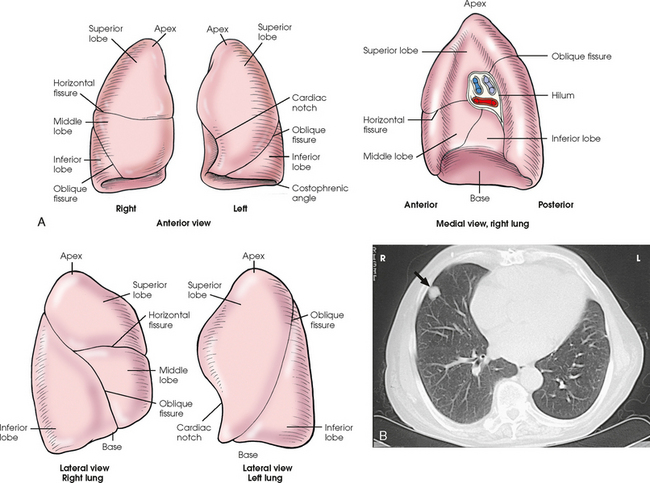
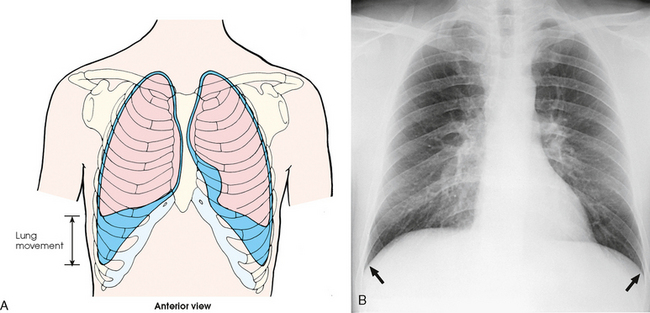
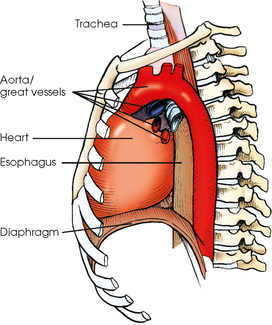
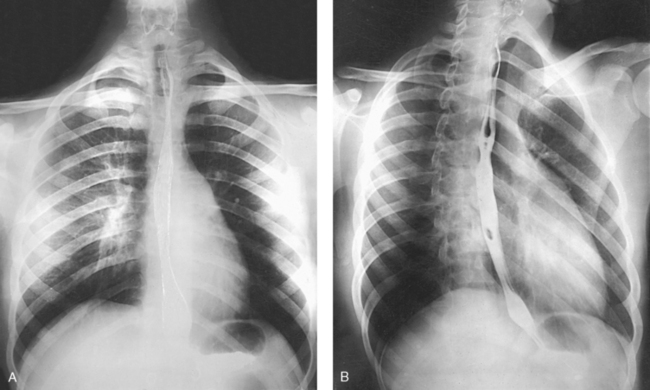
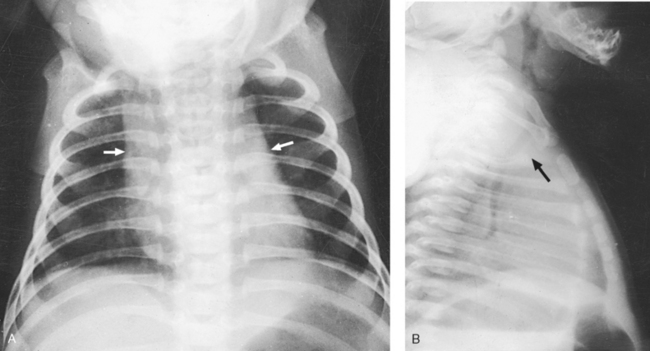
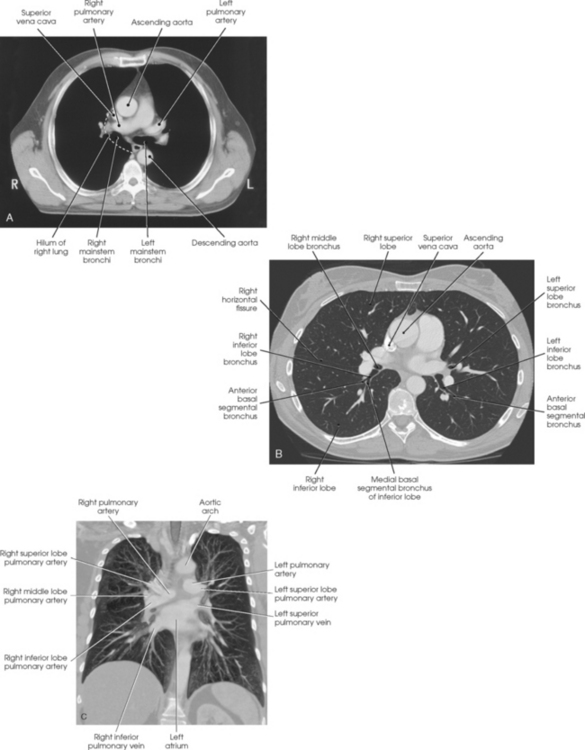
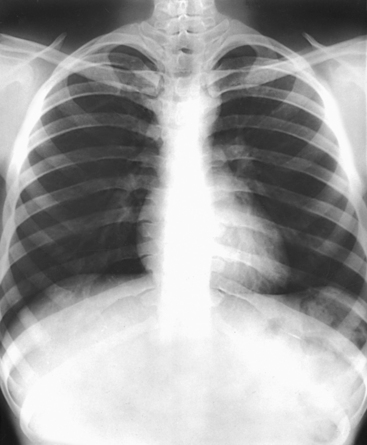
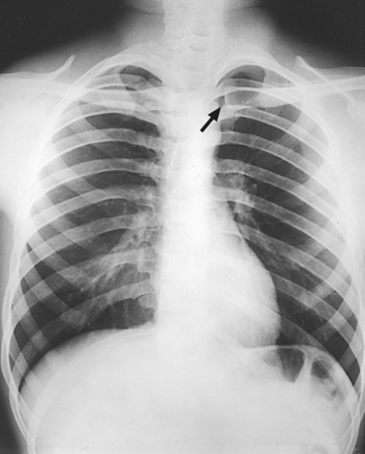
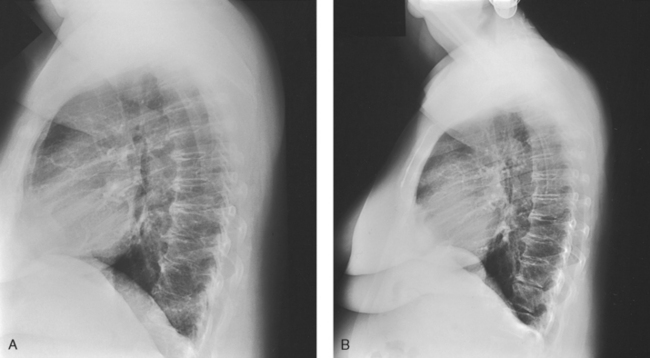
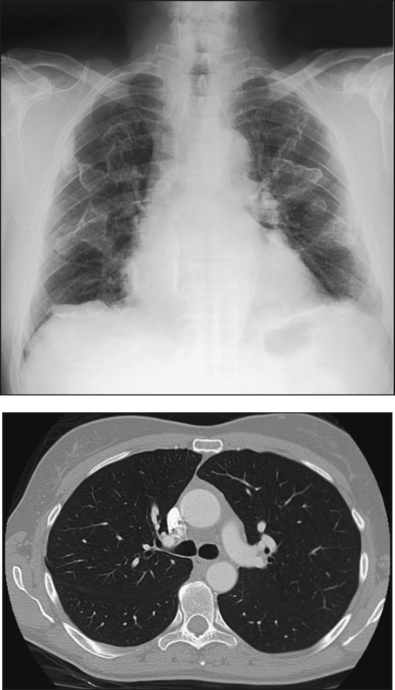
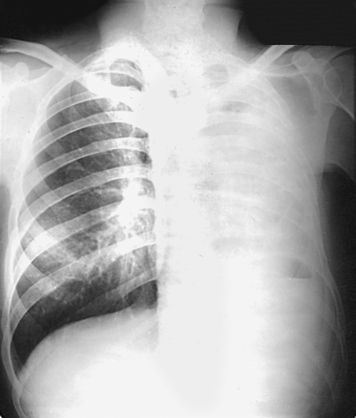
10 The general shape of the human body, or the body habitus, determines the size, shape, position, and movement of the internal organs. Fig. 10-1 outlines the general shape of the thorax in the four types of body habitus and how each appears on radiographs of the thoracic area. The thoracic cavity is bounded by the walls of the thorax and extends from the superior thoracic aperture, where structures enter the thorax, to the inferior thoracic aperture. The diaphragm separates the thoracic cavity from the abdominal cavity. The anatomic structures that pass from the thorax to the abdomen go through openings in the diaphragm (Fig. 10-2). The trachea is a fibrous, muscular tube with 16 to 20 C-shaped cartilaginous rings embedded in its walls for greater rigidity (Fig. 10-3, A). It measures approximately ½ inch (1.3 cm) in diameter and 4½ inches (11 cm) in length, and its posterior aspect is flat. The cartilaginous rings are incomplete posteriorly and extend around the anterior two thirds of the tube. The trachea lies in the midline of the body, anterior to the esophagus in the neck. In the thorax, the trachea is shifted slightly to the right of the midline as a result of the arching of the aorta. The trachea follows the curve of the vertebral column and extends from its junction with the larynx at the level of the sixth cervical vertebra inferiorly through the mediastinum to about the level of the space between the fourth and fifth thoracic vertebrae. The last tracheal cartilage is elongated and has a hooklike process, the carina, which extends posteriorly on its inferior surface. At the carina, the trachea divides, or bifurcates, into two lesser tubes—the primary bronchi. One of these bronchi enters the right lung, and the other enters the left lung. The primary bronchi slant obliquely inferiorly to their entrance into the lungs, where they branch out to form the right and left bronchial branches (Fig. 10-3, B). The right primary bronchus is shorter, wider, and more vertical than the left primary bronchus. Because of the more vertical position and greater diameter of the right main bronchus, foreign bodies entering the trachea are more likely to pass into the right bronchus than the left bronchus. After entering the lung, each primary bronchus divides, sending branches to each lobe of the lung: three to the right lung and two to the left lung. These secondary bronchi divide further and decrease in caliber. The bronchi continue dividing into tertiary bronchi, then to smaller bronchioles, and end in minute tubes called the terminal bronchioles (see Fig. 10-3). The extensive branching of the trachea is commonly referred to as the bronchial tree because it resembles a tree trunk (see box). The terminal bronchioles communicate with alveolar ducts. Each duct ends in several alveolar sacs. The walls of the alveolar sacs are lined with alveoli (see Fig. 10-3, A). Each lung contains millions of alveoli. Oxygen and carbon dioxide are exchanged by diffusion within the walls of the alveoli. The lungs are the organs of respiration (Fig. 10-4). They are the mechanism for introducing oxygen into the blood and removing carbon dioxide from the blood. The lungs are composed of a light, spongy, highly elastic substance, the parenchyma, and they are covered by a layer of serous membrane. Each lung presents a rounded apex that reaches above the level of the clavicles into the root of the neck and a broad base that, resting on the obliquely placed diaphragm, reaches lower in back and at the sides than in front. The right lung is about 1 inch (2.5 cm) shorter than the left lung because of the large space occupied by the liver, and it is broader than the left lung because of the position of the heart. The lateral surface of each lung conforms with the shape of the chest wall. The inferior surface of the lung is concave, fitting over the diaphragm, and the lateral margins are thin. During respiration, the lungs move inferiorly for inspiration and superiorly for expiration (Fig. 10-5). During inspiration, the lateral margins descend into the deep recesses of the parietal pleura. In radiology, this recess is called the costophrenic angle (see Fig. 10-5, B). The mediastinal surface is concave with a depression, called the hilum, that accommodates the bronchi, pulmonary blood vessels, lymph vessels, and nerves. The inferior mediastinal surface of the left lung contains a concavity called the cardiac notch. This notch conforms to the shape of the heart. Each lung is enclosed in a double-walled, serous membrane sac called the pleura (see Fig. 10-3, A). The inner layer of the pleural sac, called the visceral pleura, closely adheres to the surface of the lung, extends into the interlobar fissures, and is contiguous with the outer layer at the hilum. The outer layer, called the parietal pleura, lines the wall of the thoracic cavity occupied by the lung and closely adheres to the upper surface of the diaphragm. The two layers are moistened by serous fluid so that they move easily on each other. The serous fluid prevents friction between the lungs and chest walls during respiration. The space between the two pleural walls is called the pleural cavity. Although the space is termed a cavity, the layers are actually in close contact. Each lung is divided into lobes by deep fissures. The fissures lie in an oblique plane inferiorly and anteriorly from above, so that the lobes overlap each other in the AP direction. The oblique fissures divide the lungs into superior and inferior lobes. The superior lobes lie above and are anterior to the inferior lobes. The right superior lobe is divided further by a horizontal fissure, creating a right middle lobe (see Fig. 10-4). The left lung has no horizontal fissure and no middle lobe. The portion of the left lobe that corresponds in position to the right middle lobe is called the lingula. The lingula is a tongue-shaped process on the anteromedial border of the left lung. It fills the space between the chest wall and the heart. The mediastinum is the area of the thorax bounded by the sternum anteriorly, the spine posteriorly, and the lungs laterally (Fig. 10-6). The structures associated with the mediastinum are as follows: The esophagus lies just in front of the vertebral column, with its anterior surface in close relation to the trachea, aortic arch, and heart. This makes the esophagus valuable in certain heart examinations. When the esophagus is filled with barium sulfate, the posterior border of the heart and aorta are outlined well in lateral and oblique projections (Fig. 10-7). Frontal, oblique, and lateral images are often used in examinations of the esophagus. Radiography of the esophagus is discussed later in this chapter. The thymus gland is the primary control organ of the lymphatic system. It is responsible for producing the hormone thymosin, which plays a crucial role in the development and maturation of the immune system. The thymus consists of two pyramid-shaped lobes that lie in the lower neck and superior mediastinum, anterior to the trachea and great vessels of the heart and posterior to the manubrium. The thymus reaches its maximum size at puberty and then gradually undergoes atrophy until it almost disappears (Fig. 10-8). For radiography of the heart and lungs, the patient is placed in an upright position whenever possible to prevent engorgement of the pulmonary vessels and to allow gravity to depress the diaphragm. Of equal importance, the upright position shows air and fluid levels. In the recumbent position, gravitational force causes the abdominal viscera and diaphragm to move superiorly; it compresses the thoracic viscera, which prevents full expansion of the lungs. Although the difference in diaphragm movement is not great in hyposthenic individuals, it is marked in hypersthenic individuals. Figs. 10-10 and 10-11 illustrate the effect of body position in the same patient. The left lateral chest position (Fig. 10-12) is most commonly employed because it places the heart closer to the IR, resulting in a less magnified heart image. Left and right lateral chest images are compared in Figs. 10-12 and 10-13. For PA projections, procedures are as follows: • Instruct the patient to sit or stand upright. If the standing position is used, the weight of the body must be equally distributed on the feet. • Position the patient’s head upright, facing directly forward. • Have the patient depress the shoulders and hold them in contact with the grid device to carry the clavicles below the lung apices. Except in the presence of an upper thoracic scoliosis, a faulty body position can be detected by the asymmetric appearance of the sternoclavicular joints. Compare the clavicular margins in Figs. 10-14 and 10-15. For lateral projections, procedures are as follows: • Place the side of interest against the IR holder. • Have the patient stand so that the weight is equally distributed on the feet. The patient should not lean toward or away from the IR holder. • Raise the patient’s arms to prevent the soft tissue of the arms from superimposing the lung fields. • Instruct the patient to face straight ahead and raise the chin. • To determine rotation, examine the posterior aspects of the ribs. Radiographs without rotation show superimposed posterior ribs (see Figs. 10-12 and 10-13). When pneumothorax (gas or air in the pleural cavity) is suspected, one exposure is often made at the end of full inspiration and another at the end of full expiration to show small amounts of free air in the pleural cavity that might be obscured on the inspiration exposure (Figs. 10-16 and 10-17). Inspiration and expiration radiographs are also used to show the movement of the diaphragm, the occasional presence of a foreign body, and atelectasis (absence of air). If the selected kVp is too low, the radiographic contrast may be too high, resulting in few shades of gray. The lung fields may appear properly penetrated on such a radiograph, but the mediastinum appears underexposed. If the selected kVp is too high, the contrast may be too low, and the finer lung markings are not shown. Adequate kVp penetrates the mediastinum and shows a faint shadow of the spine. Whenever possible, a minimum source-to-IR distance (SID) of 72 inches (183 cm) should be used to minimize magnification of the heart and to obtain greater recorded detail of the delicate lung structures (Fig. 10-18). A 120-inch (305-cm) SID is commonly used in radiography of the chest. A grid technique is recommended for opaque areas within the lung fields and to show the lung structure through thickened pleural membranes (Figs. 10-19 and 10-20). This technique produces an image with higher contrast. Fig. 10-19 Nongrid radiograph showing fluid-type pathologic condition in same patient as in Fig. 10-20. Protection of the patient from unnecessary radiation is the professional responsibility of the radiographer (see Chapter 1 for specific guidelines). In this chapter, the Shield gonads statement indicates that the patient is to be protected from unnecessary radiation by restricting the radiation beam using proper collimation. In addition, the placement of lead shielding between the gonads and the radiation source is appropriate when the clinical objectives of the examination are not compromised. An example of a properly placed lead shield is shown in Fig. 10-25.
