27 Ultrasound Assessment of the Abdominal Aorta
Normal Sizes
The abdominal aorta gradually tapers as it courses through the abdomen. The average diameter of the aorta is smaller in women than in men. Normal values vary with age, progressively increasing from childhood into adulthood. By adulthood, the average diameter of the abdominal aorta is approximately 27 mm at the diaphragm, tapering to approximately 21 mm at the iliac bifurcation.1 For women, diameters are smaller by approximately 3 to 5 mm.
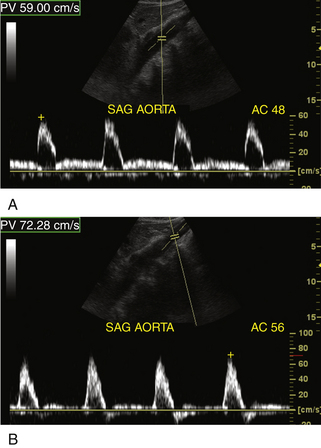
Normal Doppler Velocity Profiles
Peak systolic velocities in the abdominal aorta average 110 cm/sec in the population with an average age of 12 years.2 With aging, the average velocity decreases, ranging from 70 to 100 cm/sec. Proximally, the waveforms are triphasic but with noticeable forward blood flow during diastole (Figure 27-1, A). This diastolic component is a reflection of the low impedance of vascular beds located slightly lower in the abdominal aorta: the liver, the spleen, and the kidneys. These organs have low-resistance blood flow patterns, in essence monophasic. Below the renal arteries, the aortic Doppler tracings will show a typical “peripheral” waveform (Figure 27-1, B) with a relative decrease in forward diastolic blood flow and more prominent flow reversal in early diastole. In summary, the aortic blood flow profiles are triphasic3 and the diastolic component decreases with distance from the diaphragm. Blood flow patterns through the abdominal aorta will therefore be affected, to a certain extent, by the state of the renal arteries and of the celiac axis. There have not been any systematic studies of the variations of adult abdominal Doppler tracings linked to pathologic changes in these organs. For example, no specific studies have looked at the Doppler aortic waveforms in the presence of chronic renal failure.
Pathologic States
Atherosclerosis and Occlusive Arterial Disease
The atherosclerotic process affects the aortic wall relatively early in life and is prevalent by the late 50s in men (Figure 27-2) and later, by approximately 10 years, in women. Most autopsy studies of the distribution of arterial disease show that the abdominal aorta is one of the first affected vessels with the thoracic aorta possibly showing some of the earliest changes.4,5 Isolated high-grade stenoses and full occlusions of the abdominal aorta are uncommon in the spectrum of peripheral arterial disease.6,7 Isolated aortic lesions that become symptomatic can be seen in younger patients (less than 55 years) and more often in women. Clinically, the development of high-grade lesions tends to be slow and progressive with the concurrent development of collateral blood flow channels. Acute aortic occlusions can occur very rapidly and compromise blood supply to the lower extremities and even the mesenteric and renal arteries. More commonly, progressive aortic occlusive narrowing is accompanied by slowly increasing lower extremity symptoms. Symptoms can be very restrictive, and the patients adapt by decreasing the distances and frequency over which they walk, progressing to rest pain and then impotence in men; the syndrome is referred to as Leriche’s syndrome. Full occlusions of the abdominal aorta tend to occur in the lower portion of the aorta with thrombus spreading upward (cephalad). Normally the occlusive process and the associated thrombus formation will extend to the level of the renal arteries. The renal arteries tend to stay patent and rarely occlude. The superior mesenteric artery is rarely affected and serves as a source of collateral blood flow to the lower extremities via colonic collaterals to the inferior mesenteric artery branches and then into the internal iliac arteries.
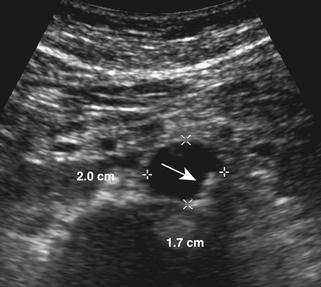
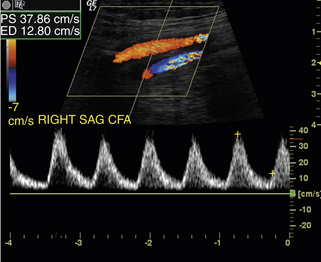
Doppler imaging at the level of the common femoral arteries can suggest the diagnosis of either occlusion or severe stenosis of the abdominal aorta (Figure 27-3). This indirect approach will of course fail to fully document the extent of aortic involvement. Doppler tracings will typically show a monophasic pattern common to any severe proximal arterial occlusion with peak velocities of 45 cm/sec or less.8–10 With acute occlusions, the relative magnitude of the diastolic velocities compared to the systolic velocities may not be as well developed. The monophasic waveform and the extent of diastolic flow reflect the ability of the peripheral circulation to recruit collateral blood flow and to vasodilate.
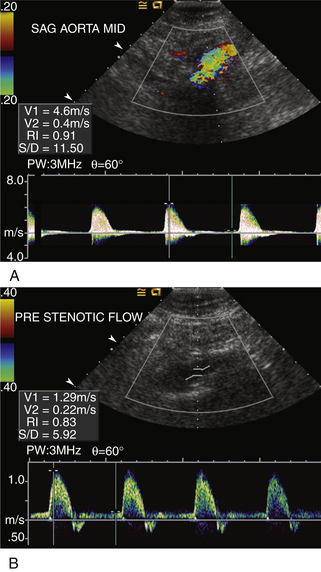
Doppler ultrasound can be used to confirm the diagnosis of an aortic occlusion by verifying the absence of blood flow in the involved aortic segment. No large series has evaluated the accuracy of this approach. Grading of stenosis severity in the aorta by Doppler criteria has also not been extensively studied because of the rarity of isolated aortic stenoses and occlusions. Implicitly, the diagnostic criteria used to grade stenosis severity are adapted from the criteria used for the lower extremity arteries, and a peak systolic velocity ratio is used (Figure 27-4). As discussed in Chapter 17, the Doppler peak systolic velocity ratio is determined by performing a Doppler velocity measurement at the site of maximal blood flow velocity and then dividing this peak systolic velocity by a “ normal” aortic peak systolic velocity. This “normal” value is measured in a contiguous segment of the aorta located above the site of stenosis. In cases of diffuse disease or absence of a good acoustic window, distal peak systolic velocities can be used to calculate this ratio when “disturbed flow” seen distal to a stenosis becomes normal again. As in the lower extremity, a velocity ratio of 2 or greater is used to indicate the presence of a 50% or greater diameter stenosis.11
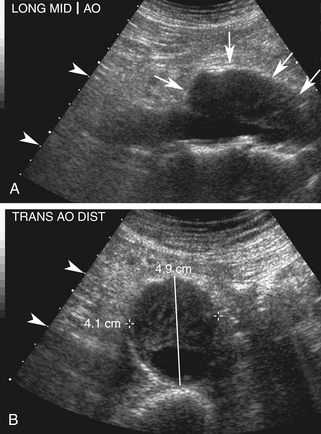
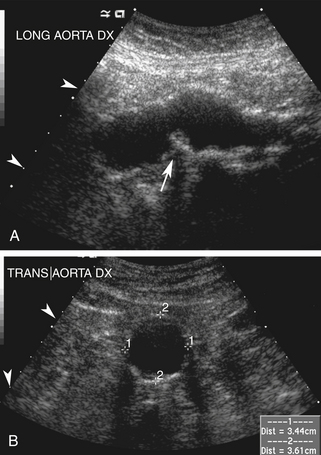
Abdominal Aortic Aneurysm
Types of Aneurysms
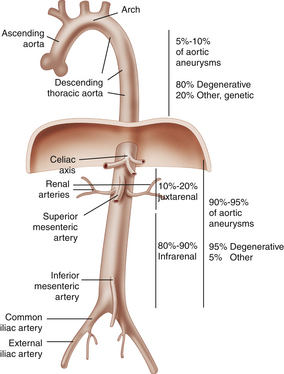
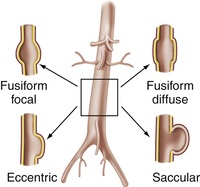
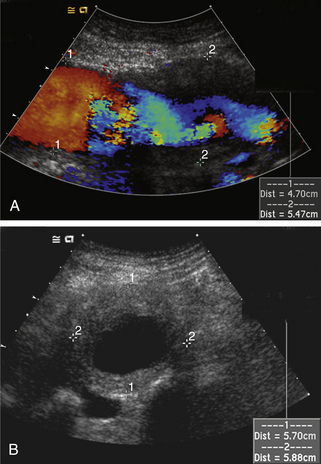
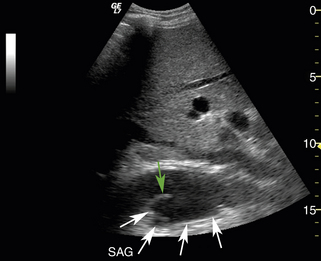
A general overview of aneurysm disease is shown in Figure 27-5. A summary of the different types of abdominal aortic aneurysms is shown in Figure 27-6. It is generally accepted that there are two types of aneurysms: fusiform (Figure 27-7; see Videos 27-1 and 27-2) and saccular (Figure 27-8). By far, the most common form of aneurysm is the fusiform type. Fusiform describes a concentric enlargement of the aorta but also includes cases where there can be extensive eccentric enlargement. By definition, all three layers of the abdominal aorta are intact in a fusiform aneurysm. Saccular aneurysms are, by their nature, eccentric because the artery wall has a dissection, and they are much less common than fusiform aneurysms, making up less than 1% of all aortic aneurysms. This number is a bit misleading because most saccular aneurysms occur in the thoracic aorta and are very rare in the abdominal aorta.
There are various possible etiologies for aneurysm formation: traumatic, infectious, vasculitides, and those associated with spontaneous dissections into the aortic wall. Although traumatic pseudoaneurysms typically rupture through all three layers of the aortic wall, they can sometimes lead to saccular aneurysms. By far, the most common location is the thoracic aorta.12 Prior instrumentation, such as placement of cannulas in the aortic wall, can be the source of saccular aneurysm formation. A second type of saccular aneurysm has typically been termed a mycotic aneurysm. Mycotic aneurysms develop because of an acute infection in the layers of the aortic wall, typically by bacteria such as nontyphoid Salmonella species, Streptococcus pneumoniae, and Staphylococcus species, although any organism can potentially be a source. Interestingly, the term mycotic implies that a fungal source would be the cause of the infection, though this is uncommon. Candida is the most common fungal organism seen in mycotic aneurysms. The distinction between saccular and mycotic aneurysm can only be made by means of cultures for the suspected organisms and the patient’s clinical presentation. The third type of saccular aneurysm is associated with a vasculitis. The inflammatory process affects the vasa vasorum of the adventitia, then spreads to cause fibrosis and degeneration of the media. The aortic wall ruptures into the media, causing a saccular aneurysm. This is typical of Behçet’s syndrome. The fourth type of saccular aneurysm occurs when a penetrating ulcer ruptures into the media of the aorta.13 This leads to a contained leak into the wall with eccentric pressure effects that promote the formation of the aneurysm. The saccular aneurysm is therefore associated with a compromise of the aortic wall. The major difference with a pseudoaneurysm is the fact that the adventitia and very commonly a part of the media remain intact in a saccular aneurysm. All three layers are ruptured in the case of a pseudoaneurysm.
Confusion can arise when a very eccentric fusiform aneurysm is imaged (Figure 27-9). The eccentricity does not represent a saccular aneurysm because all three layers of the abdominal aorta are intact. The edges of the eccentric aneurysm appear smooth, whereas a defect is seen in the aortic wall at the beginning of a saccular aneurysm.
Aneurysm Formation
The magic number for abdominal aortic intervention is 5.5 cm. The use of diagnostic ultrasound is based on detecting aneurysms below this threshold because the most serious complication of abdominal aortic aneurysm is rupture into the retroperitoneum. Although patients can present with symptoms (Table 27-1), the use of ultrasound has significantly increased the detection of smaller asymptomatic aneurysms. Rupture of an abdominal aortic aneurysm is a catastrophic event with low survival rates. The risk for rupture increases so rapidly for diameters above 5.5 cm that surgical or endovascular intervention is recommended in almost all instances once the diameter reaches 5.5 cm.
TABLE 27-1 Complications of Abdominal Aortic Aneurysms
| Complication | Mechanism | Comment |
|---|---|---|
| Rupture | Increases as size increases | Lags by 10 years in women |
| Pain (back pain or lower abdominal) | More likely in adults 50 years or less | Possibly due to inflammatory component |
| Hydronephrosis | Compression of the ureters | Large aneurysms |
| Distal embolization | Associated with mural thrombus | Uncommon |
| Acute thrombosis | Associated with atherosclerosis | Rare |
The pathologic processes that lead to the formation of abdominal aortic aneurysm are not fully understood. It is clear that elevated blood pressure, cigarette smoking, and a genetic predisposition are the major factors contributing to aneurysm formation. Aneurysms are also much more common in men than in women, with a ratio estimated from 4 to 13:1.14
The common belief that aneurysm formation is an atherosclerotic process needs to be placed in context (Figure 27-10). Elevated blood pressure and cigarette smoking are risk factors that are causally linked to the development of atherosclerosis. In the aorta, these risk factors will promote the formation of early atherosclerotic plaque and continue to promote growth and remodeling of these lesions. Continued exposure to cigarette smoke and elevated blood pressure can act directly on the constituents of the aortic wall and degrade the elastin in the artery wall. For example, cigarette smoke is associated with increased activity of elastase. Elastase will enzymatically break down the elastin in the aortic wall and compromise the mechanical integrity of the wall. Elevated blood pressure, especially pulse pressure, will cause repetitive mechanical stress on the wall of the aorta. This repeated stress leads to mechanical fatigue of the elastin, as well as the other elements of the wall, and ultimately to fragmentation and local mechanical disruption of fibers within the wall. In addition, the proportion of collagen in the aortic wall increases (types I and III). This process, occurring over time, weakens the wall of the aorta and leads to aneurysm formation.
Ultrasound Examination
Preparation
The most common reason for a failed examination of the abdominal aorta is the presence of bowel gas. Fasting after midnight and abstinence from actions that lead to air swallowing, such as smoking or chewing gum, are recommended. In some instances, a bowel preparation can be used to guarantee a better-quality examination.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree