Tuberculosis, Miliary
Martha Huller Maier, MD
Key Fact
Terminology
Fulminant infection with Mycobacterium tuberculosis disseminated via bloodstream
Imaging Findings
Nodules small and uniform in size, usually too numerous to count
May have background of ground-glass opacities or septal thickening
Random distribution of nodules with respect to secondary pulmonary lobule
Mild basilar predominance acutely
Mild upper lung zone predominance chronically
Resolution complete with proper therapy or restoration of immune competence
Typical miliary lesions may not be visible radiographically until 3-6 weeks after hematogenous dissemination
Top Differential Diagnoses
Metastases
Disseminated Fungal Disease
Viral Pneumonia
Pathology
PPD and sputum often negative in miliary TB
Clinical Issues
Lack of respiratory symptoms common
100% mortality if untreated
Miliary TB also seen after intravesical BCG immunotherapy for transitional cell carcinoma of bladder
TERMINOLOGY
Abbreviations and Synonyms
Tuberculosis (TB), miliary TB, disseminated tuberculosis, mycobacteremia
Definitions
Fulminant infection with Mycobacterium tuberculosis disseminated via bloodstream
Typically a complication of primary infection with tubercle bacillus
Less common in post-primary tuberculosis
IMAGING FINDINGS
General Features
Best diagnostic clue
Innumerable small noncalcified nodules with random distribution
Distinct from endobronchial spread of infection, with tubercle bacillus resulting in tree-in-bud pattern of nodularity
Patient position/location
Bilateral diffuse random distribution of nodules
Mild basilar predominance acutely
Mild upper lung zone predominance chronically
Size: Nodules < 5 mm diameter
Morphology: Fine rounded nodules: May be discrete or less well defined
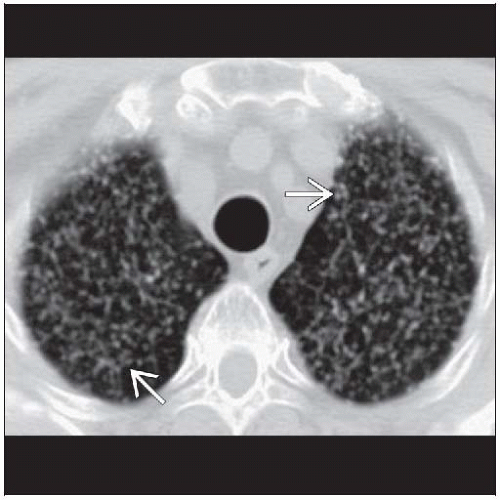
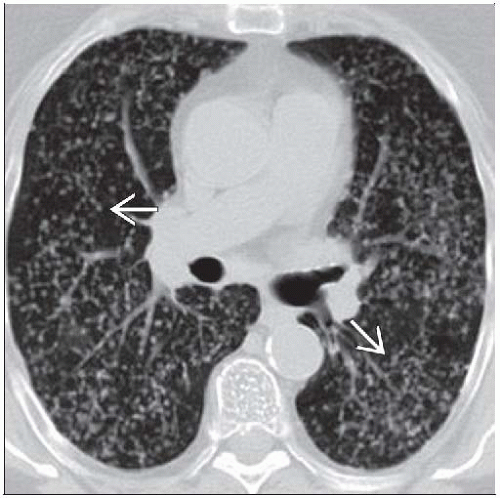
CT Findings
Morphology
Nodules small and uniform in size, usually too numerous to count
Usually sharply marginated
May have background of ground-glass opacities or septal thickening
Nodules are diffuse and bilateral
May have feeding vessel sign
Distribution
Random distribution of nodules with respect to secondary pulmonary lobule
Not clustered into rosettes like centrilobular disease
Profusion of nodules may be higher in lower lung zones acutely
Due to increased perfusion of lower lung zones
Nodules may grow faster and become larger in upper lung zones with time
Due to increased oxygen concentrations in upper lung zones
Evolution
Resolution complete with proper therapy or restoration of immune competence
Associated findings
30% of individuals with miliary disease may have other findings that suggest TB
Tuberculoma, lymphadenopathy, consolidation, effusion suggest miliary dissemination as result of primary TB
Calcified lymph nodes, cavitation, upper lobe fibrocavitary disease suggest miliary dissemination as result of post-primary TB
Radiographic Findings
Tiny nodules in miliary TB are too small (< 3 mm diameter) to be individually visualized radiographically
Summation effect: Superimposition of lesions normally too small to be seen on radiographs; nodules summate to miliary pattern
Imaging Recommendations
Best imaging tool
CT can demonstrate miliary disease before it becomes radiographically apparent
Typical miliary lesions may not be visible radiographically until 3-6 weeks after hematogenous dissemination
25-40% of affected individuals have normal chest radiographs at initial presentation
DIFFERENTIAL DIAGNOSIS
Metastases
Common metastases presenting with miliary pattern
Thyroid cancer
Melanoma
Choriocarcinoma
Renal cell carcinoma
Breast cancer
Metastatic nodules tend to be slightly larger, more well defined than those of miliary tuberculosis
Tend to vary more in size than those of miliary tuberculosis
Disseminated Fungal Disease
Histoplasmosis: Miliary nodules heal with calcification
Viral Pneumonia
Healed varicella pneumonia can present as miliary calcified nodules
Sarcoidosis and Silicosis
Miliary pattern of nodularity less common but has been described
Nodules predominantly in middle and upper lung
Pulmonary Hemosiderosis
Associated with chronic mitral valve stenosis
Nodules often calcified/ossified
Talcosis
Initial miliary pattern may coalesce to progressive massive fibrosis much like silicosis
Nodules may be calcified
Bronchioloalveolar Cell Carcinoma
Predominant nodule distribution pattern is centrilobular, reflects endobronchial spread of disease
Nodules with true random distribution are seen less often, reflect hematogenous spread
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree