11 Ultrasound Assessment of the Vertebral Arteries
The relationship between carotid atherosclerotic disease and lateralizing symptoms of cerebrovascular ischemia, such as transient ischemic attacks, amaurosis fugax, and stroke, is well established, and carotid endarterectomy has been shown to be effective in the management of selected groups of these patients. However, no consistently successful diagnostic and management techniques are available for those patients who present with a more confusing clinical picture of nonlocalizing symptoms of transient cerebral ischemia, such as blurred vision, ataxia, vertigo, syncope, or generalized extremity weakness. It can be difficult to determine whether the symptoms arise from carotid artery thromboembolic disease, generalized ischemia resulting from carotid or vertebrobasilar artery occlusive disease (or both), or some factor not directly related to the cerebral vasculature, such as cardiac disease.1–5 Symptomatology of posterior circulation ischemia is typically multiple and varied, and the potential contribution of vertebrobasilar insufficiency may be difficult to evaluate (Box 11-1). Although treatment of vertebral artery disease can be a successful and relatively safe procedure, the selection of appropriate patients for such reconstruction can be confounded by the previously mentioned diagnostic uncertainties, as well as by the fact that symptoms of posterior circulation ischemia frequently improve following carotid artery endarterectomy or reconstruction.6,7
BOX 11-1 Symptoms and Signs of Posterior Circulation Ischemia
Angiography, performed on the basis of the patient’s clinical history data, historically has been the definitive diagnostic procedure to identify significant vertebrobasilar obstructive lesions.8,9 The use of duplex ultrasound as a primary diagnostic technique for the diagnosis of vertebrobasilar insufficiency has been limited. Routine evaluation of the vertebral arteries is an accreditation requirement for extracranial cerebrovascular examinations by the Intersocietal Commission for the Accreditation of Vascular Laboratories,* as well as other accrediting organizations, but this assessment typically is limited to the presence or absence of flow and flow direction. Standard textbooks have limited reference to the vertebral arteries; for example, in Strandness’s textbook10 on vascular disorders, only two paragraphs of the entire chapter on extracranial arterial disease deal with the vertebral arteries, and then only to discuss qualitative waveform evaluation.
Duplex ultrasound has been shown to be an effective noninvasive technique for the evaluation of the extracranial segments of the vertebral arteries.11–13 Adequate imaging and quantitative spectral Doppler velocity data can be obtained from a portion of the midsegment of the extracranial vertebral arteries in more than 98% of patients and vessels.14,15 It is possible to collect imaging and spectral Doppler velocity data from the origin of the right vertebral artery in more than 80% of patients and from the origin of the left vertebral artery in approximately two-thirds of patients. The sections below describe appropriate duplex ultrasound evaluation techniques, the qualitative and quantitative data that can be obtained, and the interpretation and possible clinical significance of these results.
Examination Techniques
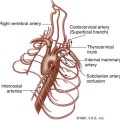
Because most hemodynamically significant lesions of the vertebral arteries occur at their origin (Region V1, defined as the segment from the origin of the vertebral artery to its entrance into the foramen of the transverse process, which occurs at the level of the sixth cervical vertebra in approximately 90% of cases), it would seem that this would be the logical site to begin the duplex ultrasound examination. Anatomically, however, this approach can be technically difficult (if not technically impossible) in as many as one-third of patients, because visualization of the origin of the vertebral artery may be obstructed by the clavicle, which interferes with the necessary probe position. Occasionally (in 3%–5% of cases) the left vertebral artery originates directly from the aorta. In addition, as the first major branch of the subclavian artery, the vertebral artery origin may be markedly tortuous, making proper angle correction for velocity measurements very difficult. Finally, the origin and proximal segment of the vertebral artery may be confused with other large branches arising from the proximal subclavian artery, such as the thyrocervical trunk.
A more reliable approach to assessment of the vertebral arteries is to initially evaluate the vessel near its midsegment, or Region V2 (the segment of the vertebral artery that courses cranially through the foramina to the transverse process of the axis). (Figure 11-1) This segment of vessel is typically quite straight, with minimal tortuosity; does not have any significant taper or diameter changes; has no immediately adjacent blood vessels, except the vertebral vein; and has no significant branching segments that would make flow velocity measurements unreliable. In addition, Region V2 of the vertebral arteries is only rarely involved with atherosclerotic obstructive disease. Further distally, the vertebral artery may be interrogated using a suboccipital approach and transcranial Doppler techniques, but Region V3 (the segment that extends from the artery’s exit at the axis to its entrance into the spinal canal) and Region V4 (extending from the point of perforation of the dura to the origin of the basilar artery) are generally inaccessible to duplex ultrasound during an extracranial cerebrovascular examination.
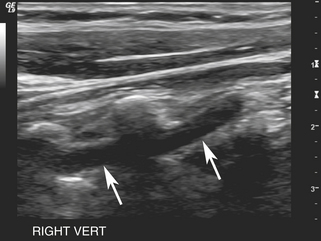
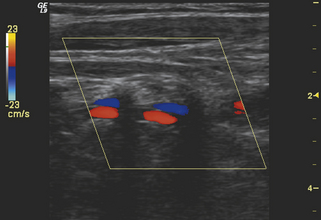
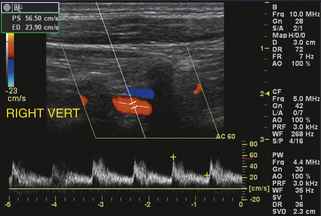
Imaging of Region V2 is most easily accomplished by first obtaining a good longitudinal view of the mid–common carotid artery at the approximate level of the third through fifth cervical vertebrae. Once this image has been obtained, a slight lateral rocking motion of the probe will bring the vertebral artery into view (see Video 11-1). The vertebral artery is readily identified by the prominent anatomic landmarks of the transverse processes of the cervical spine, which appear as bright echogenic lines in the image, beyond which deeper-lying tissues are obscured by acoustic shadowing (Figure 11-2). Between these anechoic, rectangular-shaped regions of acoustic shadowing lies an anechoic band representing the vertebral artery, as seen with gray-scale sonography. Color flow Doppler imaging helps to identify the vertebral artery by the pulsatile pattern of color flow within the anechoic band. The color flow image also distinguishes the vertebral artery from the adjacent vertebral vein (Figure 11-3), but typically the gray-scale image, with its anatomic landmarks, is sufficient for identifying the vertebral artery. Once an image of the artery has been obtained, the spectral Doppler sample volume can be placed in midvessel (Figure 11-4) to obtain qualitative and quantitative data for the evaluation of local hemodynamics. If these data appear abnormal, the vertebral artery can be followed back toward its origin as far as possible (Figure 11-5), using combined gray-scale and color Doppler imaging, to assess flow hemodynamics in the proximal segment of the artery.
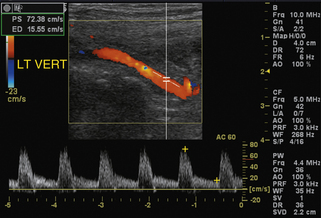
FIGURE 11-5 Color and spectral Doppler image at the origin of a normal vertebral artery. The overall waveform has a sharp systolic upstroke and is characteristic of low-resistance flow; note that peak systole is mildly exaggerated relative to end diastole (compare to Figure 11-4) secondary to the local hemodynamic effects at a site of vessel branching.
Vertebral Artery Hemodynamics: Qualitative Assessment
Normal Findings
Qualitatively, the spectral Doppler velocity waveform in the vertebral artery should appear as a scaled-down version of the normal flow signal in the internal carotid artery, since both directly supply the low-resistance intracranial vascular system. The waveform should have a well-defined systolic peak with sustained flow throughout diastole, as seen in Figure 11-4. There is wide variability in the absolute peak systolic velocity in normal patients, with a range of 20 cm/sec to 60 cm/sec.13 Up to three-quarters of all patients have a dominant vertebral artery, which demonstrates larger size and higher flows than the contralateral side, most often occurring on the left side.
Elevated Velocity and Stenosis
Abnormalities in vertebral artery flow hemodynamics caused by stenotic lesions can be detected readily from the spectral Doppler waveform characteristics and flow velocity data. The few prevalence and natural history studies on atherosclerotic stenosis of the vertebral artery that are available show that the vast majority of these lesions, greater than 90%, occur at the origin.16 Visible narrowing on color flow examination accompanied by high-velocity color aliasing and the mosaic pattern characteristic of poststenotic disturbed flow are findings indicating vertebral artery stenosis. The confirmatory evidence is high-velocity flow documented with spectral Doppler measurements. No velocity criteria are available to define the severity of vertebral artery stenoses; however, more than a focal doubling of velocity implies a greater than 50% diameter reduction. Ultrasound diagnosis of stenosis at the vertebral artery origin is complicated by the frequent occurrence of considerable tortuosity in the proximal 1 to 2 cm of the vertebral artery (Figure 11-6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree