Trauma and Intervention
The pulmonary vessels can be injured by blunt or penetrating trauma directly, or they can be affected by trauma indirectly, as occurs with fat embolism. Pulmonary artery or vein transection and pseudoaneurysm are more common with penetrating trauma but can occur with blunt chest trauma. Peripheral interventions can affect the pulmonary vessels, most commonly with air embolism but also with catheter and cement embolism. Pulmonary vessel surgery or direct pulmonary vessel interventions can lead to in situ thrombosis, vessel stenosis, pseudoaneurysm and rupture, and occasionally fistula formation.
 Pseudoaneurysm
Pseudoaneurysm
 A pseudoaneurysm, or false aneurysm, is one in which one or more of the arterial layers (adventitia, media, and intima) are missing.
A pseudoaneurysm, or false aneurysm, is one in which one or more of the arterial layers (adventitia, media, and intima) are missing.
 These tend to be saccular in shape (Fig. 9.1).
These tend to be saccular in shape (Fig. 9.1).
 Fat Embolism
Fat Embolism
 Fat embolism is an infrequent complication of fracture in a single long bone but is relatively common after more severe trauma. Other causes include hemoglobinopathies, major burns, pancreatitis, overwhelming infection, tumors, blood transfusion, and liposuction.
Fat embolism is an infrequent complication of fracture in a single long bone but is relatively common after more severe trauma. Other causes include hemoglobinopathies, major burns, pancreatitis, overwhelming infection, tumors, blood transfusion, and liposuction.
 The production of free fatty acids initiates a toxic reaction and inflammation centered on the endothelium. Also, fat globules and aggregates of red blood cells and platelets cause mechanical obstruction of the pulmonary vasculature.
The production of free fatty acids initiates a toxic reaction and inflammation centered on the endothelium. Also, fat globules and aggregates of red blood cells and platelets cause mechanical obstruction of the pulmonary vasculature.
 The classic clinical triad of hypoxia, neurologic abnormalities, and petechial rash occur within 12 to 24 hours after the traumatic event.
The classic clinical triad of hypoxia, neurologic abnormalities, and petechial rash occur within 12 to 24 hours after the traumatic event.
 Usually, 1 to 2 days elapse between the traumatic event and the appearance of radiographic abnormalities (see
Usually, 1 to 2 days elapse between the traumatic event and the appearance of radiographic abnormalities (see
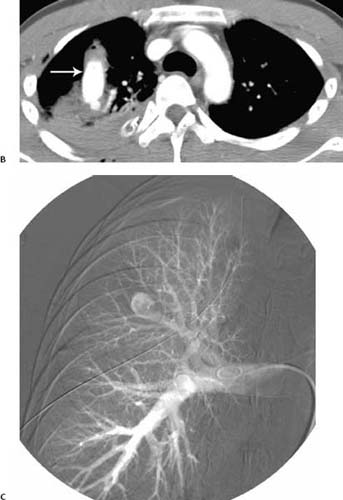
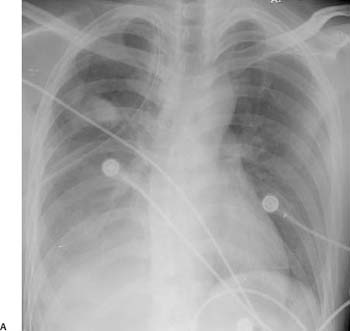
Fig. 9.1 (A–C) Pseudoaneurysm in a 23-year-old man with a stab wound. (A) Chest radiograph shows an ill-defined right upper lobe nodule, adjacent ground-glass opacification, and a moderate amount of right pleural fluid. Pseudoaneurysm in a 23-year-old man with a stab wound. (B) Contrast material–enhanced CT demonstrates a large pseudoaneurysm in the right upper lobe (arrow) and adjacent pulmonary hemorrhage. (C) Right pulmonary angiogram before coiling confirms a pseudoaneurysm arising from the right upper lobe.
Fig. 4.42 in Chapter 4); this allows differentiation from traumatic contusion.
 Air Embolism
Air Embolism
 Iatrogenic causes include injection of fluid including contrast material into venous catheters, transthoracic needle biopsy, and barotrauma resulting from positive-pressure ventilation.
Iatrogenic causes include injection of fluid including contrast material into venous catheters, transthoracic needle biopsy, and barotrauma resulting from positive-pressure ventilation.
 Air embolism occurs in up to 23% of patients given contrast material at computed tomography (CT; see Fig. 4.37 in Chapter 4).
Air embolism occurs in up to 23% of patients given contrast material at computed tomography (CT; see Fig. 4.37 in Chapter 4).
 Large volumes of air or right-to-left shunts can result in death or stroke.
Large volumes of air or right-to-left shunts can result in death or stroke.
 Catheter Embolism
Catheter Embolism
 This iatrogenic embolism is due to catheter tear, which most often occurs on catheter removal (Fig. 9.2).
This iatrogenic embolism is due to catheter tear, which most often occurs on catheter removal (Fig. 9.2).
Fig. 9.2 Catheter embolism in a 59-year-old woman. CT demonstrates catheter within anterior segment of the right upper lobe pulmonary artery (arrow).
 Cement (Polymethylmethacrylate) Embolism
Cement (Polymethylmethacrylate) Embolism
 The introduction of cement during percutaneous vertebroplasty is the most common cause of cement pulmonary embolism.
The introduction of cement during percutaneous vertebroplasty is the most common cause of cement pulmonary embolism.
 Embolism is via the external vertebral venous plexuses to the pulmonary arteries (Fig. 9.3).
Embolism is via the external vertebral venous plexuses to the pulmonary arteries (Fig. 9.3).
Fig. 9.3 Cement embolism in an 83-year-old man. CT demonstrates a subsegmental cement embolism within the left lower lobe (arrow).
 Pulmonary Artery Thrombosis
Pulmonary Artery Thrombosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree