- •
Presence of monochorionic pregnancy in which one twin has a primitive, ineffective heart.
- •
Direction of flow in the umbilical artery is from placenta to fetus in the acardiac-acephalic twin (twin reverse arterial perfusion).
- •
The normal “pump” twin can develop cardiomegaly, atrioventricular valve regurgitation, and signs of heart failure due to increased work and volume load.
- •
Serial assessment of combined cardiac output in the normal “pump” twin can be helpful in monitoring for increasing burden of cardiac work.
Anatomy and Anatomical Associations
Twin reversal arterial perfusion (TRAP) sequence is a rare anomaly that occurs in 1 in 35,000 pregnancies and in 1% of monochorionic twin pregnancies. In TRAP, there is a normal twin and one that is malformed without a functioning heart, each connected to the other through a common placenta, sharing vascular connections ( Figure 39-1 ). The normal twin is called the pump twin and the affected one is the acardiac twin. The nonfunctional heart can range in spectrum from a rudimentary heart tube or markedly abnormal single ventricle that is beating to a complete lack of any cardiac structure. Because the affected twin has a nonfunctioning heart, the normal twin pumps blood through superficial arterial-arterial placental anastomoses to the affected twin. Deoxygenated blood from the affected or acardiac twin then returns to the placenta via its umbilical vein and through venous anastomoses traverses to the normal pump twin. As a result, the normal pump twin’s heart experiences an increased cardiovascular workload, which can result in heart failure, hydrops, and death.
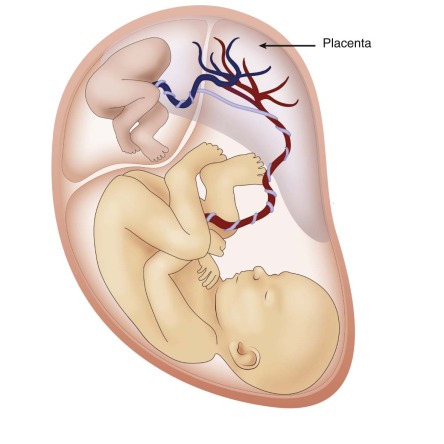
Although the pump twin is anatomically normal, a wide spectrum of anatomical pathology has been described in the acardiac twin from an amorphous mass of tissue to development of the semblance of a thorax and extremities and, occasionally, part of the cranium. There may be complete lack of cardiac structure (holocardius) to a malformed cardiac structure (hemicardius) with a heartbeat. The original classification for these developmental anomalies was based on examination of pathological specimens that lacked a cardiac structure (holocardius). Four different categories were noted: (1) acardius acephalus is the most common form seen with a well-developed pelvis and lower extremities along with no head or skull, no thoracic organs, and often no arms, (2) acardius anceps has a well-developed body and extremities but only a partially formed head and face, (3) acardius amorphous is a shapeless mass with no recognizable organs, and (4) acardius acormus, which is the rarest, has development of only the head. With the advent of ultrasound imaging, there is improvement in the understanding of the anatomical pathology of the acardiac twin. No abnormalities have been reported in the cardiac structure of the normal twin.
Frequency, Genetics, and Development
Acardiac twinning is a rare anomaly that complicates 1% of monochorionic twin pregnancies and occasionally is observed in triplet or quadruplets. It is seen in 1 in 35,000 pregnancies overall.
Because this is a rare pathology, most of the data in the literature are case reports. Although it is clear that there are abnormal flow patterns as a result of superficial placental anastomoses between the normal and the malformed twin, it is unclear whether there is a primary developmental abnormality or that abnormal flow leads to abnormal cardiac morphogenesis.
In one of the largest cohorts studied, 46/49 (94%) cases were twin gestations with 2 cases occurring in triplet pregnancies and 1 in quadruplets. In an analysis of 184 case reports of acardiac fetuses in the literature from 1960 to 1991, 92% were twins and 8% were triplets; 74% were monochorionic diamniotic with 24% monochorionic monoamniotic and 2% dichorionic diamniotic. The acardiac fetus usually has a two-vessel cord (66%) and is most likely to develop structures that are supplied by lower aortic arteries. Of 33 acardiac fetuses that had karyotyping, 11 were abnormal (33%) consisting of monosomy, trisomy, deletions, mosaics, and polyploidy, whereas 3/34 pump fetuses were abnormal (trisomy). The only associated abnormalities are rare findings of omphalocele.
Prenatal Physiology
In monochorionic pregnancies, placental vascular anastomoses normally occur between both fetuses. In pregnancies with an acardiac twin, there are abnormal superficial anastomoses both arterial and venous that allow the pump twin to supply blood for both fetuses. One of the most unique aspects of TRAP physiology is the retrograde perfusion of the acardiac twin via its umbilical artery, with hypoxic blood preferentially perfusing the caudal structures of the twin. Return of flow to the placenta is via the umbilical vein, the opposite direction of what is seen in the normal. This blood then traverses through the venous anastomoses to the pump twin. The pump twin’s heart experiences an increased workload secondary to pumping blood retrograde to the acardiac twin while also receiving additional deoxygenated blood from the placenta. As a result, the pump twin over time can develop congestive heart failure (CHF).
One report in the literature is of interest because it describes the natural progression of disease. A case of acardiac twins was followed with sequential ultrasounds from initial diagnosis at 16 weeks. The fetal echocardiogram at 30 weeks demonstrated only right and left ventricular hypertrophy. A subsequent echocardiogram 5 days later demonstrated right atrial dilation and mild tricuspid regurgitation with marked progression of these findings only a few days later leading to delivery of the fetus, suggesting the potential for rapid onset of cardiovascular deterioration. A postnatal echocardiogram, following removal of the volume load, showed resolution of the previous abnormalities.
Prenatal Management
Predictors of poor outcome in acardiac twin pregnancies include greater than 50% ratio between the acardiac/pump twin’s weights, polyhydramnios and CHF in the normal twin. Without intervention, mortality has been reported as high as 50% to 75%. Many fetal therapies have been proposed including cord occlusion. Radiofrequency ablation and laser coagulation of the acardiac twin’s umbilical cord and laser coagulation of placental anastomoses are a few techniques used.
Postnatal Physiology
In the current era, pregnancies with TRAP that are at risk for hemodynamic compromise of the pump (normal) twin have fetal intervention performed, whereas others have expectant management. In some cases, after intervention, there may be preterm delivery, which must be considered in the decision making. If the pump twin has inadequate time for cardiovascular function to improve, the neonate may present with low cardiac output requiring inotropic support. Otherwise, normal physiology for preterm or term neonates is expected.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








