Fig. 24.1
Large inferior adenoma

Fig. 24.2
Trans-upper PA
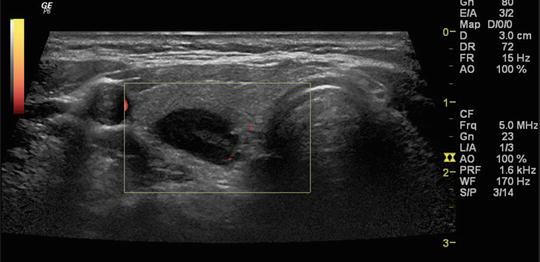
Fig. 24.3
Intrathyroidal adenoma . Note lack of echogenic line
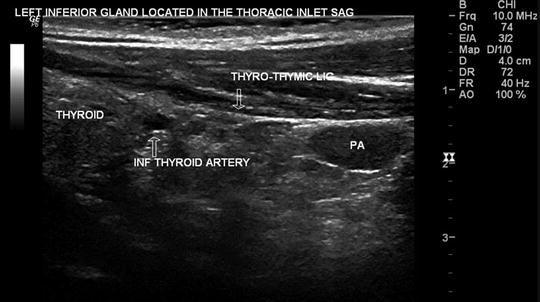
Fig. 24.4
Mediastinal thymic lesion SAG

Fig. 24.5
Inferior PA sagittal view

Fig. 24.6
Cystic adenoma FNA

Fig. 24.7
Upper PA atypical location

Fig. 24.8
Caudal displacement of superior adenoma
Parathyroid carcinomas differ in their clinical presentation compared to parathyroid adenomas, rather than by consistent US image findings. Parathyroid carcinoma should be suspected in patients who present with sudden and considerable calcium and PTH elevation. Parathyroid carcinomas can also be palpable. Even very large benign adenomas are not palpable due to their soft consistency. Parathyroid carcinomas or atypical adenomas are usually large, with our without calcific or cystic change (Fig. 24.7). Additionally, irregular margins and lack of distinct planes between the thyroid and an enlarged parathyroid gland should prompt consideration of parathyroid carcinoma .
24.7 Fine Needle Aspiration (FNA) of Parathyroid Glands or Adenomas
FNA can be performed in clinically benign appearing parathyroid tumors for confirmation prior to surgery or percutaneous ethanol injection [20, 21]. Needle tracking of malignant tumor following FNA can occur. Therefore, FNA is best avoided in suspected cases of atypical adenomas or parathyroid carcinomas. It is also best avoided at all during the initial evaluation of primary parathyroid disease. One helpful application of parathyroid FNA is to confirm a suspected lesion as parathyroid tissue in preparation for reoperative parathyroid surgery, especially when other imaging remains ambiguous or the clinical scenario is unusual.
24.8 Procedure of Parathyroid FNA
Parathyroid FNA is performed in the standard manner as one would for FNA of thyroid nodules with few differences. The use of smaller gauge needles causes less trauma and fibrosis of parathyroid adenomas and does not make subsequent surgical removal difficult [22, 23]. Parathyroid FNA can be performed using 25 or 27 G needles with or without local anesthesia. Jabbing technique is best avoided, particularly of smaller lesions to avoid multiple anterior or posterior capsular punctures. Rotation technique with aspiration is sufficient in most occasions. Blood and aspirate materials can be allowed into the hub of the needle. Parathyroid lesions yield a “bloody tap,” whereas a “dry-tap” is often encountered in the inadvertent sampling of a central compartment lymph-node .
24.9 A Protocol for Specimen Processing, Handling, and Smear Preparation of Parathyroid FNA (See Fig. 24.9)

Fig. 24.9
Specimen processing flow chart
Following completion of the biopsy of the suspected abnormal parathyroid gland, one or two direct smears are made with the material. The reminder of the specimen is washed from the syringe with 2 cm3 of saline and spun in a red top tube (contains no EDTA) for 5 min. The clear or often blood tinged supernatant is separated and submitted for PTH measurement. The specimen should be kept cold or ideally frozen prior to transportation to the laboratory. The cell pellet is saved and refrigerated as a duplicate specimen. In the unfortunate event of lost or mishandled specimen, the pellet can be resuspended in 2 cm3 of saline and re-spun to yield a second specimen. This technique can avoid unnecessary second FNA on patients. The slides are saved until the PTH FNA washout results are available. If the levels are low, then the slides along with the saved cell pellet should be submitted for cytological analysis. If the PTH FNA washout levels are elevated, then there is no need to submit the smears for cytological analysis. If the PTH levels are low, cytological analysis of the specimen should be performed. This protocol ensures that an inadvertent metastatic neck lymph node is not misdiagnosed during the evaluation of a suspected parathyroid adenoma. It is best to contact the clinical laboratory in each hospital to determine the preferred specimen processing for the red top tube; the details above are included here for the reader’s awareness of relevant issues. The syringe washout PTH levels are typically elevated in the several thousand pg/ml range. The lowest PTH that was observed in one study is 40 pg ml [21]. Parathyroid cytology is of limited value in the diagnosis and can often mimic and be misinterpreted by pathologists as a thyroid “follicular neoplasm ,” especially if the parathyroid tissue source of origin is not communicated to the lab. Thyroid follicular cells and colloid, furthermore, are often encountered on the specimen , due to the inadvertent sampling of thyroid tissue during FNA of superior adenomas [24].
24.10 Indications and Procedure of ETOH Ablation
Surgery is the mainstay for the definitive treatment of PHPT. In an occasional patient, who is deemed to have high surgical risk, percutaneous ethanol ablation may be an alternative option. The indications and contraindications to alcohol ablation are listed in Table 24.1. The procedure is performed in the following manner. The skin and subcutaneous tissue is anesthetized using 2 cm3 of lidocaine under guidance. Lidocaine infiltration is performed under vision, using US transducer along the facial planes anterior to the parathyroid lesion. Once lidocaine infiltration is complete, the lesion is entered with a 27 or 25 g needle that is loaded with 0.5–1 cm3 of alcohol. The alcohol is injected into the target lesion in question (Video 24.2). Great care should be taken to avoid injection outside the parathyroid lesion. This can result in tissue necrosis. Similarly, puncturing of the posterior or medial aspect of the capsule should be avoided altogether. The risk for injury to recurrent laryngeal nerve is greater in such situations. Patients sometimes complain of a twinge or dull ache for 5–10 min. The disappearance of blood flow by Doppler predicts success of injection. If blood flow into the gland is unaffected by the injection 5–10 min following the first injection, a second injection may be administered. Ethanol ablation can be effective in multiple endocrine neoplasia patients who have recurrent primary hyperparathyroidism [25].
Table 24.1




Indications and contraindications of parathyroid FNA
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree