Tubo-Ovarian Abscess
Aimee Lynn Maceda
Satomi Kawamoto
Tubo-ovarian abscess (TOA) is a serious complication of pelvic inflammatory disease (PID). Rupture of a TOA may cause generalized peritonitis and/or septic shock and is an indication for immediate surgical intervention.
Mechanism.
PID occurs due to ascending infection from the cervix extending through the endometrial cavity into fallopian tubes and adnexa. The initial infection is usually caused by Chlyamydia trachomatis or Neisseria gonorrhoeae, with subsequent colonization by anaerobes, gram-negative bacteria, and streptococci. Predisposing factors include history of sexually transmitted disease or PID, multiple sexual partners, and presence of intrauterine device (IUD). TOA can be unilateral or bilateral, independent of IUD use.
Signs and Symptoms.
Presentation of TOA is nonspecific and similar to PID, including abdominal or pelvic pain (>90%), fever and leukocytosis (60-80%), vaginal discharge, vaginal bleeding, nausea, cervical motion tenderness, and palpable pelvic mass. Some patients with TOA may be asymptomatic or have mild symptoms. Absence of fever or leukocytosis does not exclude the diagnosis of TOA. Seventy percent of women with PID are younger than 25 years. A white blood cell (WBC) and β-human chorionic gonadotropin (hCG) should be obtained in all patients suspected of having TOA.
Differential Diagnosis.
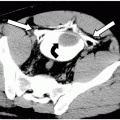
Differential diagnosis includes hydro- or pyosalpinx, ectopic pregnancy, endometriosis, ovarian neoplasm/cyst, ovarian torsion, appendicitis, and diverticulitis.
Indication.
Diagnosis of PID should be made on the basis of symptoms, clinical examination, and laboratory tests, not imaging. Imaging is indicated in patients with suspected PID who have a palpable mass, are severely ill and need inpatient therapy, are failing to respond to antibiotic therapy, or whose discomfort prevents an adequate pelvic examination. The primary goal of imaging is to differentiate between TOA and uncomplicated PID, which requires establishing the presence or absence of an inflammatory adnexal mass. Ultrasonography is the imaging test of choice for evaluation of TOA with up to 93% sensitivity and up to 98% specificity.
Protocol.
Transabdominal and endovaginal ultrasonography should be performed. Endovaginal examination has a greater sensitivity and specificity than transabdominal examination alone and must be performed unless the patient’s symptoms are unbearable.
Possible Findings in PID without TOA
Are nonspecific.
Uterus is slightly enlarged with a prominent endometrial echo. Fluid or purulent material in the uterus may be seen (endometritis).
Fallopian tube wall thickening (≥5 mm) and/or hyperemia on color Doppler suggest presence of salpingitis (Fig. 47-1).
Fallopian tube dilatation commonly occurs in chronic PID (Fig. 47-2). The dilated tube may contain clear anechoic fluid (hydrosalpinx) or echogenic debris due to pus (pyosalpinx). If the dilated tube is viewed in cross-section, thickened endosalpingeal folds may resemble the “cogwheel sign”, seen in up to 86% of patients with acute disease (Fig. 47-3).
Fluid in the pelvic cul-de-sac. Complex pelvic fluid with internal echoes, septations, and fluid-fluid levels signify fluid that may be due to infection or hemorrhage.
Pelvic pain associated with endovaginal probe motion which may be severe.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree