Tuberculosis, Post-Primary
Helen T. Winer-Muram, MD
Key Facts
Imaging Findings
Rim-enhancing enlarged mediastinal lymph nodes
Consolidation (100%)
Lobular size and peribronchial
Cavitation (50%)
Wall thickness variable: Thick > thin, shape may be irregular
Endobronchial spread
Nodules: Centrilobular rosettes (Acinar), poorly defined, 2-10 mm in size
Tree-in-bud appearance
CT more specific (rim-enhancing lymph nodes) and more sensitive for active disease (signs of endobronchial spread)
Top Differential Diagnoses
Chronic Fungal Infection
Ankylosing Spondylitis
Progressive Massive Fibrosis (PMF)
Pathology
Acid-fast bacilli located in macrophages, obligate aerobe
Clinical Issues
Chronic nonspecific symptoms: Cough, low-grade fever, malaise, weight loss
Diagnostic Checklist
Bronchogenic carcinomas (scar carcinoma) in patients with post-primary TB are usually advanced, because findings or progression are attributed to TB
TERMINOLOGY
Abbreviations and Synonyms
Tuberculosis (TB), post-primary TB, reactivation TB, recrudescent TB
Definitions
Indolent bacterial (Mycobacterium tuberculosis) infection, often relapsing course, associated with fibrosis, calcification, and adenopathy
Varying appearance, depending on time course
Primary tuberculosis, initial infection
Miliary tuberculosis, overwhelming infection
Post-primary tuberculosis, recurrent infection
IMAGING FINDINGS
General Features
Best diagnostic clue: Rim-enhancing enlarged mediastinal lymph nodes
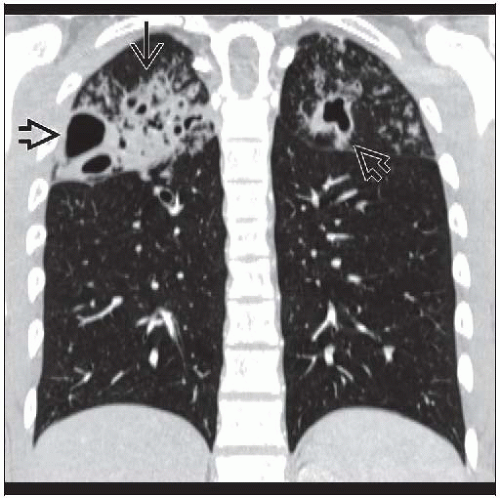
Patient position/location: Apical or posterior segments of upper lobes, superior segment of lower lobes (90%)
Morphology
Combination
Consolidation + cavitation + endobronchial spread
CT Findings
Morphology
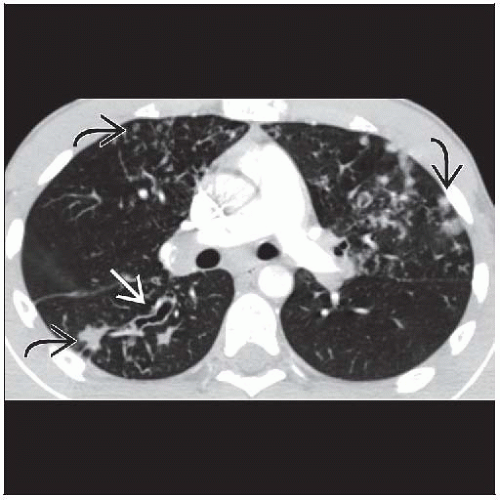
Consolidation (100%)
Lobular size and peribronchial
Cavitation (50%)
Wall thickness variable: Thick > thin, shape may be irregular
Air-fluid levels uncommon
Often surrounded by consolidated lung
Endobronchial spread
Nodules: Centrilobular rosettes (acinar), poorly defined, 2-10 mm in size
Tree-in-bud appearance
Bronchial wall thickening
Volume loss in affected lung
Usually from fibrosis (30%): Architectural distortion, bronchiectasis, emphysema
Distribution
Often segmental in distribution
Apical and posterior segments of upper lobes, superior segments of lower lobes
Bronchogenous spread: Gravity dependent lobes
Adenopathy (30%)
Classic appearance: Low-density center with peripheral rim enhancement
Mean size 3 cm in diameter
Pleural effusions (20%)
Usually small; if air, consider complicating bronchopleural fistula
Pleural thickening common in advanced cavitary disease
Evolution
With successful treatment, consolidation and nodules will resolve, usually over 9-12 months
Signs of fibrosis may increase with increasing volume loss in affected lung
Calcification in lung (Ghon lesion) and lymph nodes (Ranke complex) may be from previous primary disease
Active vs. inactive disease
Activity
Signs of endobronchial spread
Cavitation
Consolidation
Inactivity
Requires stability over 6 months
Complications
Bronchopleural fistula
Mycetomas-saprophytic aspergillus colonization in cavities
Fibrosis and retraction can cause secondary bronchial obstruction
Bronchostenosis
Broncholithiasis, erosion of calcified hilar or mediastinal lymph node into bronchus
Fibrosing mediastinitis
Empyema, may burrow into chest wall (empyema necessitatis), may involve breast (tuberculous mastitis)
May involve spine (Pott disease)
Pericardial involvement may give rise to constrictive pericarditis
Hemoptysis may be due to Rasmussen aneurysm, mycetomas, bronchiectasis, or broncholithiasis
In immunosuppressed patients, may progress to
Miliary disease: Profuse uniform distribution of 2-3 mm nodules, indicating hematogenous spread
Adult respiratory distress syndrome
Extrathoracic dissemination to breast, spine, kidney, meninges, bone
Post-primary TB in AIDS patients
Will manifest as primary TB pattern when CD4 count < 200 cell/mm3, absence of cavities, cannot form granulomas
Airspace consolidation, miliary dissemination, lymphadenopathy, effusions
No lobar predilection
Accuracy of diagnosis (90%)
Radiographic Findings
Primary: Airspace consolidation in 1 lobe; may be lobar or segmental, any lobe
If untreated, can spread to other lobes (bronchogenic spread)
Cavitation uncommon
± Adenopathy; unilateral hilar or mediastinal adenopathy may present with adenopathy alone
Effusions common, may be small or large
Miliary: Diffuse, tiny, relatively well-defined, uniform nodules, 2-3 mm in diameter
Evenly distributed but may appear more numerous and larger in upper lobes with chronic disease
Multilobar involvement, no adenopathy or effusion
Post-primary TB
Airspace consolidation, cavities, fibrosis, retraction, distortion, endobronchial spread to dependent lung, acinar nodular opacities
Apical and apical posterior segments of upper lobes and superior segments of lower lobes
Imaging Recommendations
Best imaging tool
Chest radiography for initial detection, usually sufficient for monitoring response to therapy
CT more specific (rim-enhancing lymph nodes) and more sensitive for active disease (signs of endobronchial spread)
Protocol advice
CT angiography indicated in patients with hemoptysis to identify source of bleeding
Common sources
Related to bronchiectasis, cavities with mycetomas
Pulmonary artery aneurysm from cavity (known as Rasmussen aneurysm)
Also useful to define bronchial artery anatomy for embolization
DIFFERENTIAL DIAGNOSIS
Chronic Fungal Infection
Histoplasmosis, coccidioidomycosis, sporotrichosis, resemble post-primary TB
Ankylosing Spondylitis
Associated spine changes, TB must be excluded by culture
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree