CHAPTER 5 Radiology of trauma to the skeletal system is such a large topic that entire volumes have been devoted to it. Lee Rogers has written the definitive work in his excellent book titled Radiology of Skeletal Trauma,1 and Jack and William Harris’s outstanding book on The Radiology of Emergency Medicine2 is a must-read for anyone dealing with a large emergency department population. The leading orthopedic treatise on fractures is Rockwood and Green’s multivolume text.3 The following is merely an overview of selected cases that residents and medical students should be exposed to and that can be studied in greater detail by referring to the texts just mentioned. What do you look for on the lateral C-spine? First, make certain that all seven cervical vertebral bodies can be visualized. A number of fractures are missed because the shoulders obscure the lower C-spine levels (Figure 5-1). If the entire cervical spine is not visualized, repeat the film with the shoulders lowered. FIGURE 5-1 Next, evaluate five (more or less) parallel lines for step-offs or discontinuity as follows (Figure 5-2): FIGURE 5-2 Line 1 is in the prevertebral soft tissue. It extends down the posterior aspect of the airway; it should be several millimeters from the first three or four vertebral bodies and then move further away at the laryngeal cartilage; it should be less than one vertebral body width from the anterior vertebral bodies from C3 or C4 to C7. It should also be smooth in its contour. Line 2 follows the anterior vertebral bodies and should be smooth and uninterrupted. Anterior osteophytes can encroach on this line and extend beyond it and should therefore be ignored in drawing this line. Interruption of the anterior vertebral body line is a sign of a serious injury (see Figure 5-1, B). Line 3 is similar to the anterior vertebral body line (line 2) except that it connects the posterior vertebral bodies. Like line 2, it should be smooth and uninterrupted; any disruption signifies a serious injury. Line 4, called the spinolaminal line, connects the posterior junction of the lamina with the spinous processes. The spinal cord lies between lines 3 and 4; therefore any offset of either of these lines could mean that a bony structure is impinging on the cord. Severe neurologic deficits can result from very little force against the cord, and any bony structure lying on the cord must be recognized as soon as possible. Line 5 is not really a line so much as a collection of points—the tips of the spinous processes. The spinous processes are quite variable in size and appearance, although C7 usually has the largest. A fracture of one of the spinous processes by itself is not a serious injury, but it occasionally heralds other, more serious injuries. Also, who wants to miss a fractured spinous process, however innocuous, and then have the patient (after visiting another doctor) proclaim that you didn’t see her “broken neck” on the radiograph? After visually inspecting these five lines on the lateral C-spine, inspect the C1–2 area a little more closely. Make certain that the anterior arch of C1 is no greater than 2.5 mm from the dens (Figure 5-3). Any greater separation than this (except in children, in whom up to 5.0 mm is normal) is suspicious for disruption of the transverse ligament between C1 and C2 (Figure 5-4). FIGURE 5-3 FIGURE 5-4 Learning to look at lateral spine films with anterior facing either right or left is very important. Many radiologists can interpret images only facing one way and become almost unable to function if the films are not placed on the viewbox in their preferred orientation. This is fine if they can control the film; however, in meetings where slides are shown, in books and journals, and on oral board examinations, radiologists cannot turn the film to their liking. Get used to viewing lateral spine films (lateral chest films, too) in either anterior left or right orientation; otherwise, you will find yourself disadvantaged in many situations. A blow to the top of the head, such as when an object falls directly on the apex of the skull, can cause the lateral masses of C1 to slide apart, splitting the bony ring of C1. This is called a Jefferson’s fracture (Figure 5-5). It nicely illustrates how a bony ring will not break in just one place but must break in several places. This rule is seldom violated. All the vertebral rings, when fractured, must fracture in two or more places. The bony rings of the pelvis behave the same way. If you see only one fracture on the radiograph, you can be certain you are missing at least one more. A CT scan is excellent at demonstrating the complete bony ring of C1 and shows the fractures, as well as any associated soft tissue mass, much better than plain films. In diagnosing a Jefferson’s fracture on plain film the lateral masses of C1 must extend beyond the margins of the C2 body (see Figure 5-5, A). Just seeing asymmetry of the spaces on either side of the dens is not enough to make the diagnosis, because these spaces can be normally asymmetric with rotation or with rotatory fixation of the atlantoaxial joint. FIGURE 5-5 What is rotatory fixation of the atlantoaxial joint? This is a somewhat controversial, little understood process in which the atlantoaxial joint becomes fixed and the C1 and C2 bodies move en masse instead of rotating on each other. This condition is easily diagnosed with open-mouth odontoid views. In the normal odontoid view the spaces lateral to the dens (odontoid) are equal. With rotation of the head to the left, the space on the left widens; and with rotation to the right, the space on the right widens. With rotatory fixation, one of the spaces is wider than the other and stays wider even with rotation of the head to the opposite side (Figure 5-6). By itself, this is a relatively innocuous malady usually treated with a soft cervical collar and/or gentle traction. It is, however, occasionally associated with disruption of the transverse ligaments at C1–2, and is then a serious problem. Rotatory fixation usually presents spontaneously or after very mild trauma, such as that caused by sleeping in an unusual position. FIGURE 5-6 Another relatively innocuous injury is a fracture of the C6 or C7 spinous process, called a clay-shoveler’s fracture. Supposedly workers shoveling sticky clay in Australia (I’ve also read England and North Carolina—this is a vital distinction, and some future researcher can perhaps straighten out this confusion) would toss the shovelfuls of clay over their shoulders; once in a while the clay would stick to the shovel, causing the ligaments attached to the spinous processes (supraspinous ligaments) to undergo a tremendous force, pulling on the spinous process and avulsing it. This fracture can occur at any of the lower cervical spinous processes (Figure 5-7). FIGURE 5-7 A hangman’s fracture is an unstable, serious fracture of the upper cervical spine that is caused by hyperextension and distraction (e.g., hitting one’s head on a dashboard). This is a fracture of the posterior elements of C2 and, usually, displacement of the C2 body anterior to C3 (Figure 5-8). Patients with this type of fracture actually do better than one might think. They often escape neurologic impairment because of the fractured posterior elements of C2, which, in effect, cause decompression and take pressure off the injured area. This is a simplistic explanation for a complex entity, but it seems to be a reasonable answer to why these patients often fare well. FIGURE 5-8 Severe flexion of the cervical spine can cause a disruption of the posterior ligaments and anterior compression of a vertebral body. This is called a flexion “teardrop” fracture (Figure 5-9). A teardrop fracture is usually associated with spinal cord injury, often from the posterior portion of the vertebral body being displaced into the central canal. FIGURE 5-9 If severe enough, and if associated with some rotation, the apophyseal joint ligaments will rupture and the facet joints dislocate and then override. This can result in locking of the facets in an overriding position, which in effect causes some stabilization to protect against further injury. This condition is called unilateral locked facets (Figures 5-10 and 5-11), but occasionally it occurs bilaterally. When unilateral, the more inferior vertebral body is usually rotated, giving it a shorter AP length on a lateral film, which is a clue to the diagnosis (see Figure 5-11). FIGURE 5-10 FIGURE 5-11 A seat belt injury is seen secondary to hyperflexion at the waist (as occurs in a car accident while the person is restrained by a lap belt). This causes distraction of the posterior elements and ligaments and anterior compression of the vertebral body. It usually involves the L1 or L2 vertebra. Several variations of this injury can occur: a fracture of the posterior body is called a Smith’s fracture, and a fracture through the spinous process is called a Chance fracture. Horizontal fractures of the pedicles, laminae, and transverse processes can also occur (Figure 5-12). FIGURE 5-12 A spinal abnormality that may or may not be caused by trauma is spondylolysis. Spondylolysis is a break or defect in the pars interarticularis portion of the lamina (Figure 5-13). It can be seen in about 5% to 10% of asymptomatic individuals. On oblique views the posterior elements form the figure of a Scottie dog, with the transverse process being the nose, the pedicle forming the eye, the inferior articular facet being the front leg, the superior articular facet representing the ear, and the pars interarticularis (which means the portion of the lamina that lies between the facets) equaling the dog’s neck. If a spondylolysis is present, the pars interarticularis, or the neck of the dog, will have a defect or break. It often looks as if the Scottie dog has a collar around its neck. Although often difficult to visualize with magnetic resonance imaging (MRI), spondylolysis should be easily seen on CT scans (see Chapter 11). The cause of a spondylolysis is said by some investigators to be congenital and by others to be posttraumatic. Many believe that this is a stress-related injury from infancy that develops when toddlers try to walk and repeatedly fall on their buttocks, sending stress to their lower lumbar spine. The significance of spondylolysis is just as controversial as its cause. More and more clinicians are coming to the viewpoint that a spondylolysis is an incidental finding with no clinical significance in most cases. Certainly some patients have pain related to a spondylolysis and get relief after surgical stabilization, but such cases are less common. FIGURE 5-13 If a spondylolysis is bilateral and the vertebral body in the more cephalad position slips forward on the more caudal body, spondylolisthesis is said to be present (Figure 5-14). Spondylolisthesis may or may not be symptomatic and by itself has no clinical significance. If severe, it can cause neuroforaminal stenosis and can impinge on the nerve roots in the central spinal canal. If it is symptomatic, it can be surgically stabilized. FIGURE 5-14 Anterior wedge compression fractures of the spine are commonly seen (Figure 5-15), especially at the thoracolumbar junction, as a result of an old injury; they are often passed off by the radiologist, if they are mentioned at all, as incidental findings. The problem with this is it’s impossible to tell from a plain film if the fracture is old or new, even if degenerative changes are present (which are often not related to the fracture). If acute and left unprotected, a wedge compression fracture can proceed to delayed further collapse with resulting severe neurologic deficits (Figure 5-16). This is called Kummell’s disease and typically occurs 1 to 2 weeks after the initial trauma. I have seen more than a dozen lawsuits against radiologists who failed to mention minor anterior wedging of a vertebral body that went on to further collapse with associated paraplegia. All that needs to be mentioned is that a fracture of indeterminate age is present and requires clinical correlation. If the patient has pain in that location, the patient needs to wear a back brace until pain free. Old films can help determine whether it is an old fracture. If no pain is present on physical examination, it can be safely assumed to be an old fracture. It is not necessary to obtain a CT or MRI scan even if pain is present, because the treatment will be the same regardless of what the CT or MRI scans reveal. No spine surgeon will operate on a stable spine fracture without kyphosis or neurologic deficits, so the CT or MRI examination add nothing but time and expense. FIGURE 5-15 FIGURE 5-16 Patients who have fusion of their spine from ankylosing spondylitis and, to a lesser extent, from diffuse idiopathic skeletal hyperostosis (DISH; see Chapter 6) are at a very high risk of spinal fractures from even relatively minor trauma. Patients with ankylosing spondylitis typically have marked osteoporosis, which further magnifies their risk of sustaining a fracture. A fused spine is more likely to fracture than a normal spine, much in the same way that a long glass pipette breaks more easily than a short one because it has a long lever arm. A small force at one end is greatly magnified further down the lever arm. For that reason, a patient with ankylosing spondylitis should be treated as though a spinal fracture is present if he or she has back pain after the trauma. CT and/or MRI scans are mandatory if plain films are negative (Figure 5-17). FIGURE 5-17 Several seemingly innocuous fractures in the hand require surgical fixation rather than just casting and therefore should be recognized by the radiologist as serious injuries. One such fracture is a fracture at the base of the thumb into the carpometacarpal joint, or a Bennett’s fracture (Figure 5-18). Because of the insertion of the strong thumb adductors at the base of the thumb, it is almost impossible to keep the metacarpal from sliding off its proper alignment. It almost always requires internal fixation. The radiologist occasionally has to remind a nonorthopedic practitioner of this, as well as closely examine the alignment of a Bennett’s fracture in plaster that has not been internally fixed with pins.
Trauma
Spine
Examination of the cervical spine


 Shoulders obscuring C7. This patient came to the emergency department after being injured as a result of diving into a shallow swimming pool. He had neck pain but no neurologic deficits. The initial radiograph obtained of the C-spine (A) was interpreted as being within normal limits. However, because of high-riding shoulders only five cervical vertebrae are visible. A repeat examination (B) with the shoulders lowered reveals a dislocation of C5 on C6. To visualize C7 the shoulders were lowered even further. The C7 vertebral body must be visualized on every lateral C-spine examination in a trauma setting.
Shoulders obscuring C7. This patient came to the emergency department after being injured as a result of diving into a shallow swimming pool. He had neck pain but no neurologic deficits. The initial radiograph obtained of the C-spine (A) was interpreted as being within normal limits. However, because of high-riding shoulders only five cervical vertebrae are visible. A repeat examination (B) with the shoulders lowered reveals a dislocation of C5 on C6. To visualize C7 the shoulders were lowered even further. The C7 vertebral body must be visualized on every lateral C-spine examination in a trauma setting.

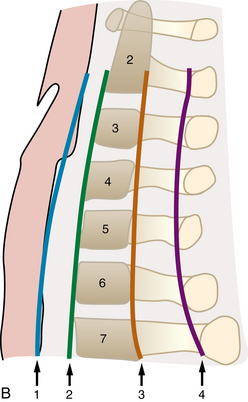
 Normal lateral cervical spine. A, Lateral radiograph of a normal cervical spine. B, Diagrammatic representation of a lateral C-spine showing four parallel lines that should be observed in every lateral C-spine examination. Line 1 is the soft tissue line that is closely applied to the posterior border of the airway through the first four or five vertebral body segments and then widens around the laryngeal cartilage and runs parallel to the remainder of the cervical vertebrae. Line 2 demarcates the anterior border of the cervical vertebral bodies. Line 3 is the posterior border of the cervical vertebral bodies. Line 4, called the spinolaminal line, is drawn by connecting the junction of the lamina at the spinous process. It represents the posterior extent of the central canal, which contains the spinal cord itself. These lines should generally be smooth and parallel, with no abrupt step-offs.
Normal lateral cervical spine. A, Lateral radiograph of a normal cervical spine. B, Diagrammatic representation of a lateral C-spine showing four parallel lines that should be observed in every lateral C-spine examination. Line 1 is the soft tissue line that is closely applied to the posterior border of the airway through the first four or five vertebral body segments and then widens around the laryngeal cartilage and runs parallel to the remainder of the cervical vertebrae. Line 2 demarcates the anterior border of the cervical vertebral bodies. Line 3 is the posterior border of the cervical vertebral bodies. Line 4, called the spinolaminal line, is drawn by connecting the junction of the lamina at the spinous process. It represents the posterior extent of the central canal, which contains the spinal cord itself. These lines should generally be smooth and parallel, with no abrupt step-offs.
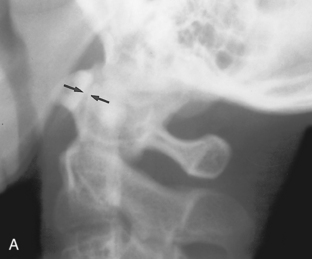
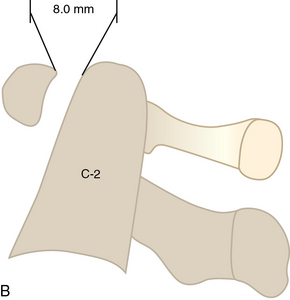
 Normal C1–2. A lateral radiograph (A) and drawing (B) of the upper cervical spine, showing the normal distance of the anterior arch of C1 to be less than 2.5 mm from the odontoid process of C2 (arrows).
Normal C1–2. A lateral radiograph (A) and drawing (B) of the upper cervical spine, showing the normal distance of the anterior arch of C1 to be less than 2.5 mm from the odontoid process of C2 (arrows).
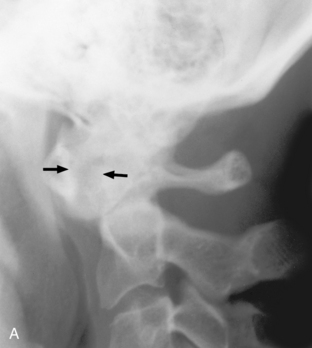
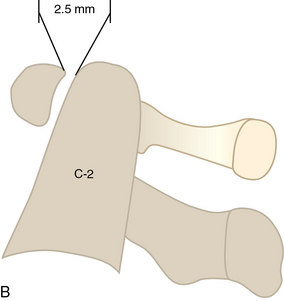
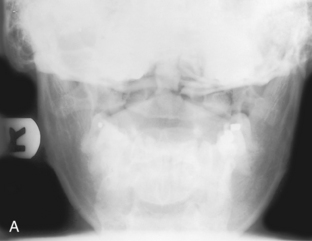
 C1–2 dislocation. A lateral radiograph (A) and drawing (B) of the upper cervical spine in a patient with trauma to the neck, which shows that the anterior arch of C1 is 8 mm anterior to the odontoid process of C2 (arrows). This is diagnostic of a dislocation of C1 on C2, and indicates rupture of the transverse ligaments, which normally hold these vertebral segments together.
C1–2 dislocation. A lateral radiograph (A) and drawing (B) of the upper cervical spine in a patient with trauma to the neck, which shows that the anterior arch of C1 is 8 mm anterior to the odontoid process of C2 (arrows). This is diagnostic of a dislocation of C1 on C2, and indicates rupture of the transverse ligaments, which normally hold these vertebral segments together.
Examples of fractures, dislocations, and other abnormalities

 Jefferson’s fracture. A, An AP open-mouth odontoid view is suspicious for the lateral masses of C1 being laterally displaced. However, because of overlying structures, this displacement is difficult to appreciate. B, Therefore, a CT scan was obtained, which shows multiple fracture sites in the C1 ring (arrows). This is called a Jefferson’s fracture. CT is routinely used in spinal trauma because of the obvious shortcomings of plain films.
Jefferson’s fracture. A, An AP open-mouth odontoid view is suspicious for the lateral masses of C1 being laterally displaced. However, because of overlying structures, this displacement is difficult to appreciate. B, Therefore, a CT scan was obtained, which shows multiple fracture sites in the C1 ring (arrows). This is called a Jefferson’s fracture. CT is routinely used in spinal trauma because of the obvious shortcomings of plain films.
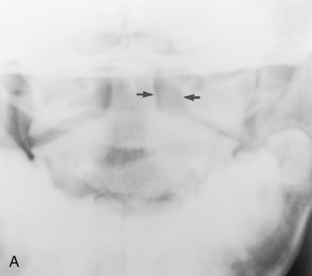
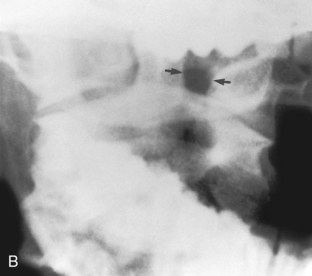

 Rotatory fixation of the atlantoaxial joint. This patient came to the emergency department with pain and decreased motion in the cervical spine. An AP open-mouth odontoid view (A) shows that the space on the left side of the odontoid between the odontoid and the lateral mass of C1 (arrows) is wider than the corresponding space on the right side. This is often caused by rotation. Therefore open-mouth odontoid views with right and left obliquities were obtained. Rotation of the patient’s head to the left (B) causes the space on the left side of the odontoid process (arrows) to be wider than that on the right, which is appropriate. However, when the patient turns to the right (C) the space on the right (arrows) does not get wider than the space on the left. This is diagnostic of rotatory fixation of the atlantoaxial joint.
Rotatory fixation of the atlantoaxial joint. This patient came to the emergency department with pain and decreased motion in the cervical spine. An AP open-mouth odontoid view (A) shows that the space on the left side of the odontoid between the odontoid and the lateral mass of C1 (arrows) is wider than the corresponding space on the right side. This is often caused by rotation. Therefore open-mouth odontoid views with right and left obliquities were obtained. Rotation of the patient’s head to the left (B) causes the space on the left side of the odontoid process (arrows) to be wider than that on the right, which is appropriate. However, when the patient turns to the right (C) the space on the right (arrows) does not get wider than the space on the left. This is diagnostic of rotatory fixation of the atlantoaxial joint.

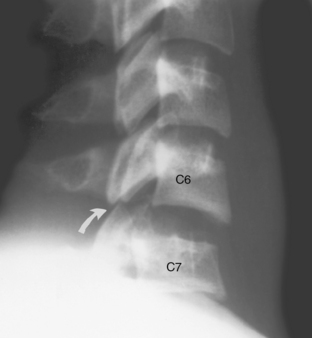
 Clay-shoveler’s fracture. A nondisplaced fracture of the C7 spinous process (arrow) is noted, which is diagnostic of a clay-shoveler’s fracture.
Clay-shoveler’s fracture. A nondisplaced fracture of the C7 spinous process (arrow) is noted, which is diagnostic of a clay-shoveler’s fracture.


 Hangman’s fracture. A, A lateral film of a patient with a hangman’s fracture shows an obvious example of the posterior elements of the C2 vertebral body fractured and displaced inferiorly. B, The film of another patient shows a subtle fracture through the posterior elements of C2 (arrow). A line drawn through the spinolaminal lines of the posterior elements shows the C2 spinolaminal line to be offset in this example.
Hangman’s fracture. A, A lateral film of a patient with a hangman’s fracture shows an obvious example of the posterior elements of the C2 vertebral body fractured and displaced inferiorly. B, The film of another patient shows a subtle fracture through the posterior elements of C2 (arrow). A line drawn through the spinolaminal lines of the posterior elements shows the C2 spinolaminal line to be offset in this example.

 Flexion teardrop fracture. This patient suffered hyperflexion in a car accident and came to the emergency department with severe neurologic deficits. A lateral radiograph of the lower cervical spine shows wedging anteriorly of the C7 vertebral body with some displacement of the posterior vertebral line of C7 into the central canal. A small avulsion fracture off the anterior body is also noted.
Flexion teardrop fracture. This patient suffered hyperflexion in a car accident and came to the emergency department with severe neurologic deficits. A lateral radiograph of the lower cervical spine shows wedging anteriorly of the C7 vertebral body with some displacement of the posterior vertebral line of C7 into the central canal. A small avulsion fracture off the anterior body is also noted.
 Unilateral locked facets. The C6–7 disc space is abnormally widened, and the C7 vertebral body is posteriorly located in relation to C6. Also note the C7 facets, which are dislocated and locked on the C6 facets (arrow). When the facets are perched in this manner, the condition is termed locked facets, which in this example is unilateral.
Unilateral locked facets. The C6–7 disc space is abnormally widened, and the C7 vertebral body is posteriorly located in relation to C6. Also note the C7 facets, which are dislocated and locked on the C6 facets (arrow). When the facets are perched in this manner, the condition is termed locked facets, which in this example is unilateral.


 Unilateral locked facets. A, The C6–7 disc space is slightly wider than normal and the C7 vertebral body is narrower in this view than the C6 vertebral body because of abnormal rotation. B, The facets of C7 are not well identified, but in the tomogram they are shown to be overriding and locked (arrow).
Unilateral locked facets. A, The C6–7 disc space is slightly wider than normal and the C7 vertebral body is narrower in this view than the C6 vertebral body because of abnormal rotation. B, The facets of C7 are not well identified, but in the tomogram they are shown to be overriding and locked (arrow).
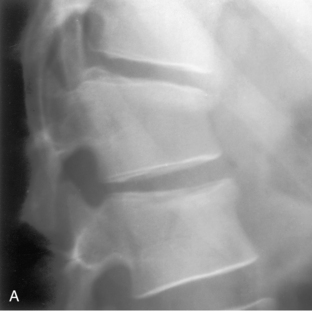
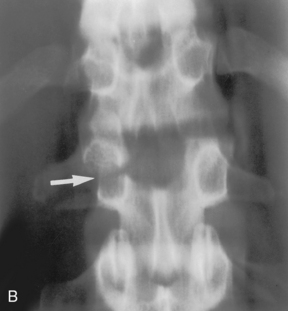
 Seat belt fracture. A, Hyperflexion at the waist can cause anterior wedging of the vertebral body in the lower thoracic or upper lumbar region. By itself, that is somewhat innocuous. B, However, here a horizontal fracture through the right transverse process and pedicle (arrow) resulting from extreme traction during the flexion injury can be seen. When fracture of the posterior elements occurs, this injury is considered unstable and potentially debilitating. Any anterior wedging injury to a vertebral body should have the posterior elements of that level closely inspected for interpedicular space widening.
Seat belt fracture. A, Hyperflexion at the waist can cause anterior wedging of the vertebral body in the lower thoracic or upper lumbar region. By itself, that is somewhat innocuous. B, However, here a horizontal fracture through the right transverse process and pedicle (arrow) resulting from extreme traction during the flexion injury can be seen. When fracture of the posterior elements occurs, this injury is considered unstable and potentially debilitating. Any anterior wedging injury to a vertebral body should have the posterior elements of that level closely inspected for interpedicular space widening.
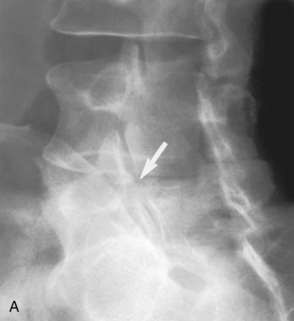
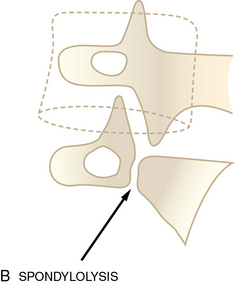
 Spondylolysis. A, An oblique film of the lumbar spine shows a defect in the neck of the Scottie dog at L5 (arrow), which is diagnostic of a spondylolysis. B, This drawing shows the findings more clearly. This has been described as a collar around the Scottie dog’s neck.
Spondylolysis. A, An oblique film of the lumbar spine shows a defect in the neck of the Scottie dog at L5 (arrow), which is diagnostic of a spondylolysis. B, This drawing shows the findings more clearly. This has been described as a collar around the Scottie dog’s neck.
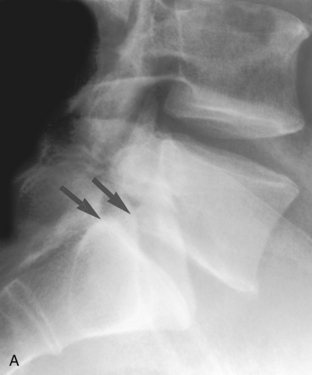
 Spondylolisthesis. A, A lateral film of the lumbar spine shows the L5 vertebral body is slightly anteriorly offset on the S1 body as noted by the posterior margins (arrows). B, The drawing shows the findings more clearly. Because the offset is less than 25% as measured by the length of the S1 end-plate, it is termed a grade 1 spondylolisthesis. A grade 2 offset is more than 25% but less than 50% of the length of the S1 end-plate.
Spondylolisthesis. A, A lateral film of the lumbar spine shows the L5 vertebral body is slightly anteriorly offset on the S1 body as noted by the posterior margins (arrows). B, The drawing shows the findings more clearly. Because the offset is less than 25% as measured by the length of the S1 end-plate, it is termed a grade 1 spondylolisthesis. A grade 2 offset is more than 25% but less than 50% of the length of the S1 end-plate.

 Anterior wedge compression fracture. Anterior compression of this lower T-spine vertebral body (arrow), which may or may not be acute, is present. If the patient has pain in this area, it is most likely acute and must be protected with a back brace until the symptoms abate.
Anterior wedge compression fracture. Anterior compression of this lower T-spine vertebral body (arrow), which may or may not be acute, is present. If the patient has pain in this area, it is most likely acute and must be protected with a back brace until the symptoms abate.
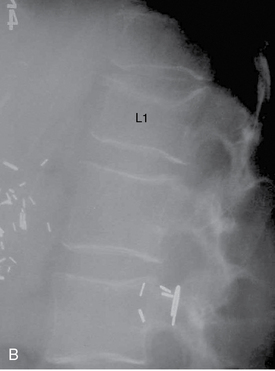
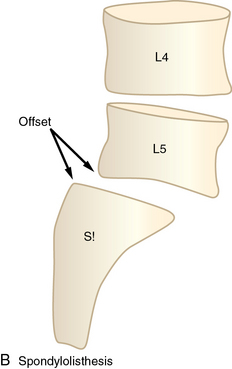
 Kummel’s disease. A, Very minimal anterior wedging of the L1 vertebral body is noted by comparing the height of the anterior body versus the posterior height. This patient had been in an auto accident and complained of back pain. No treatment for his back was given. B, After several weeks of continuing pain the patient sought treatment for leg weakness, which proceeded to paraplegia. A spine film now shows progression of the vertebral body collapse of L1. This almost certainly could have been avoided with simple bracing of the spine after the initial injury.
Kummel’s disease. A, Very minimal anterior wedging of the L1 vertebral body is noted by comparing the height of the anterior body versus the posterior height. This patient had been in an auto accident and complained of back pain. No treatment for his back was given. B, After several weeks of continuing pain the patient sought treatment for leg weakness, which proceeded to paraplegia. A spine film now shows progression of the vertebral body collapse of L1. This almost certainly could have been avoided with simple bracing of the spine after the initial injury.


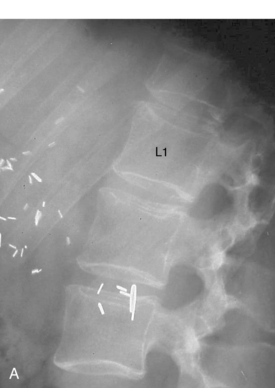
 Spine fracture in ankylosing spondylitis. A, A lateral spine plain film after trauma shows fusion of the spine anteriorly, which was secondary to ankylosing spondylitis. Minimal anterior wedging of the L1 vertebral body, which was overlooked, is present. B, Two weeks later a CT scan of the spine was performed because of the sudden onset of paralysis. This axial image through L1 shows a fracture of the posterior elements, which was undoubtedly present on the initial visit to the emergency department. Patients with ankylosing spondylitis need to be examined closely for any back pain after trauma, and CT or MRI scans should be obtained if any pain is present.
Spine fracture in ankylosing spondylitis. A, A lateral spine plain film after trauma shows fusion of the spine anteriorly, which was secondary to ankylosing spondylitis. Minimal anterior wedging of the L1 vertebral body, which was overlooked, is present. B, Two weeks later a CT scan of the spine was performed because of the sudden onset of paralysis. This axial image through L1 shows a fracture of the posterior elements, which was undoubtedly present on the initial visit to the emergency department. Patients with ankylosing spondylitis need to be examined closely for any back pain after trauma, and CT or MRI scans should be obtained if any pain is present.
Hand and wrist
Trauma





