Ultrasound
14.0 INTRODUCTION
The characteristics, properties, and production of ultrasound for clinical applications are described. Ultrasound interaction with tissues, instrumentation, equipment, image acquisition, processing, and display demonstrate how useful acoustic properties can be obtained, including tissue stiffness and blood velocity determinations. Common artifacts, bioeffects, and safety aspects are also considered.
14.1 CHARACTERISTICS OF SOUND
Sound is mechanical energy that propagates through a continuous medium by the compression (high pressure) and rarefaction (low pressure) of particles that comprise it. For ultrasound, the mechanical force is a transducer, composed of an expanding and contracting group of crystal elements creating local periodic compressions and rarefactions in the tissue medium. Mechanical energy travels at the speed of sound into the patient and “particles” of the tissue transfer energy much like a compressible spring, traveling as a longitudinal wave (Fig. 14-1).
1. Wavelength, Frequency, Speed
a. Wavelength (λ): distance between two repeating points in a periodic wave (i.e., a cycle), (e.g., mm).
b. Frequency (f) is the cycle repetition per second (s), in Hertz (Hz), where 1 Hz = 1 cycle/s.
(i) Less than 15 Hz is infrasound; 15 to 20 kHz is audible sound; greater than 20 kHz is ultrasound Medical ultrasound: 1 to 20 MHz, up to 50 MHz and beyond for specialized applications
c. Period: time duration of one wave (cycle) and is equal to 1/f
d. Speed of sound, c: distance traveled per unit time is equal to the product of wavelength and frequency

(i) Speed of sound units: m/s (meters/second), cm/s, mm/µs.
(ii) c varies in a medium, based on compressibility, stiffness, and density characteristics; tissues with high compressibility = slow speed (e.g., air); greater stiffness = high speed (e.g., bone) (Table 14-1).
e. Using c = 1.54 mm/µs, the wavelength in mm of soft tissue = 1.54 mm/f (MHz), thus the wavelength of a 10-MHz beam is easily calculated, as 1.54/10 = 0.154 mm and for a 2-MHz beam as 1.54/2 = 0.77 mm (Fig. 14-2).
f. Higher frequencies provide better resolution, but higher attenuation and limited depth penetration.
2. Pressure and Intensity
a. Pressure (P), expressed as Newton per square meter (N/m2) with SI unit of pascal (Pa); “pressure amplitude” refers to the magnitude of change in pressure: note—earth’s atmospheric pressure = 100,000 Pa and ultrasound imaging peak pressure is 1,000,000 Pa or 1 MPa—the peak US intensity is about 10 times higher than earth atmospheric pressure.
b. Intensity, I, is a measure of average power per unit area and is proportional to the square of the pressure amplitude, I ∝ P2; medical diagnostic ultrasound intensity levels are milliwatts/cm2.
c. Relative pressure and intensity levels are scaled using the decibel (dB), a unitless value.


TABLE 14-1 DENSITY, SPEED OF SOUND, AND ACOUSTIC IMPEDANCE FOR TISSUES AND MATERIALS RELEVANT TO MEDICAL ULTRASOUND
MATERIAL
DENSITY (kg/m3)
C (m/s)
Z (rayls)a
Air
1.2
330
3.96 × 102
Lung
300
600
1.80 × 103
Fat
924
1,450
1.34 × 106
Water
1,000
1,480
1.48 × 106
“Soft Tissue”
1,050
1,540
1.62 × 106
Kidney
1,041
1,565
1.63 × 106
Blood
1,058
1,560
1.65 × 106
Liver
1,061
1,555
1.65 × 106
Muscle
1,068
1,600
1.71 × 106
Skull bone
1,912
4,080
7.8 × 106
PZT
7,500
4,000
3.0 × 107
a Acoustic impedance is the product of density and speed of sound. The named unit, rayl, has base units of kg/(m2s) for values listed in the column. Acoustic impedance directly relates to the propagation characteristics of ultrasound in each medium and is the basis for echo formation.
(i) Pressure is proportional to voltage, so Equation 14-2 compares induced voltages of echoes.
(ii) Pressure or voltage comparisons have a factor of 2× higher values on dB scale relative to intensity.
(iii) Intensity ratio of 106 (e.g., incident pulse intensity is 106 greater than echo intensity) = 60 dB (Eq. 14-3).
(iv) Change of 10 in the relative intensity dB scale = order of magnitude (10 times) change.
(v) Change of 20 is equal to two orders of magnitude (100 times) change, and so forth.
(vi) Intensity ratio greater than 1, dB scale is positive; less than 1, dB scale is negative.
(vii) Loss of 3 dB (-3 dB) represents a 50% loss of signal intensity, the “half-value” thickness (HVT).
e. Ultrasound energy imparted to the medium depends on the pressure amplitude variations generated by the degree of transducer expansion and contraction through transmit gain.
TABLE 14-2 INTENSITY RATIO AND CORRESPONDING DECIBEL VALUES | |||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
14.2 INTERACTIONS OF ULTRASOUND WITH TISSUES
Interactions of ultrasound are chiefly based on the acoustic impedance of tissues and result in reflection, refraction, scattering, and absorption of the ultrasound energy.
1. Acoustic Impedance, Z: a measure of tissue stiffness and flexibility
a. Equal to the product of density and speed of sound: Z = ρc
(i) ρ is the density in kg/m3; c is the speed of sound in m/s.
b. Sound energy transfer efficiency from one tissue to another is dependent on differences in Z.
(i) For similar Z, a large fraction of incident intensity will be transmitted through a boundary.
(ii) For wide differences in Z, most incident intensity will be reflected at the boundary.
(iii) Most soft tissues have a similar Z, allowing ultrasound to penetrate deep into the body.
2. Reflection back to the transducer
a. A beam traveling perpendicular (normal incidence = 90°) to boundary between two tissues (Fig. 14-3A).
b. The fraction of incident intensity reflected at a boundary is the intensity reflection coefficient, RI:

Subscripts 1 and 2 represent tissues that are proximal and distal to the boundary, respectively.
c. Intensity transmission coefficient TI is equal to 1 – RI.
d. Example of reflection at fat/muscle interface, Zfat = 1.34, Zmuscle = 1.71, 1.5% of intensity is reflected:

e. With air, the reflection coefficient is 1, thus 100% of incident intensity is reflected.
f. For nonnormal incidence, the reflected angle = incident angle relative to the normal direction.
3. Refraction
a. A change in direction of the transmitted ultrasound pulse when the incident pulse is not perpendicular to the tissue boundary, and the speeds of sound in the two tissues are different (Fig. 14-3B).
4. Scattering
a. Arises from objects and interfaces within tissues with size on the order of ultrasound wavelength.
(i) Low frequencies (1 to 5 MHz) with longer λ, boundaries appear specular (mirror-like)
(ii) High frequencies (greater than 5 to 15 MHz) with shorter λ, boundaries are nonspecular (Fig. 14-4)
b. Tissue signatures arise from different organs due to internal structure and echo correlation patterns.
c. Hypoechoic and hyperechoic are terms describing characteristics of tissues in terms of the relative intensity of the backscattered signal.
5. Absorption and Attenuation
a. Attenuation is the loss of US intensity with distance traveled from scattering and absorption.
b. Expressed in decibels (dB), with an average attenuation of 0.5 dB/(cm-MHz) (See Table 14-4, textbook).
c. Ultrasound attenuation occurs exponentially with depth and more rapidly with frequency (Fig. 14-5).
d. Choice of ultrasound transducer frequency is strongly dependent on required depth of imaging.
e. Example: calculate the relative ratio (incident pulse to returning echo) of a 5 MHz US wave traveling to a depth of 4 cm with a 100% reflective boundary. Answer: 5 MHz × 0.5 dB/(cm-MHz) = 2.5 dB/cm attenuation for a total travel distance of 8 cm (to and from reflector), loss of US intensity is thus 2.5 dB/cm × 8 cm = 20 dB. The relative ratio is thus 20 dB = 10 log (Iincident/Iecho); Iincident = 100 Iecho.
14.3 ULTRASOUND TRANSDUCERS
Ultrasound is transmitted and received by a transducer array, composed of hundreds of small ceramic elements with electromechanical (piezoelectric) properties, connected to controlling electronics and contained in a handheld, plastic housing with other components essential to proper operation.
1. Piezoelectric Materials
a. Lead zirconate titanate (PZT)—synthetic material composed of aligned dipole structure (Fig. 14-6).
b. Electrodes attached to each surface of PZT thickness provide the ability to receive and produce US.
c. Small mechanical displacements by returning waves in the receive mode create voltage differences of microvolts (µV).
d. Externally applied voltage pulse (approximately 100 V) in the transmit mode reorients the PZT into crystal “thickness” contraction or expansion togenerate ultrasound energy.
e. The US pulse is created using a short-duration voltage spike in the compression mode; the PZT vibrates at a natural frequency in the thickness mode of λ/2; crystal thickness determines frequency (Fig. 14-7).
2. Resonance Frequency, Damping, Absorbing, and Matching Layers
a. Transducer arrays are composed of multiple elements, each attached with electrode wires.
b. Excitation of undamped crystals will result in a long-duration, narrow bandwidth frequency (Fig. 14-8A).
(i) “Q” factor represents the purity of produced sound: Q = f0/bandwidth.
(ii) A damping layer is required to shorten pulse width, which increases the bandwidth
(iii) US imaging requires transducers with low Q to obtain a short spatial pulse length.
c. Compression in thickness mode causes expansion in the width and height of the elements (Fig. 14-8B).
d. US is emitted in both directions upon PZT excitation, requiring the use of an adjacent absorption layer.
e. A matching layer provides the interface between the PZT and tissue to maximize transmission.
(i) Matching layer thickness is equal to ¼ λ with a speed of sound between PZT and soft tissue.
(ii) Acoustic coupling gel is also used to improve contact and eliminate air pockets.
f. The composite structure of the transducer element array and housing are shown in Figure 14-9.
3. Broad Bandwidth “Multifrequency” Transducer Operation
a. Transducer elements are manufactured with many small PZT rods backfilled with epoxy.
b. Properties of these elements provide a better acoustic impedance match with tissue and can be operated over a selectable range of frequencies due to the composite characteristics of the material.
c. Excitation pulses of specific square wave voltage pulses of 1 to 3 cycles selects the center frequency across the available bandwidths of the transducer array.
d. Broad bandwidth response of the transducer array (Fig. 14-10) permits reception of echoes at specific frequencies, useful for native tissue harmonic imaging (see Section 14.6.5).
4. Transducer Arrays
a. Linear, curvilinear, and phased array operation are most common for diagnostic ultrasound (Fig. 14-11).
b. Linear and curvilinear arrays activate a subset of elements producing a single transmit beam pulse.
(i) Subsequent receive mode is activated to listen to echoes from depth
(ii) Activation of a different subset of adjacent elements produces another beam pulse.
(iii) This continues for all of the elements across the array, which is then repeated.
c. Phased transducer arrays activate all elements in the array, and with fine and ultrafine transmit delay timing, electronic steering of the beam can be achieved, producing a sector-scan format.
d. Intracavitary transducer arrays use both linear and phased array operation for imaging.
e. Mechanical/electronic array scanners are used for real-time 3D imaging (e.g., fetal imaging, see text for details).
14.4 ULTRASOUND BEAM PROPERTIES
The transducer-generated US beam propagates as a longitudinal wave from the transducer surface into the propagation medium and exhibits two distinct beam patterns: a slightly converging beam out to a distance determined by the geometry and frequency of the transducer (the near field) and a diverging beam beyond that point (the far field). Other considerations include US beam focusing, the generation of side lobes and grating lobes, and the spatial resolution determinants in a US beam, including axial, lateral, and elevational.
1. The Near Field
a. Also known as the Fresnel zone, is adjacent to the transducer face out to the minimum beam diameter.
(i) A converging beam profile is due to interference patterns from the multiple US sources.
(ii) “Huygens principle” describes the transducer as an infinite number of point sources.
b. The near field depth increases with excitation radius, r, and inverse to US wavelength, λ: length = r2/λ.
(i) Lateral beam dimension for subarray of linear transducer is about ½ size of excitation footprint.
c. Pressure amplitude changes are complex in the near field and vary rapidly (Fig. 14-12).
2. The Far Field
a. Also known as the Fraunhofer zone, begins at end of the near field
(i) Characterized by diverging wave and monotonically decreasing pressure (Fig. 14-12)
3. Transducer array beam focusing
a. Transmit focus is achieved by applying timing delays between transducer elements.
(i) This occurs within the subgroup of elements for linear and curvilinear arrays and for all elements for phased array transducers (Fig. 14-13).
(ii) Focal zones can occur at various depths depending on the delays between element excitations.
b. Receive focus is dynamically applied to all active elements during the reception of the echoes.
(i) Proximal echoes returning from a boundary interface are more concave—timing delays from central elements are longer relative to the peripheral elements to achieve phase coherence (Fig. 14-13).
(ii) Distal echoes have a less concave echo pattern, and the variable timing circuitry adjusts accordingly.
4. Side Lobes and Grating Lobes
a. Side lobes represent US intensity created from the element width and height expansion and contraction.
(i) Energy is directed adjacent to the main beam area in the forward direction (Fig. 14-14A).
(ii) Side lobes can easily generate echoes that map into the main beam (see section on artifacts).
b. Grating lobes result from the discrete excitations in multielement arrays.
(i) US intensity is emitted at wide angles (Fig. 14-14B).
(ii) The intensity of grating lobes is substantially less than side lobes.
c. For both side lobes and grating lobes, intensity is diminished with low Q operation (see Section 14.3.2).
5. Spatial Resolution
US resolution has three separate components: Axial, Lateral, and Elevational (Slice Thickness) (Fig. 14-15). Visibility of detail in the image is determined by the volume and dimensions of the acoustic pulse.
a. Axial resolution is also known as linear, range, longitudinal, or depth resolution.
(i) The ability to distinguish closely spaced objects in the direction of the US beam.
(ii) Is equal to ½ spatial pulse length (SPL), where SPL = product of wavelength and #cycles per pulse.
(iii) Short SPL is achieved with higher damping of transducer elements, typically 2 to 3 cycles, and higher frequency of operation (shorter wavelength) (Fig. 14-16).
b. Lateral resolution is also known as azimuthal resolution.
(i) The ability to distinguish closely spaced objects perpendicular to the direction of the US beam, and in the plane of the image.
(ii) Beamwidth is the determining factor, which changes as a function of depth (Fig. 14-17).
(iii) Lateral focal zones can be established to create a narrower beam diameter at a specified depth.
(iv) Multiple focal zones can provide good resolution over a range of depths (Fig. 14-18).
(v) Drawbacks of focal zone placement are a loss of temporal resolution and possible transition band artifacts (see section on Ultrasound Artifacts).
c. Elevational resolution is also known as slice thickness resolution.
(i) Like lateral resolution, elevational is depth dependent with a focal zone (Fig. 14-19).
(ii) “1.5D” arrays can provide multiple elevational focal zones.
14.5 IMAGE DATA ACQUISITION AND PROCESSING
Images are acquired using a pulse-echo mode of ultrasound production and detection. Each pulse is directionally transmitted into the patient. Partial reflections from tissue boundaries at normal incidence create echoes that return to the transducer as a function of travel time and depth, along a corresponding line in the ultrasound image. The receiver detects the echoes, and the process is repeated incrementally across the field of view to sequentially construct the image line by line. Data acquisition and image formation using the pulse-echo approach requires several hardware components: the beamformer, pulser, receiver, amplifier, scan converter/image memory, and display system (Fig. 14-20).
1. Beamformer: generates electronic delays for transmit/receive focusing and beam steering
a. Computer logic controls pulser, transmit/receive switch, preamps, analog to digital amplifiers
2. Pulser (Transmitter)
a. Provides voltage for exiting transducer elements; controls output transmit power
3. Transmit/Receive Switch
a. Isolates high-voltage associated with excitation (150 V) to voltage associated with echoes (approximately µV)
b. “Ring-down” time—the time required for the transducer array to switch from excitation to reception
4. Pulse-Echo Operation
a. Ultrasound intermittently transmits over a short period (approximately 1 µs) and then receives echoes (approximately 1,000 µs).
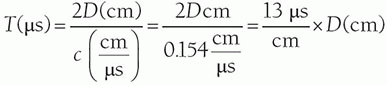
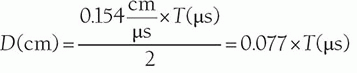
b. Depth (D) of a received echo is determined by US speed and distance traveled = 2 × depth. Pertinent equations: (uses units of µs, cm, and speed of sound in cm/µs).
c. Number of pulses/s: pulse repetition frequency (PRF)
d. Time between pulses: pulse repetition period (PRP) (Fig. 14-21)
e. Pulse duration: ratio of the #cycles/pulse to the transducer frequency = “on” time—1 to 2 µs
f. Duty cycle: fraction of “on” time = pulse duration/PRP = approximately 0.2% to 0.4%
5. Preamplification and Analog-to-Digital Conversion
a. Returning signals are preamplified prior to analog to digital conversion during swept gain step.
b. Range of voltage amplitude changes can be as much as 120 dB (a factor of 106 for pressure amplitude).
6. Beam Steering, Dynamic Focusing, and Signal Summation (Fig. 14-22)
a. It is essential to orchestrate the acquisition to achieve a high SNR echo train during the PRP.
b. A combination of preamplification and dynamic focusing produces a stream of reliable acoustic data.
7. Receiver accepts data from the beamformer during the PRP, with subsequent signal processing (Fig. 14-23): preamplification, time gain compensation, logarithmic compression, demodulation, and noise rejection
a. Time gain compensation (Fig. 14-24) is a user-adjustable amplification of returning echoes versus time
(i) Ideal TGC curve makes all equally reflective boundaries at various depths have the same amplitude.
(ii) User adjustment is typical with multiple slider potentiometers or electronic calipers.
b. Dynamic range/logarithmic compression reduces the echo amplitude range for the video display.
c. Demodulation and envelope detection converts the detected signals into a positive, smooth pulse.
d. Noise rejection sets the lower threshold signal level allowed to pass the scan converter.
e. Processed signals are passed to the scan converter for gray scale image display.
8. Echo Signal Modes
a. A-mode (amplitude) is the processed signal versus time as shown in Figure 14-23(5), where 1 A-line of data is produced per pulse for conventional line-by-line acquisition.
b. B-mode (brightness) is the conversion of the A-mode amplitude into a B-mode gray scale values.
c. M-mode (motion) is a technique using B-mode signals, a stationary beam, and deflecting the B-mode data as a function of time to evaluate anatomic motion; also known as T-M mode.
9. Scan Converter
a. Generates 2D ultrasound images from B-mode data based on trajectory and time (depth), see Figure 14-20.
b. Data interpolation is used to fill in empty or partially filled pixels in the matrix.
14.6 IMAGE ACQUISITION
The 2D ultrasound image is acquired by sweeping a pulsed ultrasound beam sequentially in a plane over the volume of interest to produce “video clips.” The matrix size and frame rate are dependent on several factors including ultrasound frequency, pulse repetition frequency, the field of view, depth of penetration, number of lines per frame, and line density. Improvements in image acquisition rate are achievable with advanced techniques such as multiline acquisition (MLA), multiline transmission (MLT), plane, and diverging wave imaging. These advances provide frame rates that go well beyond conventional line-by-line acquisitions and create high temporal resolution imaging of several hundred to thousands of frames per second.
1. Real-Time Imaging: frame rate, FOV, depth, sampling tradeoffs (Fig. 14-25)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree