Fig. 1.1
A historical image circa 1967 of the beginning of thyroid ultrasound . Fujimoto Y, Oka A, Omoto R, Hirose M. Ultrasound scanning of the thyroid gland as a new diagnostic approach. Ultrasonics. 1967;5(3):177–80. With permission
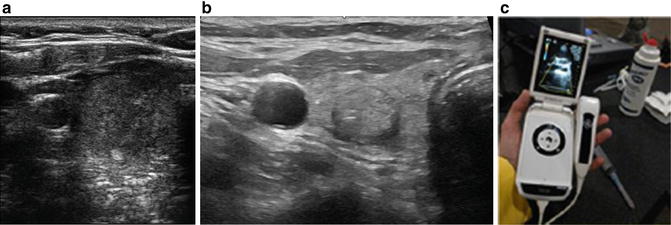
Fig. 1.2
Improvements in ultrasound image quality are evident when comparing a right thyroid nodule image from 2005 (a) to one obtained in 2015 (b). A handheld ultrasound is capable of detecting major thyroid abnormalities though models currently available still await high-frequency transducers to provide fine imaging details (c). Author’s image
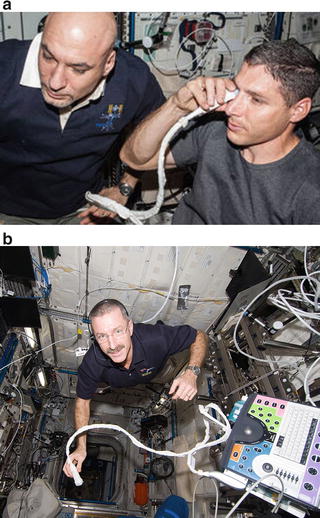
Today, ultrasound machines are found in almost every emergency room and are used for the rapid assessment of trauma patients and the bedside evaluation of a plethora of medical conditions. Ultrasonography has also been incorporated into medical care facilities at a distance from tertiary referral centers. Ultrasound probes remotely operated by technicians via robotics can be used to obtain diagnostic images in rural medical clinics or remote locations, such as the South Pole [5]. Even the International Space Station has an ultrasound machine in its Human Research Facility, the Advanced Diagnostic Ultrasound in Microgravity (ADUM) . The ADUM ultrasound is a commercial ultrasound that has been modified to allow astronaut crew members to perform their own ultrasound exams, guided by ground medical personnel [6, 7] (Fig. 1.3). The utility and scope of ultrasound are expanding, and providers in all fields of medicine , working in a variety of settings, are incorporating its use into their practice.
1.1.2 What Is Point-of-Care Ultrasound ?
Point-of-care ultrasound, also called bedside, provider-performed, or focused ultrasound, can be defined as the utilization of sonography to answer a specific clinical question at the time of patient presentation and examination [8]. In a 2011 New England Journal of Medicine review article, Moore defined point-of-care ultrasonography as the use of “real-time dynamic images (rather than images recorded by a sonographer and interpreted later), which allow findings to be directly correlated with the patient’s presenting signs and symptoms” [9]. The paradigm shift created by point-of-care ultrasound is that the clinician develops a clinical question and then performs and interprets the imaging test in real time, as opposed to the traditional practice of sending the patient for a sonogram and waiting for the results.
Point-of-care ultrasound was first utilized for trauma evaluation in Europe in the 1970s and became common in US trauma care by the mid-1980s. The first standardized point-of-care use of ultrasound was the Focused Assessment with Sonography for Trauma (FAST) exam . The FAST exam, adopted in the 1990s, includes a basic series of four views for the evaluation of free abdominal fluid and has replaced diagnostic peritoneal lavage for the evaluation of blunt abdominal trauma. FAST has now been expanded to include the evaluation for pneumothorax and fluid or blood in the thorax post trauma [10].
Today, point-of-care clinician-performed ultrasound is the standard of care in surgery, obstetrics and gynecology, emergency medicine, ophthalmology, as well as internal medicine and most of its subspecialties (cardiology, gastroenterology, endocrinology, and intensive care). The term comprehensive ultrasound, in a very traditional sense, refers to an ultrasound that is conducted in a radiology department, where the main goal is to communicate information to clinicians who themselves may not view or interpret the images and require a thorough description in order to make clinical decisions. Comprehensive ultrasound may also refer to the provision of diagnostic, interventional, and therapeutic ultrasonography for patient care, whether this occurs in a radiology department or a clinical office setting. Descriptions of point-of-care and comprehensive ultrasound contain complementary and overlapping concepts.
1.2 Point-of-Care Ultrasound of the Thyroid and Parathyroid Glands
In the late 1960s, researchers began experimenting with sonography to estimate the weight of the thyroid gland and to identify solid and cystic lesions. In 1970, the Journal of Clinical Endocrinology and Metabolism published its first paper describing thyroid ultrasound . Patients were scanned using two-dimensional B-mode and, if a lesion was detected, one-dimensional A-mode, to differentiate cystic from solid lesions. The images, which were transferred to film, were basic and of poor quality when compared to today’s standards (Fig. 1.4) [11]. Despite these shortcomings, early thyroid ultrasonography was recognized for its utility to detect and measure lesions as well as to distinguish between solid and cystic thyroid lesions. Furthermore, even in those early days of thyroid ultrasonography, investigators hypothesized that ultrasound may have the potential to distinguish between benign and malignant thyroid lesions [11].
Fig. 1.4
Early ultrasound image of normal thyroid. (a) Ultrasonic tomogram (B-scan) at low sensitivity. (b) Schematic representation: RL, right thyroid lobe; LL, left thyroid lobe; T, anterior wall of the trachea; VB, vertebral body; V, vascular sheath; S, skin and transducer artifact; and M, sternomastoid muscle. From J Clin Endocrinol Metab. 1971; (32): 709. With permission
1.3 Why Perform Point-of-Care Neck Ultrasound
The point-of-care neck ultrasound can be used to evaluate suspected anatomical or functional thyroid and parathyroid disease (Table 1.1). Along with a history and physical exam, the point-of-care neck ultrasound can be used by the provider to assess the thyroid and generate a differential diagnosis and plan of care. Whether a patient presents complaining of a neck mass or the provider palpates a lesion on neck exam, the bedside ultrasound can be utilized to identify the presence of intrathyroidal lesions, extrathyroidal lesions, or diffuse enlargement of the thyroid. In cases in which the patient presents with signs or symptoms of hyperthyroidism, a bedside ultrasound can discover a solitary nodule, leading to suspicion for a hyperfunctioning “hot” nodule, or recognize a diffusely enlarged and vascular gland, characteristic of Graves’ disease.
Table 1.1
Indications and information from point-of-care ultrasound
• Clarification of clinical exam findings |
• Accurate diagnosis of thyroid and parathyroid disease |
• Differentiation of cystic vs. solid masses |
• Measurement of lesions |
• Thyroid nodule ultrasonographic feature characterization and pattern recognition |
• Malignancy risk assessment of thyroid nodules |
• Lymph node screening with initial thyroid nodule detection |
• Lymph node mapping with thyroid cancer |
• Localization of abnormal parathyroid glands |
• Visual guidance for interventions (biopsy, cyst drainage, alcohol ablation) |
• Improvement of biopsy accuracy |
• Monitoring of response to therapy |
• Identification of recurrent/persistent cancer |
• Evaluation of cervical lymphadenopathy or metastases |
• Optimization of surgical incision placement |
• Optimization of surgical planning based on details of findings (signs of local invasion, substernal goiter extension, tracheal deviation) |
• Laryngeal ultrasound for vocal cord mobility |
• Identification of coexisting pathology |
• Intraoperative evaluation |
• Education |
• Communication of findings to multidisciplinary providers |
1.3.1 Nodules
Thyroid nodules are highly prevalent in the general population, and their incidence increases with age [12]. The superficial location of the thyroid gland permits the palpation and recognition of larger lesions, and the frequent use of imaging in medicine leads to the discovery of incidental small lesions. No matter the method of discovery of a thyroid nodule, bedside ultrasound can be used to evaluate and characterize the lesion. Ultrasound is used to assess a nodule’s risk of malignancy based on US characteristics, and to guide further decision-making and management by facilitating and guiding fine-needle aspiration (FNA) [13]. Ultrasound also facilitates the evaluation of cervical lymph nodes in the context of thyroid or other neck masses and guides the need for FNA.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree