Laboratory value
Unit
Normal reference range
Calcium, serum
mg/dl
8.3–10.4
Calcium, ionized
mg/dl
4.57–5.21
Parathyroid hormone, intact (PTH)
pg/ml
12–88
Phosphorus
mg/dl
2.5–4.5
Creatinine
mg/dl
0.6–1.5
Albumin
g/dl
3.4–5.0
24 h calcium, urine
mg/day
50–300
24 h creatinine, urine
g/day
0.8–2.0
25-hydroxy vitamin D (VitD25)
ng/ml
30–100
1,25-dihydroxy vitamin D (VitD1,25)
pg/ml
18–72
Magnesium, serum
mg/dl
1.7–2.4
26.2 Case Vignette 1: Hypercalcemic Crisis
A 64 year old man was hospitalized from his primary physician’s office after routine laboratory tests were obtained in follow-up of a recent admission for stroke. These were his presenting lab values: serum calcium 14.5, ionized calcium 8.5, PTH 94, 25 hydrroxy vitamin D level 17.6, phosphorus 2.2, creatinine 1.6, 24 h urinary calcium 296, and creatinine 1.0. Serum protein electrophoresis and PTH-related peptide were both normal. He was aware of potential parathyroid disease since 2011 and remembers undergoing a 99Tc-Sestamibi . He denied typical symptoms and side effects of parathyroid disease —kidney stones, polyuria/nocturia, neurocognitive changes, extreme fatigue, and arthralgias. Several months prior he had sustained an ankle fracture from a motorcycle accident. The patient denied childhood radiation exposure to the head and neck area or a family history of parathyroid disease . His exam was unremarkable for parathyroid disease -related abnormalities.
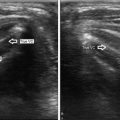
A report of the Sestamibi scan performed in 2011 indicated that there were four abnormal foci of uptake with the largest focus in the right lower neck. The same findings were re-demonstrated on the Sestamibi scan obtained during the current hospitalization (Fig. 26.1a, b). A bedside clinician-performed ultrasound detected four abnormal parathyroid glands , appreciating that the largest focus was actually a large superior parathyroid that descended into the tracheoesophageal groove , thus appearing to have a “lower” location (Fig. 26.1c, d; Videos 26.1, 26.2, 26.3, 26.4, 26.5, 26.6, and 26.7).


Fig. 26.1
(a) Sestamibi scan demonstrating four gland MGD , after initial injection of radiotracer. (b) Sestamibi scan clearly demonstrating four gland MGD , after delayed acquisition of images allowing radiotracer to wash out of thyroid gland. (c) Ultrasound image left upper parathyroid gland, transverse view. (d) Ultrasound image left upper parathyroid gland, longitudinal view
Four-gland exploration was planned once the patient was medically stable and transitioned off of anticoagulation for the stroke . The imaging findings were helpful in determining the sequence in which the parathyroid glands were exposed and which one could be fashioned into a viable remnant. All were histologically hypercellular parathyroid glands with the following sizes: right upper 4025 mg; right lower 120 mg; left upper 118 mg. The left lower parathyroid was biopsied (not weighed), since it was least abnormal in appearance and most suitable to leave in situ as a viable remnant. Normal parathyroid size is 15–50 mg, with mean weights approximately 30 mg. Intraoperative PTH declined by >50 % following excision of the large right upper parathyroid gland and would not have predicted MGD had imaging shown a single focus of disease.
This patient’s imaging findings are interesting because rarely do all four abnormal parathyroid glands appear clearly, and even rarer is the chance that two imaging studies agree on the same locations for MGD [12]. This case also illustrates how MGD in primary hyperparathyroidism can manifest with asymmetrical sizes and shapes of parathyroid glands .
26.3 Case Vignette 2: Tertiary Hyperparathyroidism and Thyroid Cancer
One month following kidney transplantation, a 55 year old woman was found to have serum calcium levels of 11–12 during a routine nephrology follow-up visit. She had been on dialysis for 10 years and this was her second kidney transplant. PTH level prior to transplant was approximately 2000 and had declined to 650 at presentation with hypercalcemia. Ultrasound detected markedly enlarged upper parathyroid glands that mimicked thyroid nodules because of their partial intrathyroidal positioning (Videos 26.8, 26.9, and 26.10). Furthermore, discreet thyroid nodules were also detected and classified into a high risk for malignancy category by sonographic features of interrupted peripheral calcifications and irregular margins (Videos 26.11 and 26.12). The patient underwent total thyroidectomy with central neck lymph node dissection and concomitant subtotal parathyroidectomy, leaving a small in-situ parathyroid fragment. Histology confirmed multifocal bilateral papillary thyroid cancer and four hyperplastic parathyroid glands . She has no evidence of recurrence for both conditions at nearly 1 year of follow-up after surgery .
This case illustrates the fact that ultrasound identifies previously unrecognized thyroid nodules and thyroid cancer . Coexistent pathology is identified in approximately 30–50 % of cases [21, 22]. In one study ultrasound identified previously silent thyroid nodules in one-third of patients with hyperparathyroidism, and the rate of thyroid cancer in patients with hyperparathyroidism was 7 % [12].
26.4 Case Vignette 3: Double Superior Parathyroid Adenomas Versus 4-Gland Hyperplasia
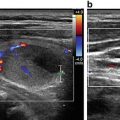
Two years following a focused parathyroidectomy to remove a 5 cm right upper parathyroid, a 71 year old man was found to be hypercalcemic. At the initial operation, intraoperative PTH was not available. His biochemical serum and urine parameters were diagnostic of primary hyperparathyroidism at the original time of presentation and were confirmed at this recent presentation. Sestamibi scan (Fig. 26.2a) detected only a single strong focus of radiotracer uptake in the left neck prior to reoperative surgery. This corresponded to a large (3–4 cm) left upper parathyroid gland on ultrasound (Fig. 26.2b, Videos 26.13, 26.14, and 26.15). A subtle echogenicity was also appreciated at the tip of the left lower pole (Fig. 26.2c, Video 26.15) and alerted the surgeon to explore this area as well. Intraoperatively, both the left upper and lower parathyroid glands were abnormally enlarged. Exploration of the right lower parathyroid revealed a third abnormal parathyroid gland. A portion of this parathyroid was fashioned into a remnant while the remaining parathyroid tissue was excised. Histology confirmed hypercellular parathyroid glands with the following sizes: left upper 2673 mg, left lower 80 mg with cystic degeneration; right lower fragment confirmed as hypercellular. Intraoperative PTH level declined from 262 to 30 following excision of only the large left upper gland, hence failing to predict the additional abnormal glands. In follow-up, calcium and PTH levels are 9.1 and 10, respectively.


Fig. 26.2
(a) Sestamibi scan showing only large single focus of radiotracer in left neck. (b) Ultrasound image left upper parathyroid, longitudinal view, showing extent of enlargement nearly as long as the thyroid lobe itself. (c) Ultrasound image left lower parathyroid (circled in red). Keeping this image in mind, viewing of Video 26.15 cine clip may be helpful
This case illustrates the more typical clinical situation where Sestamibi scan detects only one gland in MGD . Ultrasound and a low threshold to suspect MGD were essential to this patient avoiding a third surgery for persistent hyperparathyroidism. Because of the sestamibi results the surgeon might have considered that the patient actually had two large superior parathyroid adenomas, which are the most commonly encountered double adenoma combination [23]; however, the subtle findings on ultrasound helped clarify the presence of 4-gland disease.
26.5 Case Vignette 4: Primary Hyperparathyroidism in Pregnancy
A 37 year old woman presented during her second pregnancy with fluctuating calcium values. She had been told 5 years previously during her first pregnancy that she has primary hyperparathyroidism. Lack of medical insurance had prevented her from seeking additional treatment previously and there were no adverse effects from maternal hypercalcemia on the first baby. The patient had multiple kidney stones over the last several years, fatigue and osteopenia. Her biochemical profile was unusual and the following laboratory values are grouped in brackets by two separate dates tested: [calcium 10.7, ionized calcium 6.0, PTH 43, 25 hydroxy vitamin D 22.7, 1,25 dihydroxy vitamin D 102, 24 h urinary calcium 631] and [calcium 11.6, ionized calcium 6.31, PTH 26, 25 hydroxy vitamin D 13.4, 1,25 dihydroxy vitamin D 133, creatinine 0.58, albumin 4.4].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree