, Valery Kornienko2 and Igor Pronin2
(1)
N.N. Blockhin Russian Cancer Research Center, Moscow, Russia
(2)
N.N. Burdenko National Scientific and Practical Center for Neurosurgery, Moscow, Russia
Thyroid cancer (TC) is the most common tumor of the endocrine system and amounts to 1–3% in the overall structure of cancers. The incidence of thyroid cancer has been steadily increasing within the past two decades, especially in industrialized countries. In Europe, the average rates are 1.2–3 per 100000 population. In Russia, more than 10000 patients are diagnosed with thyroid cancer every year. According to Davydov and Axel (2012), an increase in the incidence of thyroid cancer amounted to 6.2% in 2007–2012. The increased incidence of thyroid cancer is prevalent in the female population. Women make up 86% of all thyroid malignancies identified (Paches 2000a, b).
Factors contributing to the development of thyroid cancer include hyperplastic processes and disorders of endocrine regulation, radiation exposure and occupational hazards, stay in the areas of radiation accidents, and thyroid injuries.
Papillary carcinoma is a common tumor of the thyroid gland. It accounts for about 70% of all malignant tumors of the thyroid gland and usually develops in the third and fourth decade of life. Papillary carcinoma is characterized by lymphogenous metastasizing, while hematogenous metastasizing occurs relatively infrequently, with the typical location of metastases being lungs. Follicular thyroid cancer amounts to 15–20% and occurs in older age. The incidence of lymphogenous metastasizing of follicular carcinoma is 2–10%; hematogenous metastases occur in 20% of cases, typically in bones. Both forms of cancer are characterized by rather slow growth and a favorable prognosis. The 5- and 10-year survival rate in papillary and follicular thyroid carcinomas is 95.3% and 94.2% and 90.1% and 85.7%, respectively. According to Pacini et al. (2008), despite the increase in its incidence, mortality from thyroid cancer, in general, and from papillary thyroid carcinoma, in particular, remained stable both in 1973 and 2002 and amounted to 0.5 deaths per 100000 patients.
The proportion of other malignant thyroid tumors (medullary carcinoma, undifferentiated/anaplastic cancer) does not exceed 8–15%, while that of squamous cell carcinoma is 3.1%. Squamous thyroid cancer is characterized by early and extensive metastasizing, a severe clinical course and a poor prognosis. Non-differentiated thyroid cancer is also characterized by a severe clinical course with a median survival of 5–6 months (Paches and Propp 1995; Valdina 2006).
The incidence of metastatic brain lesions with thyroid cancer, according to different authors, is 0.1–5% (Parker et al. 1986; Jyothirmayi et al. 1995; Altimari-Romero et al. 1997; Salvati et al. 2001; Mazzaferri et al. 2006; Al-Dhahri et al. 2009). On the other hand, Pemberton (1939) found metastases in 4–9% in the analysis of a series of 774 patients with thyroid cancer. In a retrospective database study for the period from 1976 to 2011, Tsuda et al. (2013) found metastases of papillary carcinoma in the brain only in five cases. The time from the detection of the primary tumor to the detection of metastases of thyroid cancer in the brain is 2.8 years for papillary cancer and 1.2 years for anaplastic cancer (Salvati et al. 1995).
In our sample, metastases of thyroid cancer were identified in 0.8% of cases.
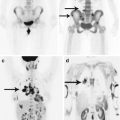
Thyroid cancer metastases in the brain are presented as a supra- and subtentorial lesions. In our cases, we also noted metastatic involvement of the skull with intracranial spread. No significant invasion of adjacent meninges was noted, while the destruction of bone structures infiltrated by the tumor was total. The contrast agent accumulation in the TC metastasis stroma in the brain is homogeneous, in several cases microhemorrhagic inclusions were observed in the form of increased signal portions on T1-weighted MRI.
MRI provides for a study according to the standard protocols—T2-weighted, T1-weighted, T2-FLAIR, and T1-weighted + Gd MRI. Additional methods—3D SPGR, SWI (SWAN), spectroscopy, and ASL—did not show any significant differential diagnostic signs.
24.1 Clinical Cases