THORACIC VISCERA
Body Habitus
Thoracic Cavity
Respiratory System
TRACHEA
ALVEOLI
LUNGS
Mediastinum
SUMMARY OF PATHOLOGY
Condition
Definition
Aspiration/foreign body
Inspiration of a foreign material into the airway
Atelectasis
Collapse of all or part of the lung
Bronchiectasis
Chronic dilation of the bronchi and bronchioles associated with secondary infection
Bronchitis
Inflammation of the bronchi
Chronic obstructive pulmonary disease
Chronic condition of persistent obstruction of bronchial airflow
Cystic fibrosis
Disorder associated with widespread dysfunction of the exocrine glands, abnormal secretion of sweat and saliva, and accumulation of thick mucus in the lungs
Emphysema
Destructive and obstructive airway changes leading to an increased volume of air in the lungs
Epiglottitis
Inflammation of the epiglottis
Fungal disease
Inflammation of the lung caused by a fungal organism
Histoplasmosis
Infection caused by the yeastlike organism Histoplasma capsulatum
Granulomatous disease
Condition of the lung marked by formation of granulomas
Sarcoidosis
Condition of unknown origin often associated with pulmonary fibrosis
Tuberculosis
Chronic infection of the lung caused by the tubercle bacillus
Hyaline membrane disease or respiratory distress syndrome
Underaeration of the lungs caused by lack of surfactant
Metastases
Transfer of a cancerous lesion from one area to another
Pleural effusion
Collection of fluid in the pleural cavity
Pneumoconiosis
Lung diseases resulting from inhalation of industrial substances
Anthracosis or coal miner’s lung or black lung
Inflammation caused by inhalation of coal dust (anthracite)
Asbestosis
Inflammation caused by inhalation of asbestos
Silicosis
Inflammation caused by inhalation of silicon dioxide
Pneumonia
Acute infection in the lung parenchyma
Aspiration
Pneumonia caused by aspiration of foreign particles
Interstitial or viral or pneumonitis
Pneumonia caused by a virus and involving the alveolar walls and interstitial structures
Lobar or bacterial
Pneumonia involving the alveoli of an entire lobe without involving the bronchi
Lobular or bronchopneumonia
Pneumonia involving the bronchi and scattered throughout the lung
Pneumothorax
Accumulation of air in the pleural cavity resulting in collapse of the lung
Pulmonary edema
Replacement of air with fluid in the lung interstitium and alveoli
Tumor
New tissue growth where cell proliferation is uncontrolled
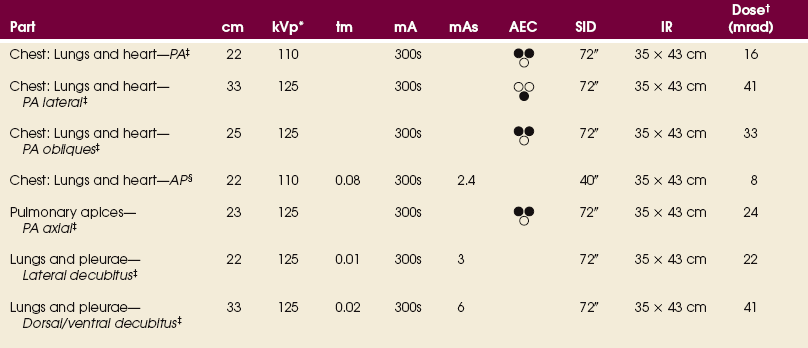
EXPOSURE TECHNIQUE CHART ESSENTIAL PROJECTIONS
General Positioning Considerations
PA CRITERIA
LATERAL CRITERIA
Breathing Instructions
Technical Procedure
Radiation Protection
THORACIC VISCERA