Tracheobronchial Papillomatosis
Helen T. Winer-Muram, MD
Key Facts
Terminology
Laryngeal nodules due to human papilloma virus, usually self-limited infection
< 1% seed the lung, known as invasive papillomatosis
At risk to develop squamous cell carcinoma (2%)
Imaging Findings
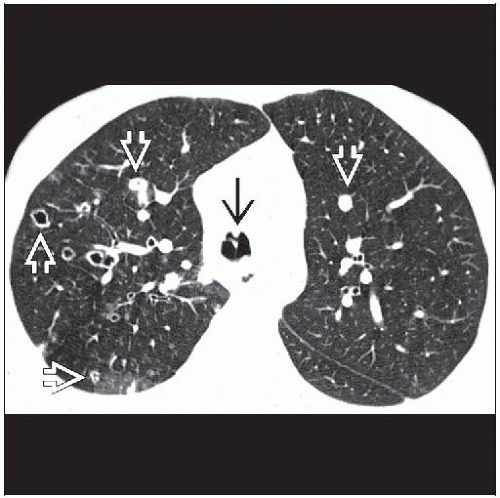
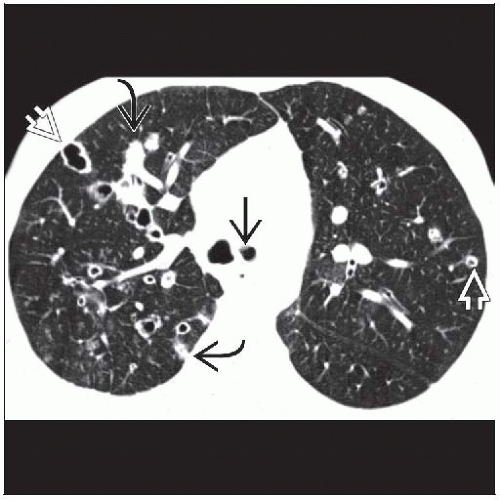
Best diagnostic clue: Multiple solid and cystic nodules
Dorsal distribution in axial plane (gravity seeding)
Top Differential Diagnoses
Metastases
Wegener Granulomatosis
Pneumatoceles
Lymphangioleiomyomatosis
Lymphocytic Interstitial Pneumonia
Pneumatoceles
Pathology
Virus also responsible for cutaneous warts, genital warts, and cervical cancer
Clinical Issues
Hoarseness most common due to laryngeal involvement
Lung nodules grow very slowly; usually measured in decades
Diagnostic Checklist
Nodules grow slowly, and sudden growth or change in nodule appearance must be investigated for transformation to squamous cell carcinoma
Always evaluate trachea for nodules in young patient with multiple cavities
TERMINOLOGY
Abbreviations and Synonyms
Juvenile-onset recurrent respiratory papillomatosis, adult-onset recurrent respiratory papillomatosis, human papilloma virus, invasive papillomatosis
Definitions
Laryngeal nodules due to human papilloma virus, usually self-limited infection
< 1% seed the lung, known as invasive papillomatosis
At risk to develop squamous cell carcinoma (2%)
IMAGING FINDINGS
General Features
Best diagnostic clue
Laryngotracheal and bronchial nodules
Multiple solid and cystic pulmonary nodules
Patient position/location
Perihilar and central location in coronal plane
Dorsal distribution in axial plane (gravity seeding)
Size: Typically 1-3 cm in diameter
Morphology: Smaller nodules are solid, more likely to cavitate when larger
CT Findings
Morphology
Airway nodules
Smooth, solid, larger nodules may have cauliflower shape
Vary in size, may occlude airway
Airway wall usually not thickened, no extrathoracic component
Airway nodules do not cavitate
Pulmonary nodules
Solid, cavitary, or cystic
Typically lung nodules spectrum of solid and cavitary
Larger nodules more likely to be cavitary
Multiple and bilateral; may be a few to hundreds of nodules
Nearly always associated with airway nodules
Papillomas may exhibit lipidic growth and result in ground-glass opacities to frank consolidation
Nodules may exhibit halo sign
Solitary papillomas less common than multiple
Most commonly located in lobar or segmental bronchi where they result in hyperinflation (ball-valve mechanism) or atelectasis and obstructive pneumonia of distal lung
Cavitary wall
Thick or thin wall, typically 2-3 mm in thickness
Air-fluid level infrequent; when present, suggests superinfection
Nodules may communicate with adjacent airways
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree