Trauma
SLIPPED CAPITAL FEMORAL EPIPHYSIS
SPONDYLOLISTHESIS AND SPONDYLOLYSIS
Chapter Format
This chapter reviews trauma to the skeleton. The emphasis is presented under the heading of bone and joint trauma. Multiple tables list fractures and soft-tissue injuries stratified by body region. Other topics related to trauma, such as battered child syndrome, spondylolisthesis, and osteochondritis dissecans, also are discussed under separate headings.
Imaging
Imaging of skeletal trauma is dominated by plain film radiology. Plain film offers excellent evaluation of small or simple anatomy, and provides a first step in imaging more complex anatomy, to be followed by more sophisticated modalities.
Computed tomography (CT) is beneficial for exhibiting complex anatomy, especially the head, calcaneus, acetabulum, and spine. CT provides imaging directly in an axial plane and is commonly reformatted to view the anatomy in other planes. CT is particularly adept at demonstrating cortical bone. Linear tomography is useful for detailing fractures and is often applied to the upper cervical spine and wrist.
Magnetic resonance imaging (MRI) is performed if a significant soft-tissue component is indirectly seen or suspected clinically, if visualization of bone marrow is needed, or if neurologic findings are present. Like CT, MRI also provides axial imaging, but goes further to offer true multidimensional imaging in other planes (e.g., frontal, sagittal). MRI is noninvasive and has the advantage of being able to evaluate a wide range of both intraarticular and extraarticular anatomy.
Bone and Joint Trauma
Background
Bone Injuries.
Traumatic lesions of the skeleton are common to all ages and patient populations. Traumatic bone insult may be fairly innocuous, manifesting as little more than a bone bruise or may be severe enough to break the bone and produce a fracture. A fracture is defined as an interruption of the structural integrity and anatomic continuity of bone, manifesting as minor cracks, crumpling, splintering, or complete disruption of the cortex. If the overlying skin remains intact, the fracture is closed (or simple); if the skin is disrupted, the fracture is open (or compound).
Fractures are oriented transverse, longitudinal, or oblique to the long axis of the bone, largely dictated by the force applied to the bone. Spiral fractures result from rotational stresses and have an oblique fracture plane encircling the long axis of the bone. Complete fractures extend through the bone and produce at least two fragments. Those with more than two fragments are known as comminuted fractures. Because of the pliability of long bones in children, a fracture may not appear to extend through the entire bone. If a portion of the bone remains intact, the fracture is incomplete. Incomplete fractures of long bones present with either distraction (greenstick) or impaction (buckle or torus) of the completely fractured cortical side of the bone (Table 10-1). Incomplete fractures are named according to their radiographic appearance. That is, they may extend completely through the bone anatomically, but routinely appear to only “incompletely” extend through the bone on the corresponding radiograph.
TABLE 10-1
DESCRIPTIVE TERMINOLOGY OF FRACTURES
| Types of Fracture | Comments |
| Avulsion (Figs. 10-6 and 10-7) | An avulsion fracture occurs as the attachment of a ligament or tendon is pulled from the bone, taking a small bone fragment with it. The fragments are often highly serrated. |
| Closed (simple) | A closed fracture does not penetrate the skin. |
| Comminuted (Fig. 10-8) | A comminuted fracture has more than two fragments. A butterfly fragment describes a triangular-shaped bone fragment split from one of the main fragments. |
| Complicated | A complicated fracture may be “complicated” by damage to nerves, vessels, and viscera. |
| Corner (chip) (Fig. 10-9) | A corner fracture describes a fracture of the articular margin of a bone, releasing a small fragment. |
| Diastatic (Fig. 10-10) | A diastatic fracture is a separation injury of synarthrodial joints (e.g., pubic symphysis, proximal, and distal tibiofibular joints). |
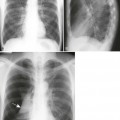
| Greenstick (Fig. 10-11) | A greenstick fracture is an incomplete fracture of long bones that is seen in children. The concave side of the bending bone is intact and the opposite convex cortex is distracted with an obvious ragged fracture line. |
| Impaction (crush) (Fig. 10-12) | An impaction fracture occurs when one fragment is driven or telescoped into the cancellous bone of the adjacent fragment. There are two types: (a) depression fractures, in which one bone is driven into the adjacent bone (e.g., occurs when the femoral condyle is driven into the softer tibial plateau), and (b) compression fractures, in which the articular surfaces of a bone approximate one another (e.g., compression fracture of the vertebral body). Like stress fractures, impaction fractures present as radiodense, not radiolucent, defects. |
| Incomplete | In this fracture, the fracture line radiographically appears not to traverse or penetrate the entire bone (periosteum may be intact); most often occurs in children in whom the soft, pliable bones bow in response to the applied force. Greenstick and torus are two examples of incomplete fractures (see entries in this table and also in Table 10-9). |
| Insufficiency (Fig. 10-13) | This is a stress fracture of diseased bone; that is, repeated application of normal loads resulting in an abnormal response of bone. |
| Intraarticular (Fig. 10-14) | An intraarticular fracture extends through the articular surface of a joint. Fractures that penetrate the joint may be complicated by the chondrolytic consequences of intraarticular blood. |
| Oblique | This is a fracture line that is oriented oblique to the long axis of the bone but does not exhibit a spiral path. |
| Occult | This is clinical, but not radiographic, evidence of fracture. Radiographic evidence usually develops within 1 to 2 weeks of injury. |
| Open (compound) | An open fracture penetrates the skin. |
| Pathologic (Figs. 10-15 and 10-16) | A pathologic fracture occurs in bone that has been weakened by disease. The disease may be localized (e.g., infection, tumor, disuse) or more generalized (e.g., osteogenesis imperfecta, osteoporosis, rickets, osteomalacia). Pathologic fractures often are oriented transverse to the long axis of the bone. An insufficiency fracture is a pathologic fracture that results from repeated application of normal subthreshold forces. |
| Pseudoarthrosis | Pseudoarthrosis describes the articulation that develops between bone fragments after nonunion. |
| Spiral (Fig. 10-17) | A spiral fracture is a fracture line obliquely oriented and coils around the long axis of the bone. |
| Stellate | Stellate describes a fracture seen in flat bones or the patella where the fracture lines extend radially from a central point. |
| Stress | There are two types of stress fractures: fatigue and insufficiency. Fatigue fractures result from repeated applications of abnormal stresses on bones of normal elastic resistance. Insufficiency fractures result from repeated application of normal stresses on bones of abnor mal elastic resistance. Common stress fractures are listed in Table 10-2. |
| Torus (buckle) | A torus fracture is an incomplete fracture of long bones seen in children. It presents as a cortical bulge on the concave side of a bending long bone and is common in the distal radius. |
| Transverse | A transverse fracture line is oriented perpendicular to the long axis of the bone. Fracture of transverse orientation suggests underlying osseous pathology (e.g., Paget disease, metastatic bone disease). |
| Unstable/Stable | A biomechanically unstable fracture tends to displace once it has been reduced nonsurgically and immobilized; a stable fracture does not. A neurologically unstable fracture has a propensity for neurologic insult. |








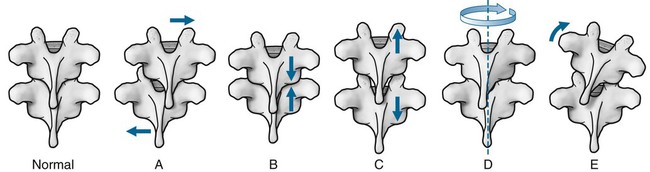
Reporting on fractures and dislocations should encompass such information as which bone is involved, where in the bone the fracture is found, fragment apposition (shift), alignment (tilt), rotation (twist), distraction (separation), and any resulting alteration in limb length. Figures 10-1 to 10-3 show descriptive terms for long bone and vertebral injuries.
Types of Fractures.
Fractures develop from a single application of stress outside of the normal range of physiologic limits (traumatic, acute, or strain fracture), repetitive application of stress within the normal range of physiologic limits (fatigue or stress fracture), or the single (pathologic) or repeated (insufficiency) application of stress within the normal range of physiologic limits but applied to bone that has been weakened by underlying pathology (e.g., Paget disease, metastatic bone disease). Tables 10-2 through 10-10 are constructed to provide examples and more detail about stress fractures (Table 10-2), Salter-Harris fractures (Table 10-3), and selected topics of bone and joint injury sorted by anatomic region: skull and face (Table 10-4), cervical spine (Tables 10-5 and 10-6), thoracic spine and thorax (Table 10-7), lumbar spine (Table 10-8), upper extremity (Table 10-9), and pelvis and lower extremity (Table 10-10).
TABLE 10-2
COMMON STRESS FRACTURES AND ASSOCIATED CAUSES200
| Skeletal Location | Related Activities |
| Calcaneus (Fig. 10-18) | Jumping, parachuting, prolonged standing, recent immobilization |
| Cervical and thoracic vertebrae | Shoveling action, classically clay shoveling (spinous processes) |
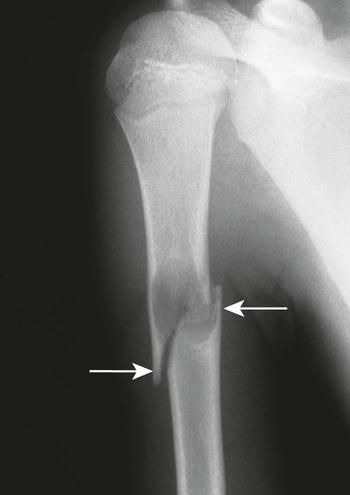
| Femur (shaft and neck) (Fig. 10-19) | Ballet, long-distance running, marching, gymnastics |
| Fibula (shaft) | Long-distance running, jumping, parachuting |
| Hamate (hook) | Golfing, racquet sports, baseball batting |
| Humerus (distal shaft) | Throwing a ball |
| Lumbar vertebrae (pars interarticularis) | Ballet, weightlifting, football, scrubbing floors, lumbar hyperextension |
| Metatarsal shaft (Fig. 10-20) | Marching, prolonged standing, ballet |
| Navicular | Marching, long-distance running |
| Patella | Hurdling |
| Pelvis (obturator ring) (Fig. 10-21) | Stooping, bowling, gymnastics, ballet |
| Ribs (Fig. 10-22) | Carrying heavy pack, golfing, coughing |
| Scapulae (coracoid process) | Trapshooting |
| Sesamoid bones | Prolonged standing |
| Tibia (shaft) (Figs. 10-23 to 10-25) | Long-distance running |
| Ulna (coronoid process) | Pitching a ball, using a pitchfork, propelling a wheelchair |
TABLE 10-3
CLASSIFICATIONS OF EPIPHYSEAL INJURIES (SALTER-HARRIS I–V AND RANG-OGDEN VI–IX)*
| Classification | Description and Comments |
| Type I (Fig. 10-26) | Tansverse fracture through the physis. The physis is widened. Usually the widening is imperceptible on radiographs. No residual growth deformity is expected. |
| Type II (Figs. 10-27 to 10-29) | Transverse fracture through most of the physis and a small portion of the metaphysis. The separated portion of the metaphysis (known as a Thurston-Holland fragment) remains in contact with the epiphyseal fragment. It does not result in residual functional deficiency of limb length. Type II is the most common Salter-Harris type. |
| Type III (Fig. 10-30) | Transverse fracture through a portion of the physis and a portion of the epiphysis. Because this fracture extends into the joint space, it can introduce blood with chondrolytic joint derangement from the hemarthrosis. Type III fractures pass through the hypertrophic layer of the physis, leading to damage of the reproductive layers of cartilage and resulting in possible growth retardation. Although serious consequences are possible, the type III fracture usually heals with little real deficiency. Surgery may be required. |
| Type IV | Oblique or spiral fracture through the metaphysis, physis, and epiphysis. Along with the type III, the type IV fracture extends into the joint with possible joint destruction as a consequence of hemarthrosis. It may cause bone deformity of the bone growth by injuring the growing layers of the physis. |
| Type V | Compression injury of the physis with no associated fracture to the epiphysis or metaphysis. It may result in serious injury with common residual shortening of the involved limb because of injury to the growing layers of cartilage. Type V fractures are practically impossible to see with plain film radiography initially. Retrospectively, they are suggested by the findings of limb shortening or premature closure of the physis. MRI, bone scan, or CT is warranted for initial detection. |
| Type VI | Rare injury to the perichondral elements (portion of physis shears off) promoting reactive bone formation. |
| Type VII | Injury to the epiphysis and articular cartilage without involving the adjacent physis or metaphysis (e.g., osteochondritis dissecans). |
| Type VIII | Rare injury exclusive to the metaphysis, with potential implications to endochondral bone formation. |
| Type IX | Rare injury to the periosteum, with potential implications to intramembranous bone growth. |
*SALTR is a commonly applied mnemonic to remember the order of the first five classifications. The mnemonic only works if one visualizes a bone where the epiphysis is below the metaphysis (e.g., distal femur or radius in anatomic position). The SALTR letters stand for simple, above, lower, together, and reduction (of physis).
TABLE 10-4
FRACTURES OF THE SKULL AND FACE
| Fracture | Comments |
| Skull | |
| Basilar skull fracture | Results from a blow to front of skull; difficult to detect with plain film radiography. As is the case with all skull and face fractures, CT is usually needed to demonstrate the injury. The air–fluid level or opacification of sphenoid sinus is the most reliable sign of basilar skull fractures.203 |
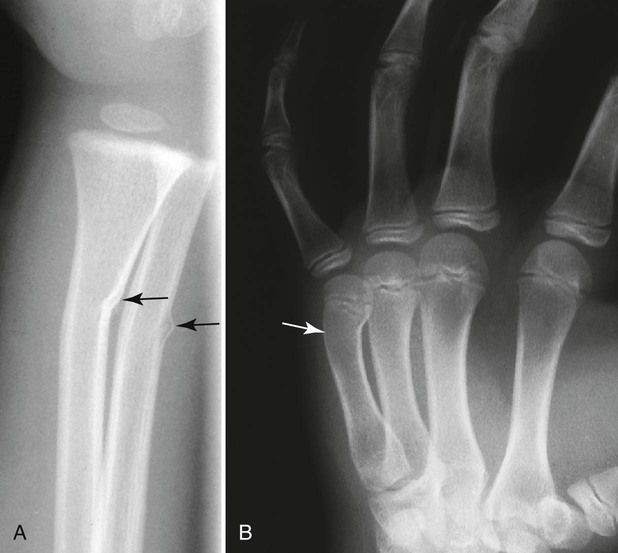
| Depressed fracture (see Fig. 10-12) | Results from an impact injury to the cranial vault causing depression of fragments, and represents 15% of all skull fractures; usually it is located in the frontoparietal area. Thirty-three percent are associated with dural tears that are suggested when fragments are depressed beyond 5 mm of the skull surface or beyond the level of the inner table.243 The plasticity of a child’s skull allows depression without obvious fracture, known as a ping-pong fracture. |
| Diastatic fracture (see Fig. 10-10) | A diastatic fracture results from trauma that causes widening of the cranial sutures, and accounts for 5% of skull fractures,101 most commonly lambdoid and sagittal sutures. They often are associated with, or are extensions of, linear fractures. |
| Leptomeningeal cyst | Represents fracture complication resulting from arachnoid mater extending through a tear in the dura mater, into a skull fracture. The pulsatility of the cerebrospinal fluid may inhibit fracture healing and, at times, erode the perimeter of the fracture, giving the appearance of a “growing fracture.” |
| Linear fracture | A linear fracture represents a lucent line of several centimeters, and represents 80% of all skull fractures; usually occurs in the parietal or temporal bone and may cross sutures and vascular grooves. It does not exhibit a branching pattern as is seen with normal vascular channels.206 |
| Pneumocephalus | Pneumocephalus is a fracture complication resulting from air in the subarachnoid space. Trauma to the walls of the air-filled paranasal sinus or mastoid air cells permits dissection of air into the subarachnoid space. Other causes include infection, neoplasm, or surgery. |
| Face | |
| LeFort fractures (Fig. 10-31) | LeFort fractures occur along three planes of weakness in the facial skeleton. All types are unstable, bilateral, involve the pterygoid processes, and separate a fragment of bone from the face. LeFort type fracture I is a transverse fracture through the maxilla separating the upper dentition from the rest of the head (floating palate).63 LeFort type fracture II is an oblique fracture through the maxilla separating a pyramid-shaped segment of the midface.62 LeFort type fracture III is a nearly vertical fracture through the nasal bones and septum, maxilla, and orbits completely separating the face from the skull.62 |
| Mandible fracture | A mandible fracture is the third most common facial fracture (after nasal and maxilla), usually occurring in the body (40%), angle (30%), and condyloid process (20%) of the mandible,159 presenting bilaterally17,249 and often is multiple. Mandible fractures are seen well with CT or a panoramic projection with linear tomography. Physical assault and automobile accidents account for 80% of mandibular fractures.17,157 |
| Nasal bone fracture (Figs. 10-32 and 10-33) | Fracture of the nasal bones are the most frequent facial fracture.123,220 They nearly always exhibit a transverse orientation. Fragments usually are depressed and displaced. Nasofrontal sutures or longitudinal grooves often are mistaken for fractures. |
| Orbital fracture (Fig. 10-34) | Orbital fracture occurs as an isolated fracture to the rim or walls (blowout) of the orbit, or as components of more complex tripod or LeFort fractures. Orbital floor fractures may be complicated by entrapment of the inferior rectus and inferior oblique muscles. Medial wall fractures may be complicated by entrapment of the medial rectus. Closed cavity traumas correlate to eye injuries. Open cavity injuries have a risk of infection via communication with the sinuses. |
| Tripod (trimalar) fracture (Fig. 10-35) | Conflicting reports exist as to whether the tripod fracture is the most common fracture of the face206 or second most common fracture of the face (following nasal bones).123,220 The term tripod is used to describe the three limbs of the zygoma that are fractured, separating the zygoma from its frontal, temporal, and maxillary attachments by a direct blow to the malar prominence.139 They are isolated and usually comminuted. Fractures of the zygomatic arch are caused commonly by a direct blow to the side of the face. |
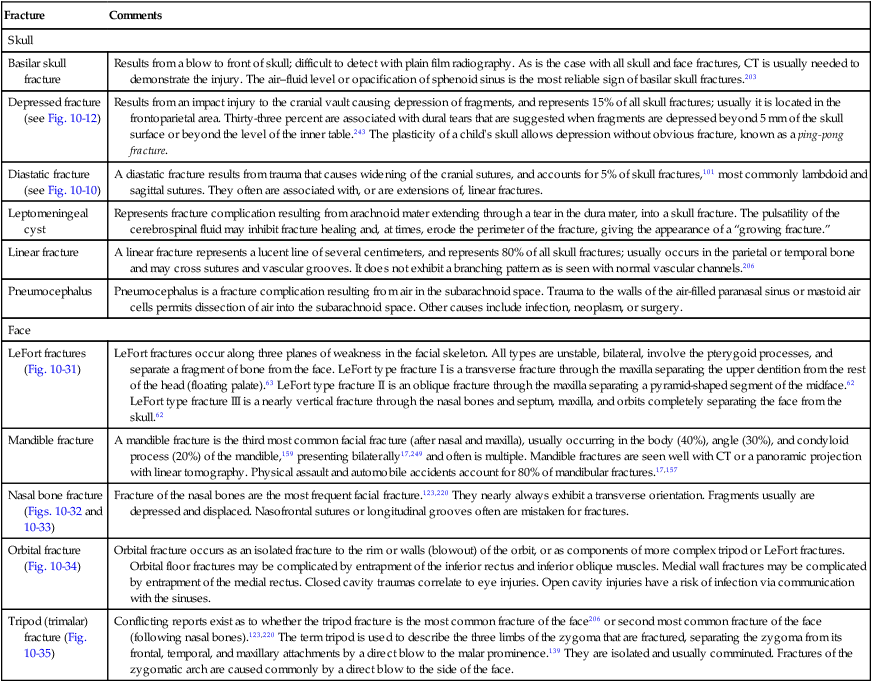
TABLE 10-5
FRACTURES AND DISLOCATIONS OF THE CERVICAL SPINE
| Injury | Comments |
| Fractures | |
| Occipital condyle fracture | A combination of axial compression and lateral bending may result in avulsion or compression fractures of the occipital condyles. These injuries are associated with cranial nerve deficits. This area of complex anatomy is difficult to visualize on plain film, requiring CT to determine if fracture is present. |
| Atlas posterior arch fracture (Fig. 10-36) | Fracture of the posterior arch of the atlas is defined by vertical fractures secondary to a cervical hyperextension injury and resulting compression of the weaker posterior arch of the atlas between the larger anatomic structures of the spinous process of C2 and occiput. Generally, the mechanism of cervical trauma provides a clue to the type of resultant injury (Box 10-2). The fracture line is seen on the lateral cervical view, and the APOM (anterior-to-posterior open-mouth) projection appears normal. Because the transverse atlantal ligament and anterior arch of the atlas are intact, posterior arch fractures are stable and generally without risk of neurologic deficit. They are the most common fractures of the atlas.225 |
| Jefferson fracture (Figs. 10-37 to 10-41) | A Jefferson fracture is a bursting fracture of the atlas involving both the posterior and anterior arches secondary to an axial force.85,120 It is indicated by lateral offset of lateral masses on the C2 articulations as seen in the frontal projection. Offset of more than 7 mm may indicate rupture of the transverse atlantal ligament and resulting instability (Box 10-3),202 a common accompanying injury and strong positive predictor of associated neurologic involvement. There is usually a marked distention of the precervical soft tissue as noted on the lateral cervical projection. At times its diagnosis may be missed because of lack of marked neurologic signs, or the APOM radiograph, which is pathognomonic for the diagnosis, is often inadequate or not obtained.130 |
| Odontoid process fracture (Figs. 10-42 to 10-46) | Odontoid fractures represent approximately 50% of all C2 fractures206 and are divided into three types based on location. Type I is an avulsion of the tip of the odontoid process. Type II is a transverse fracture at the base of the odontoid process and is the most common type. Type III is a fracture of the C2 body, below the base of the odontoid process. Type I is mechanically stable. Type II often is associated with nonunion because of poor regional blood supply. Types II and III may result in cord compression from posterior migration of the odontoid fragment directly, or from the resulting guillotine effect on the cord from the anterior translation of the posterior arch of the atlas. |
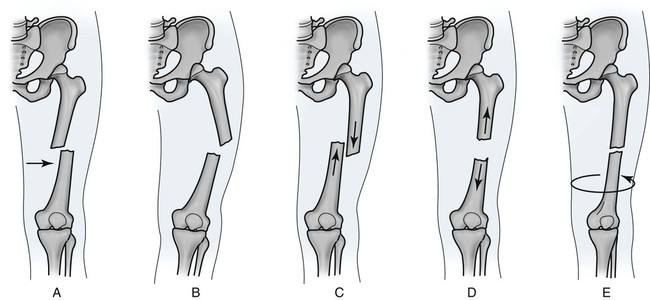
| Hangman fracture (traumatic spondylolisthesis) (Figs. 10-47 to 10-49) | Hangman fracture describes a bilateral fracture of the posterior arch of axis, usually the pedicles or pars interarticularis (fracture to the latter is also termed traumatic spondylolisthesis).214 Hangman fracture occurs from cervical hyperextension, usually from a car accident, although the historic example is hanging a person at the gallows (hence the name). Hangman fractures represent approximately 25%206 of all C2 fractures, and are difficult to detect radiographically at times. They typically result in anterior displacement of C2 on C3 that can be classified into three types: type 1 is minimal to 3 mm of anterior displacement with no evidence of focal kyphosis; type 2 is more than 3 mm of anterior displacement and focal kyphosis; type 2a is severe angulation but less than 3 mm anterior displacement; and type 3 is severe angulation and unilateral or bilateral dislocation of the C2-3 facets.146 Generally displacement of more than 3 mm indicates instability; cord compression is a concern, but does not commonly realize because the spinal canal is maintained or enlarged.169 Angiography to detect intimal injury of the vertebral arteries, and possibly anticoagulation therapy, may be necessary when the fracture involves the transverse foramina.169 |
| Teardrop fracture (Figs. 10-50 and 10-51) | Teardrop fractures most often occur at C2, produced from hyperflexion or hyperextension forces that avulse and displace a small, usually triangular segment, of the inferior, less commonly superior, vertebral body.18 Although both the flexion and extension mechanisms are serious injuries, the flexion injury disrupts the posterior ligament system, promotes instability, and is more often associated with neurologic deficient, resulting in acute anterior cord syndrome in nearly 90% of cases.104 The extension teardrop fracture involves the anterior longitudinal ligament and anterior annulus fibrosis, yet the posterior ligament system remains intact; therefore it is a stable injury with flexion and unstable with extension. |
| Articular pillar fracture (Fig. 10-52) | Fracture of the articular pillar usually follows a hyperextension and rotation injury. Most commonly it occurs at the C6 and C7 levels. In the lateral cervical projection, the articular pillar may appear as a double shadow (“double outline” sign), also a feature of unilateral facet dislocation. Fracture of the lamina may be seen as an isolated injury or as accompanying articular pillar fractures. |
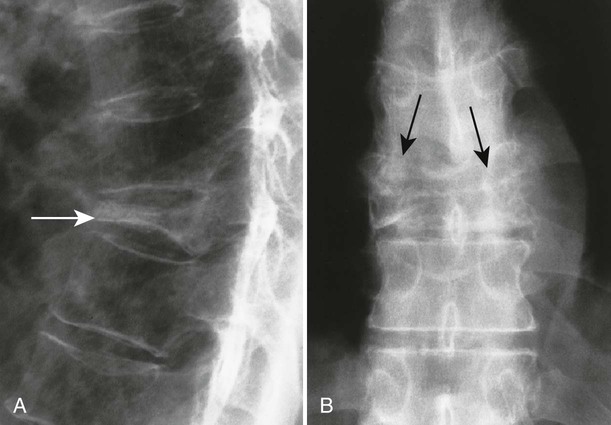
| Burst fracture (Figs. 10-53 and 10-54) | A burst fracture is a compression fracture in which axial loads drive portions of the intervertebral disc into the adjacent vertebra, producing a comminuted, circumferentially expanded fracture that may demonstrate posterior displacement of fracture fragments into the vertebral canal, often producing neurologic deficits.6 These fractures usually have a sagittal component,131 and often demonstrate an increased interpeduncular distance in the frontal projection.6 Nearly 50% occur at the L1 level.6 |
| Clay shoveler’s fracture (coal shoveler’s) (Figs. 10-55 to 10-59) | Clay shoveler’s fracture is an oblique avulsion of the spinous process, occurring at the level of C6-T1. It is best seen in the lateral projection, and appears as a “double-spinous” sign in the AP projection. Irregularity and distraction of the fragment differentiate fracture from nonunion of secondary growth center of the spinous process that often occurs at lower cervical levels, or dystrophic calcification of the nuchal ligament (nuchal bones). |
| Dislocations | |
| Atlantoaxial dislocation (Figs. 10-60) | An atlantoaxial dislocation results from acquired or congenital damage of the transverse atlantal ligament that produces anterior translation of the atlas, producing a guillotine effect on the cord.234 When trauma is the cause, the force is typically from hyperflexion. Atlantoaxial dislocation is indicated radiographically by an atlantodental interval larger than 3 mm in adults or 5 mm in children. |
| Atlantooccipital dislocation | Dislocation of the atlantooccipital joint is rare, usually occurring secondary to cervical hyperextension injury. An anterior direction of dislocation is most common, and usually results in immediate death from respiratory failure associated with brainstem injury. |
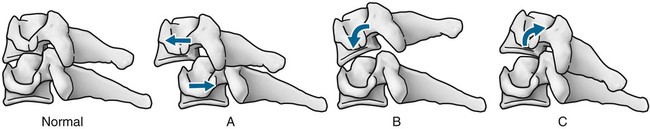
| Facet dislocation (Figs. 10-61 to 10-69) | Unilateral facet dislocation usually is a stable lesion resulting from a flexion rotation injury. It occurs most often at the C4 to C7 level. The dislocated inferior facet appears “locked” or “perched” anterior to the superior articular process of the segment below. The articular pillars of the dislocated segment simulate a “bow tie” appearance in the oblique projection and “fanning” spinous processes in the lateral projection; decreased range of motion, accompanying fractures (e.g., pillar fracture),18 and radicular symptoms may be present.270 Bilateral facet dislocation is a usually unstable lesion resulting from a hyperflexion injury. It occurs most often at the C4 to C7 level. In the lateral projection, bilateral facet dislocation exhibits “fanning” of the spinous processes, narrowed disc space and anterolisthesis usually are evident, and cord damage is common.104 Bilateral and unilateral dislocation have a similar incidence rate.87 However, unilateral facet dislocation is more likely to present to private chiropractic, orthopedic, or other nonemergent practice settings. |
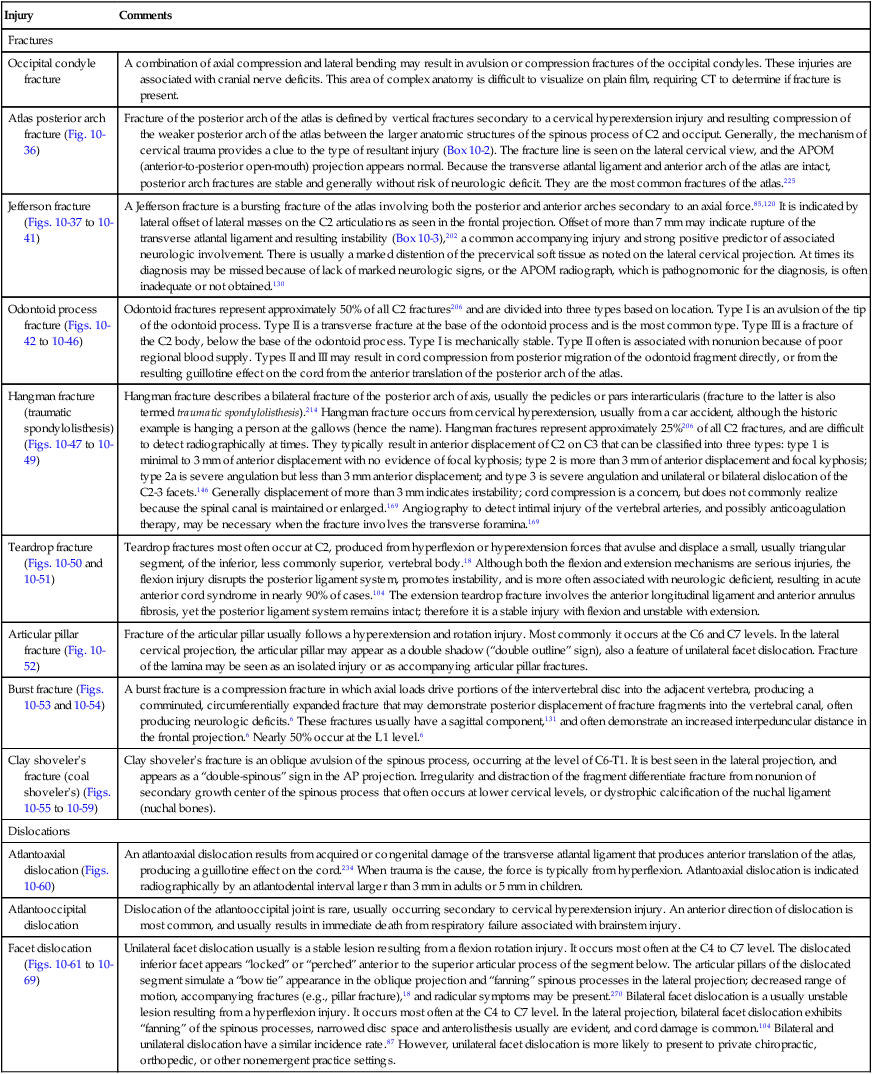
TABLE 10-6
CERVICAL ACCELERATION-DECELERATION SYNDROME OR “WHIPLASH SYNDROME”
| Injury | Comments |
| Cervical “whiplash” syndrome or cervical acceleration-deceleration syndrome (CADS) | Whiplash is a medicolegal term first used by Crowe in 1928 to describe the effects of rapid acceleration-deceleration mechanism of energy transfer to the neck.48 It may result in bony or soft-tissue injuries. According to the Quebec Task Force,229 there are four grades of whiplash injury: |
|
0: No complaint about the neck I: Neck complaint of pain and stiffness, no signs II: Neck complaint, musculoskeletal signs
|
Imaging assessment of the cervical trauma patient begins with plain film radiography. Generally clues to cervical spine injury include obvious fracture or dislocation, axial rotation of a vertebra, increased atlantodental interval beyond 3 mm (>5 mm in children), loss or reversal of the normal cervical lordosis, acute angular kyphosis, interspinous process gapping, widened retropharyngeal space (>6 mm at C2), widened retrotracheal space (>22 mm at C6), displacement of the prevertebral fat stripe,55 lateral tracheal deviation, and soft-tissue emphysema. The S-shape curvature—defined as hypolordosis in the upper region and kyphosis in the lower region of the sagittal cervical curvature—of the cervical spine has been qualitatively associated with whiplash injuries; however, it has not been subjected to detailed quantitative analyses.97,187 Griffiths found high sensitivity (81%) and specificity (76%) to whiplash injuries when the radiographs exhibited greater than 10 degrees of intersegmental motion or more than 12 mm of spinous process fanning.99 These measures are difficult to directly apply to the young patient where ligamentous laxity is the norm and abnormally large measures may be physiologic, not pathologic.White and Panjabi262 describe cervical injury with subsequent neurologic damage as a clinical unstable situation. Clinical instability is defined on the neutral 72-inch focal film distance lateral radiograph as more than 3.5 mm of displacement of one segment relative to the position of the subadjacent vertebra or greater than 11 degrees intersegmental rotation relative to the rotation of the adjacent vertebrae.262 With use of flexion–extension radiographs, relative translations greater than 3.5 mm or more than 20 degrees of sagittal plane rotation is abnormal. Clinical instability generally is regarded as a contraindication to same-level chiropractic adjustment and relative contraindication to distal, but related areas. Dai51 found that cervical segmental instability may be associated with early degeneration of the involved intervertebral disc.Radiographs remain as the modality of choice for the initial evaluation of whiplash-type injuries72; however, plain film radiographs may not reveal significant trauma.271 For example, up to 20% of fractures are missed on initial plain film studies; therefore it is important to proceed to a CT scan if there are significant historic indicators of trauma and suspicious clinical presentation.132 CT is particularly useful for reviewing complex anatomy and clinically suggested fracture, and in circumstances where quality radiographs are difficult to obtain (e.g., large-body habitus or structural deformity as with scoliosis), MRI and bone scans may be useful to exhibit radiographically occult fractures.Disc pathology is a contributing factor in the development of chronic symptoms after whiplash injury. However, because of the high proportion of false-positive results, it is best to reserve MRI examination for patients with persistent upper extremity pain and neurologic deficits.21,191 Therefore, MRI is most useful for chronic pain syndromes (>6 months) and to evaluate the soft-tissue elements of the spine, including the cord, disc, and ligaments.According to the National Emergency X-Radiography Utilization Study (NEXUS) study criteria, the patient’s cervical spine injury is considered low risk for fracture if it exhibits the following criteria: no posterior midline cervical spine tenderness, no evidence of intoxication, normal level of alertness, no focal neurologic deficit, and no painful distracting injuries.108 If radiographs are indicated, evaluation begins with the standard three-view series (anteroposterior [AP] lower cervical, anterior-to-posterior open-mouth [APOM], and lateral). The lateral view is most helpful. Additional views, such as oblique, swimmer’s, flexion–extension, and odontoid may be included. Oblique projections often are added if there is a neurologic component to the clinical presentation. Flexion–extension views are indicated if assessment of intersegmental biomechanics is warranted. When performing flexion–extension views, care should be taken on the part of the examiner not to force the injured patient in either flexion or extension, and possibly injuring the patient further. The traditional seven views (neutral lateral, AP lower cervical, AP open-mouth, right and left oblique, flexion, and extension) are no longer routinely advocated. If plain film imaging is warranted, a three-view series (lateral, APOM, and AP lower cervical) with possible helical CT is likely to be more informative.151 If warranted, flexion and extension views are best applied 7 to 10 days after injury, at which time confounding muscle spasm has largely subsided. However, MRI is more accurate in evaluating ligamentous injury and very useful for examining any associated neurologic involvement. The expected clinical outcomes to whiplash injury are difficult to accurately predict. Typically patients recover completely.22 However, as many as 20% to 60% of patients exhibit clinical features 6 months after the injury.9,237 Age, gender, baseline pain intensity, and radicular signs and symptoms are important prognostic factors for the outcome of whiplash trauma.43 In addition, there is a significant correlation between a narrowed sagittal dimension of the spinal canal (secondary to fragment retropulsion and edema) and increased severity of concurrent neurologic symptoms.71 A small cervical canal predisposes to an adverse clinical outcome after whiplash injury.125 Spinal cord injury without radiographic abnormality (acronym SCIWORA) can be a fatal or disabling condition developing from childhood injuries, and most often affects those under the age of 8 or 9 years. A contributing mechanism of injury appears to be the poorly developed cervical musculature that offers little protection to the injured cervical spine. The injuries can be focused on the cervical or thoracic spine, including whiplash-type mechanisms from automobile accidents, sports, and falls. SCIWORA most often represents a diagnosis of exclusion, necessitating a high index of clinical suspicion. The neurologic signs may be delayed or evolve slowly. SCIWORA is a pre-MRI diagnosis of exclusion. By definition, plain film radiographs are negative. MRI is the standard assessment, commonly exhibiting central disc herniation, spinal stenosis, and spinal cord edema.230
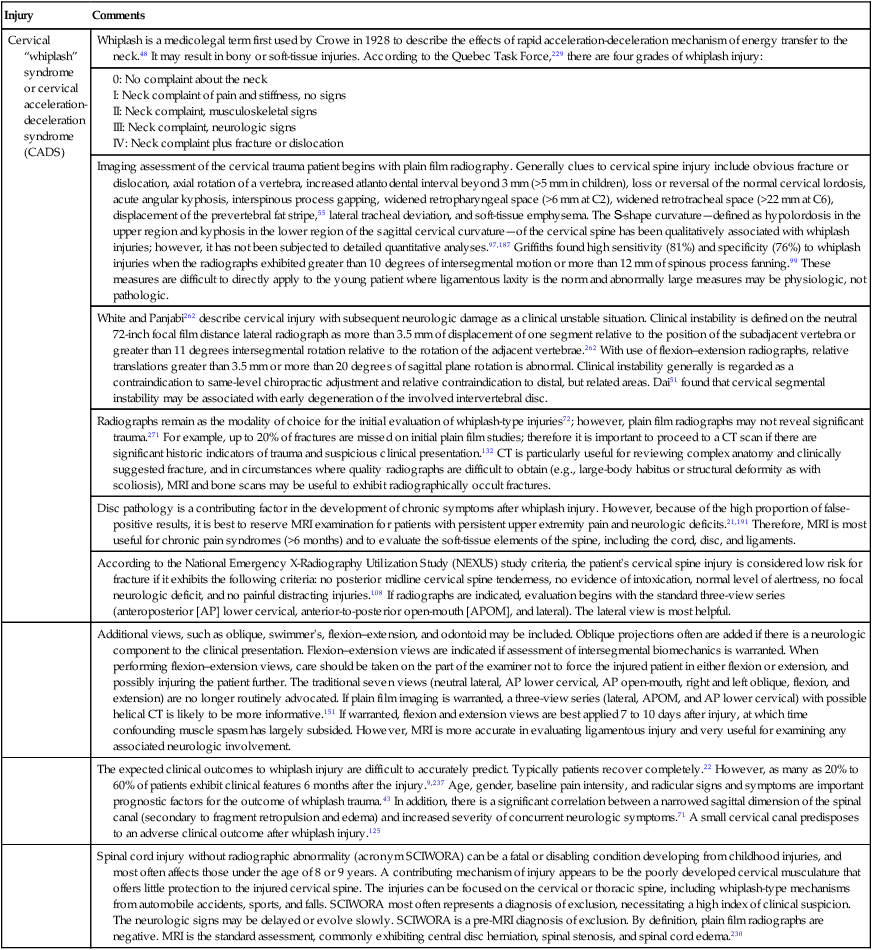
TABLE 10-7
FRACTURES OF THE THORACIC SPINE AND THORAX
| Fracture | Comments |
| Compression Fracture | |
| Flail chest | Flail chest describes the occurrence of multiple fractures of the same ribs, isolating a plate of one or more ribs that are now free to move inward and outward in response to respiration. Posterior flail segments are easier to manage because they are stabilized by the strong scapular musculature, and the patient can rest for longer periods of time more comfortably on his or her back than any other position. (see discussion in Table 10-8). |
| Golfer’s fracture | This describes a lateral rib fracture that occurs when a golf club strikes the ground instead of striking the ball. |
| Rib fracture (Figs. 10-70 to 10-77) | Rib fracture is a common sequela of blunt trauma to the thorax. Motor vehicle accidents are particularly common among adults, whereas physical abuse and falls are common causes among children. Most commonly the sixth, seventh, and eighth levels are involved, more frequent in the posterior and middle two-thirds of the rib. Stress fracture can result from sports (e.g., golf) or chronic coughing. Rib fracture may compromise proper ventilation, or penetrate pleura or lungs, resulting in hemothorax (usually from lacerated intercostal vessels) or pneumothorax. Approximately 60% of rib fractures involve multiple levels; 40% involve only one level. There is a direct correlation between the number of ribs fractured and the associated clinical impact of the injury. When one or two ribs are fractured, mortality is estimated at 5%, but increases to nearly 30% when more than six ribs are fractured.275 There is a 13% to 69% lung-related morbidity rate with multiple rib fractures. Because of their elasticity, a child’s ribs are less likely to fracture. Conversely, senior patients are more likely to experience fractures. Senior women are the most common group to demonstrate nontraumatically induced rib fractures (e.g., coughing). Fractures of the first three ribs are associated with brachial plexus and major vessels; arteriography may be considered.201 Lower rib fractures are associated with solid organ injury; CT may be considered. Fractures of the upper ribs indicate that the patient has experienced severe trauma.192,204 Treatment consists of chest wall stabilization, reduction of the respiratory dead space, and management of any associated pulmonary contusion, pneumothorax, effusion, or other features. It is important to search for visceral complications, which are of more clinical concern than the fractured ribs themselves. Also, costicartilage and costochondral injuries often mimic rib fractures clinically but are invisible on radiographs. |
| Sternal fracture (Fig. 10-78) | Direct frontal force (e.g., steering wheel during automobile accident) most often results in transverse fracture of the sternal body. Hyperflexion injury of the spine most often results in a posterior dislocation of the manubrium at the manubriosternal joint. Forty percent of sternal fractures occur with associated spinal fractures.122 A sternal fracture has a 25% to 45% mortality rate secondary to associated cardiac and great vessel injury. Although sometimes seen on radiographs, CT is needed to detail sternal injuries. |
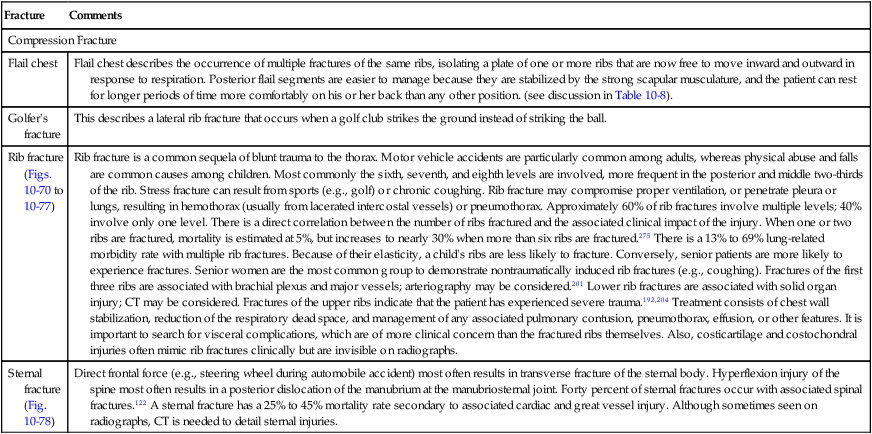
TABLE 10-8
FRACTURES AND DISLOCATIONS OF THE LUMBAR SPINE
| Injury | Comments |
| Chance (seatbelt, lap belt, fulcrum) fracture (Figs. 10-79 and 10-80) | Chance fracture describes a transverse fracture through the spinous process and neural arch that extends into and possibly through the vertebral body. It is named for the British radiologist with the same name.34 Classically it develops from an automobile accident in which flexion forces are applied to the spine while the patient is held down by a lap seatbelt, which acts as a fulcrum to cause the fracture. In the frontal projection a radiolucent region (“empty vertebra”) is created by the separation of the vertebrae. Approximately 50% of cases have associated intraabdominal injuries at the time of presentation. It most often presents at L1 and L2; however, T11 and T12 sometimes are seen. Children have a low center of gravity, causing the middle lumbar levels to be involved more often. |
| Pars interarticularis fracture (Fig. 10-81) | Acute fracture of the pars interarticularis is uncommon, develops from hyperextension injury, and is best seen in the oblique projection. Stress fractures of the region are common, typically occur at L5, are usually bilateral, and promote spondylolisthesis at the same level. |
| Transverse process fracture (Figs. 10-82 and 10-83) | Transverse process fracture is common and often occurs at multiple levels. It is typically present in the upper lumbar levels and in either a vertical or oblique direction. Irregularity of the fracture line and distraction of the fragment differentiate it from nonunion of the transverse process. There is usually an associated history of direct blunt trauma, violent lateral flexion injuries, or avulsion of the psoas muscle. Generally there is little clinical concern for fractures of the transverse process itself. They are considered stable and minor, but there is clinical interest for associated soft-tissue defects to the abdominal or pelvic viscera, particularly renal injury. Approximately 20% of patients with transverse process fractures demonstrate concurrent injury to the abdominal viscera.238 Because of overlying bowel gas and so on, CT may be necessary to fully evaluate the presence of fracture and any associated visceral injury. |
| Vertebral body compression fracture (Figs. 10-84 to 10-93) | Compression fracture most frequently occurs at T12, L1, or L2. Generally compression fracture is noted by a loss of more than 2 mm of anterior vertebral body height compared with the posterior; however, a history of trauma is essential, and differentiates a traumatically induced wedged vertebral configuration from a normal trapezoidal variant in configuration that is common to the T11-L1 levels. The wedged appearance results from forward rotation forces of the traumatic event. In general terms, flexion produces wedge fractures, compression causes burst fractures, shear causes Chance fractures, and rotation causes fracture-dislocations. Compression fracture also may exhibit depression of the vertebral endplates secondary to forces of axial loading. Four classifications (A to D) of compression fracture have been described: involvement of both endplates (A), involvement of superior endplate (B), involvement of inferior endplate (C), and buckling of the anterior cortex of the vertebral body with both endplates intact (D).57 The stability of the lumbar spine after trauma is predicted by the anatomic region of injury, described by three columns (see Fig. 10-92). |
| In a patient older than 40 years of age, there is increased suspicion of a pathologic etiology of the compression fracture related to metastatic bone disease, multiple myeloma, and so on. These aggressive etiologies need to be excluded from fractures caused by osteoporosis or acute injury alone. Differentiation of a pathologic fracture from acute injury alone is aided by a history of malignancy, past radiographs, other sites of involvement (e.g., pedicles), cortical bone destruction, associated soft-tissue mass, collapse of posterior margin of the vertebral body, advanced collapse of the segment (vertebra plana), specialized imaging, and occasionally laboratory work (e.g., multiple myeloma). | |
| Plain film radiographs usually constitute the first step in imaging; the lateral view is most informative. Up to 20% of patients exhibit multiple levels of fracture. CT is used to define the osseous anatomy. MRI is used to assess for underlying pathology, ligamentous injury, and neurologic involvement. On the lateral radiograph, the presence of a horizontal radiopaque zone of condensation and cortical offset “step defect” along the anterior body margin indicate that the fracture is recent (<2 to 3 months);272 vertebral compression fractures with less than 20 degrees of local kyphosis generally are stable and typically do not manifest with neurologic compromise. | |
| Surgical treatment may be considered for patients with documented progression or neurologic compromise; vertebroplasty, first described in 1987, involves the forced injection of low-viscosity polymethylmethacrylate cement into the center of the collapsed vertebral body. Once solidified, the cement significantly improves the structural strength of the vertebral body. Kyphoplasty involves the additional step of using an inflatable balloon inserted into the fractured segment to restore the normal configuration of the segment before injecting the cement. |
TABLE 10-9
FRACTURES, DISLOCATIONS, AND SOFT-TISSUE INJURIES OF THE UPPER EXTREMITIES
| Injury | Comments |
| Shoulder | |
| Fractures | |
| Clavicle (Figs. 10-94 to 10-97) | The clavicle is the most common bone fractured during birth (3% of live births) and childhood272; 80% of fractures occur in the middle, 15% in the lateral, and 5% in the medial third of the bone. Nonunion often results in hypertrophic callus formation that may impinge on the neurovascular bundle exiting the root of the neck (thoracic outlet syndrome). Management is based on immobilization with a figure-eight brace or sling. A stress defect may occur to the distal clavicle as it presents with focal osteolysis after acute injury or repetitive stress, as in weightlifting. |
| Proximal humerus (Figs. 10-98 to 10-100) | Fracture of the proximal humerus occurs at the surgical neck (distal to tuberosities). Proximal humerus fractures are commonly the result of a fall on outstretched hand (acronym FOOSH injury) in an osteoporotic patient. A proximal humerus fracture can be described using the four-part Neer classification system, based on the number of fragments that are displaced. A 1-part Neer describes a proximal humerus fracture (comminuted or not) without any displaced fragments and is treated with a sling. A 2-part Neer has displacement of one fragment (creating two parts) and is treated with closed reduction. A 3-part Neer has two displaced fragments in which at least one tuberosity is in contact with the humeral head and is treated with closed reduction. Last, a 4-part Neer exhibits three displaced segments, requiring open reduction and fixation. Several fractures of the proximal humerus are associated with an anterior dislocation of the proximal humerus, including avulsion of the greater tuberosity (“flap” fracture) and impaction of the posterolateral surface on the inferior glenoid tubercle (Hill-Sachs or “hatchet” defect). |
| Scapula (Figs. 10-101 to 10-104) | A fracture of the scapula is uncommon (approximately 1% of all fractures), usually as a result of direct impact. Most scapular fractures involve the body and neck of the scapula. They are rarely isolated; therefore they may be overlooked because attention is focused on more severe accompanying injuries.95,104 Fractures can be described using four classifications100,117:
I: Glenoid fossa (IA-anterior and IB-posterior). II: Fracture through the glenoid fossa that extends to the lateral border of the scapula. III: Fracture through the glenoid fossa that extends to the superior border of the scapula. IV: Fracture through the glenoid fossa that extends to the medial border of the scapula. Avulsion of the inferior glenoid rim (“Bankart”) is related to anterior dislocation of the humerus. The transscapular (“Y-view”) is usually best to view a scapular fracture. Even if a fracture does not manifest, regional trauma and dislocations may create complex soft-tissue injuries of the related anatomy, warranting MRI follow-up.
|
| Dislocations | |
| Acromioclavicular joint dislocation (Figs. 10-105 to 10-107) | Acromioclavicular (AC) dislocation is most often caused by a fall onto the lateral margin of the shoulder or as a result of severe arm traction, usually occurring without an associated fracture. Six grades of AC injury are recognized. Grade I is a ligamentous sprain with no radiographic evidence of injury. Grade II is rupture of the joint capsule and acromioclavicular ligaments with radiographic evidence of joint space widening and mild elevation of the distal clavicle (<25% displacement). With Grade III the stronger coracoclavicular ligaments are also torn, resulting in increased coracoclavicular distance (>1.3 cm or 40% asymmetry from side to side) and superior displacement (25% to 100% displacement). Grade IV is total dislocation with posterior displacement of the distal clavicle into the trapezius muscle. Grade V is total dislocation with marked superior displacement (>100% displacement) of the distal clavicle. Grade VI is total dislocation with inferior (subacromial or subcoracoid) position of the distal clavicle. Commonly in casual clinical application of the grades, only three grades are used where Grades I and II are similar to the above description, and Grade III may encompass severe strains with extensive elevation of the clavicle. Separation of the joint is enhanced when the patients holds a 10- to 20-lb weight in the hand during the radiographic examination (anteroposterior [AP] with 15 degrees cephalic tube tilt) to draw the arm downward. Depending on the grade, the injury usually is treated conservatively; however, if a patient is physically active (e.g., manual worker or athlete) or does not wish to have the usual step-off bump as a residual cosmetic deformity that is characteristic of the injury, a screw may be surgically placed through the clavicle into the acromion. |
| Glenohumeral dislocation (Figs. 10-108 to 10-110) | Ninety-five percent of glenohumeral dislocations are directed anteriorly, of which 60% are associated with impaction fractures of the posterolateral surface of the humeral head (Hill-Sachs lesion), 15% with avulsion of the greater tuberosity (flap fracture), and less commonly a fracture of the infraglenoid tubercle (Bankart). The radiographic appearance of an anterior humeral dislocation is marked by an intrathoracic (between ribs), subclavicular, subcoracoid (most common), or subglenoid position of the humeral head. Posterior glenohumeral dislocations are less common (about 5%) and anecdotally associated with epileptic or electric shock convulsions. Posterior humeral dislocations are marked by joint widening between the humeral head and anterior glenoid rim (>6 mm, “rim” sign); an impaction of the medial humeral head may be seen (“trough line”).37 Rarely, the humeral head becomes inferiorly displaced under the glenoid process (luxatio erecta), which most often is related to extreme hyperabduction injury. |
| Sternoclavicular joint dislocation | The medial end of the clavicle typically dislocates anteriorly, usually from a blow to the posterior shoulder. A direct anterior blow will dislocate the medial end of the clavicle posteriorly, which is potentially lethal if it encroaches on the great vessels. In those younger than 25 years old, many of these lesions represent separation of the growth plate (Salter-Harris type I) and not true dislocations.206 |
| Soft-Tissue Injuries (Ligaments and Cartilage) | |
| Biceps tendon injury (Fig. 10-111) | The tendon of the long head of the biceps usually appears as a round, low signal intensity structure within the intertubercular groove on the axial MRI images of the shoulder. When not seen within its expected location, rupture or dislocation should be considered; fluid also may be observed within the biceps tendon sheath, representing edema associated with trauma. |
| Glenoid labral tear (Fig. 10-112) | The glenoid labrum often tears when it becomes injured. These tears are most commonly of two types: Bankart lesions and superior labral anterior-posterior (SLAP) lesions. Bankart tears involve the anteroinferior portion of the labrum, usually secondary to an anterior shoulder dislocation when the joint capsule avulses from its glenoid insertion. Bankart lesions predispose to recurrent anterior shoulder dislocations. SLAP lesions occur in the superior margin of the labrum at the point where the long head of the biceps tendon attaches. SLAP lesions occur most commonly from falls on an outstretched hand. SLAP lesions have four expressions. Type I is fraying of the superior margin of the labrum. Type II is detachment of the labral–bicipital complex. Type III is a tear of the inner rim of the superior portion of the glenoid labrum (bucket-handle tear). Type IV is a tear of the inner rim of the superior portion of the glenoid labrum (bucket-handle tear) with extension of the tear into the labral–bicipital complex. At times a labral tear can develop gradually. Risk factors for this occurrence include repetitive movements, such as occur with throwing and strong muscle contractions of the biceps muscles, such as occur with weightlifting. |
| Rotator cuff tear (Figs. 10-113 and 10-114) | Any of the rotator cuff muscle group (subscapularis, supraspinatus, infraspinatus, or teres minor) can be involved with partial (more common) or full-thickness tears. Tears may be acute, but are more often chronic, appearing in patients over the age of 40 years. The radiographic appearance of rotator cuff tears manifests as an inferior concavity and sclerosis (Sourcil or eyebrow sign) to the inferior margin of the acromion along with elevation of the humerus, the latter observed as narrowing of the acromiohumeral space. MRI is accurate in diagnosing full-thickness tears of the rotator cuff to nearly 90%. The principal finding of a rotator cuff tear is a hyperintense signal on the T2-weighted image extending through the rotator cuff with discontinuity of the tendon and communicating with the subacromial or subdeltoid space. Retraction of the musculotendinous junction of the supraspinatus muscle also can be seen along with significant fluid accumulation in the subacromial bursa. Secondary signs of injury include loss of the subdeltoid fat, atrophy of the supraspinatus muscle, and cystic changes of the humeral head principally at the site of the supraspinatus tendon insertion. Partial thickness tears can involve either the articular or bursal surface of the tendon or the substance of the tendon and are seen as high signal intensity lesions on T2-weighted images. Articular surface lesions are the most common and are associated with impingement syndrome. |
| Shoulder impingement (Fig. 10-115) | Shoulder impingement syndrome can be secondary to narrowing of the subacromial space, syndrome which includes changes in the shape and slope of the acromion process, subacromial osteophytes, and degenerative joint disease of the AC articulation. These changes create chronic effacement of the rotator cuff tendon and often are precursors to rotator cuff tears. In older patients, the combination of repetitive overhead activity along with a congenitally narrowed subacromial space is a common cause of osteophytes on the undersurface of the acromion. In younger patients, involvement in sports that require high arm velocity and overhead throwing can be an additional cause of instability. The Neer system is one of several that exist to classify the degree of impingement. Neer stage I describes edema or hemorrhage in the supraspinatus tendon, usually in young adult patients. Stage II is more advanced tendonitis and fibrosis, presenting in middle-aged patients. Stage III describes the long-term presence of degeneration leading to rupture in middle-aged and older patients. |
| Elbow | |
| Fractures | |
| Distal humerus fracture (Figs. 10-116 to 10-119) | Supracondylar fracture is the most common fracture about the elbow in children.45,75 Comminuted intracondylar fracture of a T or Y configuration is common in adults.134,168 There are three types of supracondylar fractures. Type I is nondisplaced. Type II is an angulated fracture with minimal displacement (portion of cortex retains continuity). Type III is total displacement (complete loss of cortical continuity). A small osteochondral flake fractured off the convex surface of the capitellum is termed Kocher fracture. Malunion deformity (most often cubitus varus), nerve and vessel injury, and Volkmann contracture are complications to distal humeral fractures. In children, the appearance of normal secondary ossification centers may be mistakenly interpreted as fractures; the acronym CRITOE describes the order of appearance of the secondary ossification centers about the elbow: capitellum, radial head, internal epicondyle, trochlea, olecranon, and external epicondyle. If the trochlea is seen, there also must be an internal epicondyle; otherwise what is thought to be the trochlea is probably a fracture fragment.39 |
| Little Leaguer’s elbow (Figs. 10-120 and 10-121) | Little leaguer’s elbow is an avulsion of the medial epicondyle resulting from traction forces of the flexor-pronator tendons.27,36 Injury is related to chronic muscles strain placed on immature bone and cartilage. As the name implies, it is common among young baseball players due to the action of throwing a baseball. Clinical presentations include pain and a hesitation or “catching” of the joint during its range of motion. |
| Olecranon (Fig. 10-122) | An olecranon fracture is the second most common elbow fracture, following the proximal radius.206 Fractures usually are oriented transversely112 and are easily noted in the lateral projection, usually occurring as isolated injuries. A fall on a semiflexed supinated forearm is the most common mechanism of injury, in which the triceps muscles leverage the olecranon over the fulcrum of the distal humerus. Other mechanisms of injury include hyperextension and a direct blow to the region.135 |
| Coronoid fracture (Fig. 10-123) | Fracture of the coronoid process is uncommon generally, and rare as an isolated injury. Fractures of the coronoid process usually are associated with either a posterior elbow dislocation or a radial head fracture. |
| Radial head fracture (Figs. 10-124 to 10-126) | A radial head fracture is the most common elbow fracture in the adult,206 and typically is difficult to detect on radiographs. One hint to the diagnosis of an intracapsular injury (inclusive of the radial head) is the observation of the thin fat pads (“fat pad” or “sail” sign) located between the synovial and fibrous layers of the joint capsule of the elbow. In the lateral flexed elbow position, an elbow injury with resulting joint effusion may cause elevation of the normally slightly visible anterior fat pad and visibility of the normally invisible posterior fat pad.20,134,136 A fracture oriented with the long axis of the bone is termed a chisel fracture. Radial head fractures are classified according to the degree of displacement. Type I fractures are generally small and nondisplaced. Type II fractures are larger and displaced. Type III fractures are comminuted. Displaced fragments may require surgery. |
| Dislocations | |
| Elbow dislocation (Fig. 10-127) | Elbow dislocation is the third most common dislocation in adults, following those of the shoulder and interphalanges, and is the most common dislocation in children. Overall, it is more common in children than adults.5 The direction of dislocations of both the radius and ulna usually (90%) is posterior.195 There is a high rate of concurrent fractures. On a normal lateral projection of the elbow, a line through the center of the shaft of the radius should intersect the center of the capitellum; failure to do so may indicate dislocation.236 The anterior humeral line describes a line drawn along the anterior border of the humerus in the lateral projection. Under normal circumstances the line should intersect the middle third of the capitellum.206 Anterior displacement of the line may indicate supracondylar fracture. |
| Pulled elbow (nursemaid’s elbow) | A sudden jerk or pull on a toddler’s pronated elbow may cause dislocation of the proximal radius with entrapment of the annular ligament within the joint space.213 Radiographs typically are negative. |
| Forearm | |
| Fractures | |
| Essex-Lopresti injury (Fig. 10-128) | Essex-Lopresti fracture is a comminuted fracture of the radial head with dislocation of the distal radioulnar joint.50,70,74 This complex injury usually results from a fracture–dislocation of the elbow or radial head impaction on the capitellum from longitudinal application of force associated with a fall on an outstretched hand. |
| Galeazzi (Piedmont, reversed Monteggia) (Fig. 10-129) | Galeazzi fracture is a fracture of the distal radius with dislocation of the distal radioulnar injury joint.115,167 It is associated with a fall in which an axial load is placed on the hyperpronated forearm.198,256 Sometimes the fracture is complicated by compartment syndrome. Anterior interosseous nerve (branch of the median nerve) palsy may arise, presenting with a loss in pinch strength of the thumb (flexor pollicis longus) and index finger (flexor digitorum profundus). A Galeazzi fracture usually is treated with open reduction. |
| Monteggia injury (Fig. 10-130) | Monteggia fracture involves the proximal ulna with dislocation of the radial head.7 Although dislocation may occur in any direction, anterior dislocation of the radius was first described and is most common.28 Monteggia fracture occurs in both children and adults. In adult patients, this fracture is historically notorious for its poor clinical outcome; however, modern techniques of plate–screw fixation have improved anatomic reduction and functional outcomes substantially.81,202 In children, the ulna fracture typically is incomplete and therefore more stable. |
| Nightstick (parry) fracture | A nightstick fracture occurs to the distal third65 or (less often) middle third of the ulnar shaft. Often it is secondary to raising the forearm overhead in an attempt to protect the victim’s head or face from a nightstick or club strike. |
| Both bones (BB) fracture (Fig. 10-131) | Concurrent fractures of the radius and ulna (or tibia and fibula) most often are found in the middle third of the bones and often result in marked limb angulation and rotation. |
| Wrist | |
| Fractures | |
| Chauffeur’s (backfire, Hutchinson) (Figs. 10-132 and 10-133) | A chauffeur’s fracture is an undisplaced fracture of the radial styloid. It is named for the fracture occupational hazard of experiencing a backfire while attempting to start an automobile with a hand crank.33 |
| Colles fracture (Figs. 10-134 to 10-137) | A Colles fracture results most often from a fall on an outstretched hand (FOOSH) with the forearm pronated in dorsiflexion.259 It consists of a fracture of the distal radius with posterior angulation of the distal fragment producing a “dinner fork” or “silver fork” deformity. There is an increased incidence with advanced age; it is more common among women; and 60% are accompanied by fracture of the ulnar styloid process.3 |
| Greenstick fracture (Fig. 10-138) | A greenstick fracture is an incomplete fracture occurring in a long bone of a child. The fracture occurs on the convex side of a bowing bone, demonstrating marked angulation at the site of fracture. It is common at, but not limited, to the radius. |
| Hamate fracture | A hamate fracture is common to golf,247 baseball,32 and racquet sports,231 and usually involves the hamulus, which appears sclerotic, ill defined, or absent if injured.182 |
| Rim (Barton) fracture | A Barton fracture is an intraarticular fracture of the posterior rim of the distal radius. The carpals usually deviate posteriorly with the fractured fragment, often blurring the posterior distal forearm fat pad. A reversed Barton fracture involves the anterior rim of the distal radius. |
| Scaphoid (navicular) fracture (Figs. 10-139 to 10-142) | A scaphoid fracture is the most common carpal fracture. It usually occurs in persons between 15 and 40 years of age, and is a common occult fracture.98 Seventy percent of fractures occur at the waist of the bone, 20% in the proximal pole, and 10% are in the distal pole.98 Scaphoid fractures often are subtle and overlooked on radiographs. Care must be exercised with radiographic positioning. It is helpful to distract the wrist to the ulnar side via the ulnar flexion view, which elongates the scaphoid for a better view of the bone on the posteroanterior wrist projection. Because the principal blood supply for the scaphoid enters at its waist, more proximal fractures risk avascular necrosis (up to 15%),272 or nonunion (up to 30%)206 of the proximal pole. Scaphoid fractures often are difficult to detect. The presence of carpal injury is suggested by distortion of the fat pad associated with the pronator quadratus along the ventral carpus. Ninety percent of scaphoid fractures have overlying obliteration of fat stripe.244 MRI is helpful in the detection of radiographically occult scaphoid fractures and also helps delineate the complication of osteonecrosis. MRI is the most sensitive modality for the detection of osteonecrosis and is more sensitive than radionuclide studies in the early detection of this pathology.255 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree