Functions
• General somatic efferent (GSE). Somatic motor innervation of the superior oblique (SO) muscle.
Anatomy
• The trochlear nucleus is in the inferior midbrain, inferior to the oculomotor nuclear complex, dorsal to the medial longitudinal fasciculus at the level of the inferior colliculus, ventrolateral to the cerebral aqueduct (Fig. 4.1).
• Trochlear nerve fascicles course posteroinferiorly around the cerebral aqueduct to decussate in the superior medullary velum of the midbrain and exit the contralateral side of the dorsal midbrain just below the inferior colliculus (Fig. 4.2). The cisternal segment runs anteriorly under the free edge of the tentorium, traversing the quadrigeminal, ambient (perimesencephalic), crural, and pontomesencephalic cisterns (Fig. 4.3). Cranial nerve (CN) IV then passes between the posterior cerebral artery (PCA) and the superior cerebellar artery (SCA) lateral to CN III and pierces the dura of the cavernous sinus along the lateral clivus below the petroclinoid ligament. It travels in the lateral wall of the cavernous sinus below CN III and above CN V1 (Fig. 4.4) and then enters the orbit through the superior orbital fissure (SOF) above the annulus of Zinn. It then crosses medially near the roof of the orbit over the levator palpebrae superioris (LPS) and superior rectus (SR) muscles to innervate the SO muscle.
• The tendon of the SO muscle passes through the trochlea (a “pulley” of variably calcified fibrocartilage) in the medial wall of the orbit and inserts on the sclera of the posterolateral globe. Therefore, contraction of the SO causes depression of the eye when the eye is adducted and inward rotation of the eye (intorsion) when the eye is abducted (Fig. 4.5).
• The trochlear nerve has several unique features among the CNs. It is the smallest CN (only ~2400 axons), the only CN to exit from the dorsum of the brainstem, the only CN in which all axons decussate, the only CN to decussate outside the CNS, and the CN with the longest intracranial course (~7.5 cm). Note: because of the small size of CN IV, it is not visible on routine magnetic resonance imaging (MRI) sequences. It may be directly visualized with very high resolution MR imaging sequences or may be revealed in cases of nerve pathology (see below).
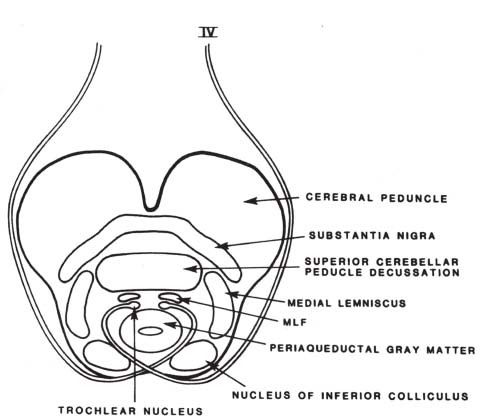
Fig. 4.1 Cross-section of midbrain at the level of the inferior colliculus demonstrating trochlear nucleus and course of CN IV (see text). (From Harnsberger HR. Handbook of Head and Neck Imaging [2nd ed.] St. Louis, MO: Mosby, 1995. Reprinted with permission.)
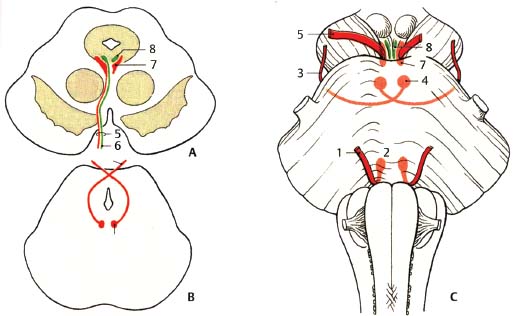
Fig. 4.2 Comparison of nuclear regions and exits of oculomotor, trochlear, and abducens nerves. (A) Midbrain at the level of the superior colliculus. (B) Midbrain at the level of the inferior colliculus. (C) Ventral view of brainstem. (1, abducens nerve; 2, abducens nucleus; 3, trochlear nerve; 4, trochlear nucleus; 5, oculomotor nerve; 6, visceromotor [parasympathetic] fibers; 7, oculomotor nucleus; 8, Edinger-Westphal nucleus.)
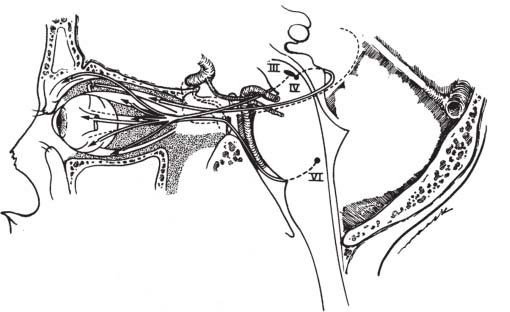
Fig. 4.3 Comparison of origins and courses of oculomotor, trochlear, and abducens nerves. The oculomotor and trochlear nerves originate in the midbrain, whereas the abducens nerve originates in the lower pons. All three nerves ultimately exit the cranial base into the eye via the superior orbital fissure (see text for details). (From Harnsberger HR. Handbook of Head and Neck Imaging [2nd ed.] St. Louis, MO: Mosby, 1995. Reprinted with permission.)
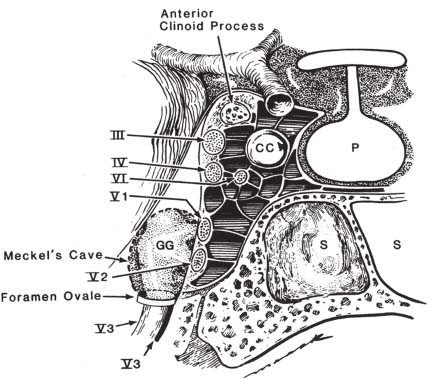
Fig. 4.4 Coronal view through the cavernous sinus demonstrates CN III, IV, VI, and V1 and V2 in the lateral wall of the cavernous sinus and CN VI within the cavernous sinus adjacent to the cavernous portion of the ICA. Note that CN V3 does not enter the cavernous sinus but rather leaves the cranial base through the foramen ovale. (From Harnsberger HR. Handbook of Head and Neck Imaging [2nd ed.] St. Louis, MO: Mosby, 1995. Reprinted with permission.)
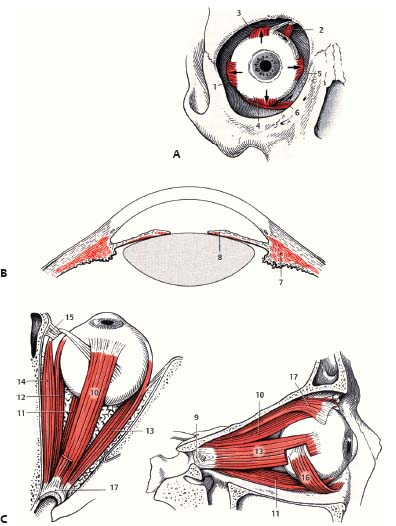
Fig. 4.5 Schematic of extraocular and intraocular muscles. (A) Anterior view. (1, LR muscle; 2, SO muscle; 3, SR muscle; 4, IR muscle; 5, MR muscle; 6, IO muscle.) (B) Intraocular muscles. (7, ciliary muscle; 8, sphincter pupillae muscle.) (C) Superior (left) and lateral (right) views. (9, common annular tendon [annulus of Zinn]; 10, SR muscle; 11, IR muscle; 12, MR muscle; 13, LR muscle; 14, SO muscle; 15, trochlea; 16, IO muscle; 17, LPS muscle.)
Trochlear Nerve Lesions
• The trochlear nerve is uncommonly affected in isolation.
• Trochlear palsy is the most common cause of vertical strabismus.
• A pure trochlear palsy is characterized by vertical or diagonal diplopia greatest on downward gaze directed to the opposite side. Excyclodeviation (outer rotation of globe) can be seen as well.
• Unilateral nuclear/fascicular lesion results in a contralateral SO palsy; lesions distal to the decussation result in an ipsilateral SO palsy.
• A patient with a unilateral SO palsy typically tilts his head to the side opposite the paretic muscle (Bielschowsky sign) to decrease diplopia, as contralateral head tilt counteracts excyclodeviation.
• Typically these patients have difficulty reading and going down stairs.
• Congenital trochlear palsies can be sporadic or familial (autosomal dominant). Longstanding head tilt observed in family photographs can aid in diagnosis.
Types
Brainstem Lesions (Nucleus or Fascicular Segment)
• Associated neurologic findings indicating dorsal mid-brain injury can include internuclear ophthalmoplegia (due to medial longitudinal fasciculus [MLF] lesion), Horner syndrome (due to lesion of descending sympathetic fibers), and afferent pupillary defect (due to lesion of pretectal fibers) (see Appendix B).
• Specific causes of nuclear/fascicular lesions:
 Trauma (trochlear nucleus may be involved by shear injury or contusion to the dorsolateral brainstem)
Trauma (trochlear nucleus may be involved by shear injury or contusion to the dorsolateral brainstem)
 Ischemia (e.g., perforator infarct)
Ischemia (e.g., perforator infarct)
 Tumor (e.g., brainstem glioma or metastasis)
Tumor (e.g., brainstem glioma or metastasis)
 Demyelinating disease (e.g., multiple sclerosis [MS]) (rare, perhaps because fascicular course of CN IV is so short)
Demyelinating disease (e.g., multiple sclerosis [MS]) (rare, perhaps because fascicular course of CN IV is so short)
 Infectious/inflammatory
Infectious/inflammatory
Lesions in the Subarachnoid Space (Cisternal Segment)
• Trauma (nerve avulsion or contusion, stretching or compression against tentorium)
• Ischemia (e.g., diabetic trochlear neuropathy)
• Increased intracranial pressure (ICP) (e.g., hydrocephalus)
• Vascular compression (e.g., SCA aneurysm in ambient cistern)
• Neoplasm (e.g., tentorial meningioma, CN IV schwannoma, perineural spread of tumor)
• Iatrogenic (injured during surgery under tentorial edge, radiation injury)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree