Tumor
The majority of primary pulmonary vascular tumors are sarcomas that most often arise in the large pulmonary arteries and less commonly the pulmonary veins. More peripherally located primary vascular neoplasms include Kaposi sarcoma, intravascular lymphoma, and epithelioid hemangioendothelioma. Secondary involvement of the pulmonary vasculature by lung metastatic deposits may mimic primary vascular tumors, and multifocal micrometastases can cause unexplained pulmonary arterial hypertension. Primary bronchogenic neoplasia may locally invade, and on occasion obliterate, pulmonary arteries and veins. This chapter also illustrates how the treatment of lung cancer can affect the pulmonary vasculature.
 Primary Sarcoma
Primary Sarcoma
 Primary sarcoma is an uncommon cause of an intraluminal filling defect in a pulmonary vessel.
Primary sarcoma is an uncommon cause of an intraluminal filling defect in a pulmonary vessel.
 Undifferentiated sarcoma and leiomyosarcoma are the most frequent histologic types that affect large pulmonary vessels, more often the arteries than the veins.
Undifferentiated sarcoma and leiomyosarcoma are the most frequent histologic types that affect large pulmonary vessels, more often the arteries than the veins.
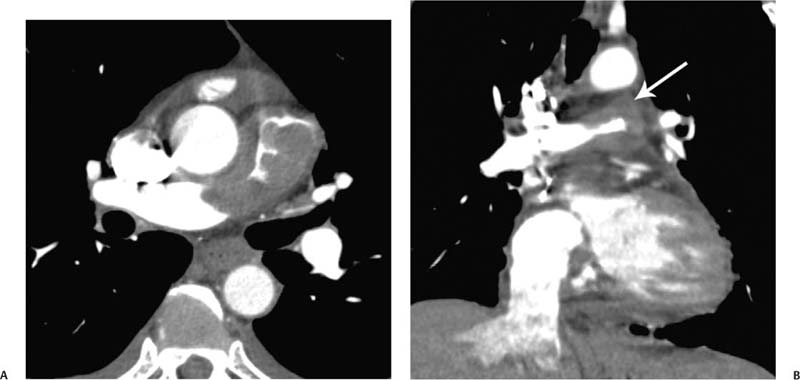
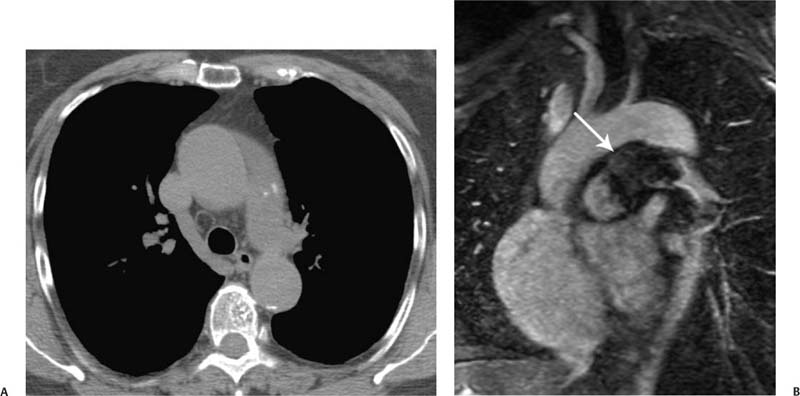
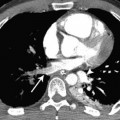
 A primary sarcoma manifests as a lobulated, heterogeneously enhancing mass on computed tomography (CT; Fig. 10.1) or magnetic resonance imaging (MRI) and can occasionally demonstrate calcifications on non–contrast-enhanced CT (Fig. 10.2).
A primary sarcoma manifests as a lobulated, heterogeneously enhancing mass on computed tomography (CT; Fig. 10.1) or magnetic resonance imaging (MRI) and can occasionally demonstrate calcifications on non–contrast-enhanced CT (Fig. 10.2).
 It often demonstrates vascular distension and local extravascular extension (Figs. 10.1 and 10.2).
It often demonstrates vascular distension and local extravascular extension (Figs. 10.1 and 10.2).
Fig. 10.1 (A,B) Pulmonary artery sarcoma in a 52-year-old man. (A) CT demonstrates a lobulated long mass extending from the main to the right pulmonary artery. (B) Coronal reconstruction CT demonstrates that the mass extends beyond the superior boundary of the pulmonary artery (arrow), indicating local invasion by a malignancy.
Fig. 10.2 (A,B) Pulmonary artery sarcoma in a 75-year-old woman. (A) Unenhanced CT demonstrates the hint of a mass and calcification within the main and left pulmonary arteries. (B) Coronal oblique contrast material–enhanced MRI demonstrates the enhancing tumor invading locally beyond the superior vessel wall (arrow).
 Kaposi Sarcoma
Kaposi Sarcoma
 Kaposi sarcoma is the most common tumor among patients with human immunodeficiency virus (HIV) infection and is associated with human herpesvirus 8 infection.
Kaposi sarcoma is the most common tumor among patients with human immunodeficiency virus (HIV) infection and is associated with human herpesvirus 8 infection.
 Despite its name, it is not a true sarcoma (which normally arises from mesenchymal tissue). Kaposi sarcoma is a cancer of the lymphatic and blood endothelium that forms vascular channels that fill with blood.
Despite its name, it is not a true sarcoma (which normally arises from mesenchymal tissue). Kaposi sarcoma is a cancer of the lymphatic and blood endothelium that forms vascular channels that fill with blood.
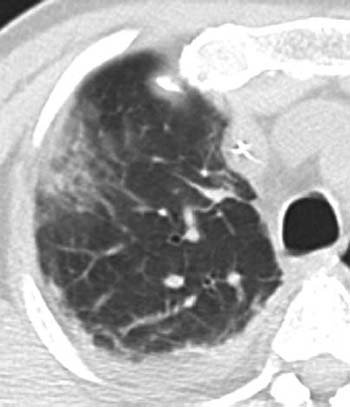
 Highly active antiretroviral therapy has resulted in a substantial diminution in the incidence, morbidity, and mortality of Kaposi sarcoma. However, the radiologic appearance has remained similar (Fig. 10.3).
Highly active antiretroviral therapy has resulted in a substantial diminution in the incidence, morbidity, and mortality of Kaposi sarcoma. However, the radiologic appearance has remained similar (Fig. 10.3).
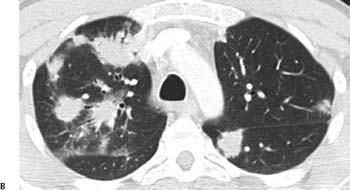
Fig. 10.3 (A,B) Kaposi sarcoma in a 40-year-old man with acquired immunodeficiency syndrome (AIDS). (A) Posteroanterior radiograph demonstrates bilateral ill-defined nodular opacities and reticular opacities, particularly of the lower lobes. Kaposi sarcoma in a 40-year-old man with acquired immunodeficiency syndrome (AIDS). (B) CT demonstrates irregular nodules and masses with a predominantly peribronchovascular distribution.
 Intravascular Lymphoma
Intravascular Lymphoma
 Intravascular lymphoma is a very uncommon non-Hodgkin lymphoma characterized by the neoplastic proliferation of lymphoid cells within the lumina of capillaries, small veins, and arteries, with little or no adjacent parenchymal involvement.
Intravascular lymphoma is a very uncommon non-Hodgkin lymphoma characterized by the neoplastic proliferation of lymphoid cells within the lumina of capillaries, small veins, and arteries, with little or no adjacent parenchymal involvement.
 The CT finding is a ground-glass opacity containing small linear and nodular opacities in the affected lung (Fig. 10.4).
The CT finding is a ground-glass opacity containing small linear and nodular opacities in the affected lung (Fig. 10.4).
Fig. 10.4 Intravascular lymphoma in a 61-year-old man. CT demonstrates a peripheral ground-glass opacity containing small linear and nodular opacities within the right upper lobe. There is also a small right pleural effusion.
 Epithelioid Hemangioendothelioma
Epithelioid Hemangioendothelioma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree