Fig. 22.1
(a) Gray-scale US . Benign appearing oval 1-cm lymph node, in the longitudinal plane, with a normal central echogenic hilum (arrow). (b) Gray-scale US. Benign appearing oval 1-cm lymph node, in the transverse plane, with normal echogenic hilum (arrow). (c) Gray-scale US. Benign 0.8-cm lymph node in the longitudinal plane demonstrating the linear hypoechoic course of the vessels through the central echogenic hilum. (d) Power Doppler. US demonstration of the linear course of the vein within the central hilum of a 0.8-cm benign lymph node imaged in the longitudinal plane. (e) Power Doppler US demonstration of the organized course of the vein within the central hilum of a 0.8-cm lymph node imaged in the transverse plane
Diagnosis: Benign appearing 0.7–cm oval lymph node in the soft tissues of the left mid-jugular territory. No biopsy was performed due to the benign appearance of the node in both the longitudinal and transverse planes. In this patient, the echogenic central hilum is normal.
22.2.2 Case 2: The Importance of Assessing for Symmetry of Cervical Lymph Nodes in the Superior Jugular Territories to Assess for Benign or Metastatic Involvement
Interestingly, the benign lymph nodes in the superior jugular territories vary in appearance compared to the benign lymph nodes in the mid- and lower jugular territories. Left and right lymph nodes in the superior jugular territories should be compared on side-by-side images to assess symmetry. Asymmetry suggests metastatic involvement.
Clinical Scenario: A 51-year-old female with a 3-year history of bilateral papillary thyroid cancer who presents with a palpable right superior neck lymph node which by patient history has been enlarging. US was requested to assess the palpable lymph node.
Imaging Features: Ultrasound. On initial US evaluation, the 1.3-cm right superior neck lymph node (Fig. 22.2a) was thought to potentially be metastatic with loss of central hilum. There was no vascular flow or calcification. US-guided biopsy was considered.
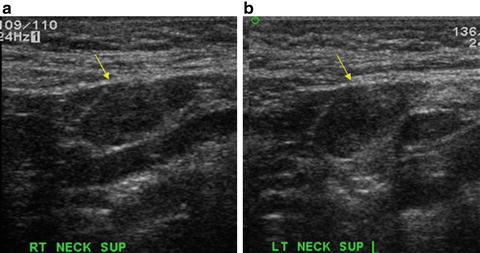
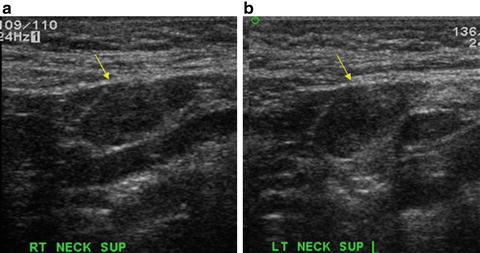
Fig. 22.2
(a) Gray-scale US . 1.3-cm right superior neck lymph node, imaged in the longitudinal plane, with absent central hilum initially of concern for a metastatic lymph node (arrow). (b) Gray-scale US. Contralateral 1.4-cm left superior neck lymph node, imaged in the longitudinal plane, with a symmetrical appearance suggesting benign symmetrical lymph nodes in the superior jugular territories (arrow)
Comparison with the contralateral 1.4-cm left superior neck node (Fig. 22.2b) revealed a symmetrical appearance suggesting that the lymph nodes were either both benign or bilateral metastatic adenopathy .
US-guided FNA was considered based on concern for absent hilum and prominent rounded lymph nodes which may have been caused by bilateral metastasis.
Diagnosis: US–guided biopsy was performed on the right and left superior neck lymph nodes. The FNAs revealed benign nodes with no malignant cells. In this case, the symmetry of the superior neck nodes was within normal limits.
22.2.3 Case 3: The Importance of Assessing for Symmetry of Cervical Lymph Nodes in the Superior Jugular Territories to Assess for Metastatic Involvement
Ultrasound imaging of the soft tissues of the neck should include a two-on-one image of the right and left superior neck lymph nodes for comparison. Symmetry may assist in defining the benign appearance of the superior neck nodes in a specific patient.
Clinical Scenario: A 47-year-old male with right thyroid follicular variant of papillary cancer and palpable lymph nodes in the right and left superior neck. US was requested to assess the palpable superior neck lymph nodes.
Imaging Features: Right superior neck palpable 1.4-cm lymph node (Fig. 22.3a) created concern for an enlarged metastatic lymph node until comparison of 1.5-cm palpable left superior neck lymph node (Fig. 22.3b). The asymmetry suggests that the left superior neck lymph node is the metastatic node.
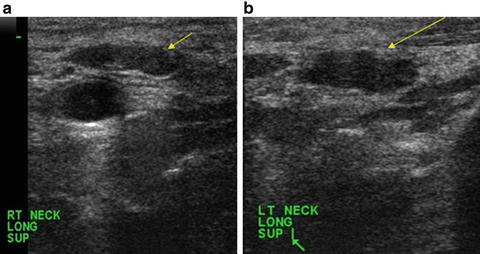
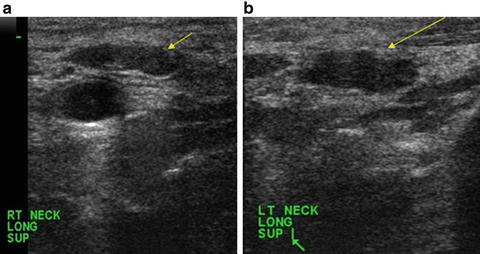
Fig. 22.3
(a) Gray-scale US . Palpable right superior neck 1.4-cm lymph node was of concern for an enlarged metastatic lymph node (arrow). (b) Gray-scale US. Comparison of contralateral 1.5-cm palpable asymmetric left superior neck lymph node with asymmetry suggesting a metastatic lymph node (arrow)
Diagnosis: US–guided FNA of the right and left superior neck lymph nodes revealed that the 1.4–cm right superior neck palpable lymph node was benign and the left 1.5–cm palpable lymph node was metastatic papillary carcinoma.
We have found that traditional criteria of size greater than 0.5 cm, shape of taller than wide, and irregular borders are not powerful indicators of malignancy. Although no single sonographic feature is pathognomonic for a metastatic lymph node, certain features should raise suspicion of a malignant lymph node. The combination of several features may be even more suggestive of metastatic adenopathy . These features include a full or rounded shape, disrupted or displaced hilum, disorganized vascularity, calcifications, cystic change, bulging of a component of the lymph node, and the presence of intranodal punctate regions of increased echogenicity. Of importance is that ultrasound characteristics are sensitive but not disease specific for a metastatic lymph node. Thus, US-guided FNA should be performed on lymph nodes of concern to establish the diagnosis.
22.2.4 Clinical Case 4: Distorted Hilum in a Metastatic Lymph Node
Metastatic involvement of a lymph node may present as distortion of the normal echogenic central hilum.
Clinical Scenario: A 46-year-old female with 0.9-cm right papillary thyroid carcinoma and 1.1-cm right mid-neck node.
Imaging Features: Abnormal right mid-neck lymph node with displaced hilum in the longitudinal (Fig. 22.4a) and transverse (Fig. 22.4b) planes.
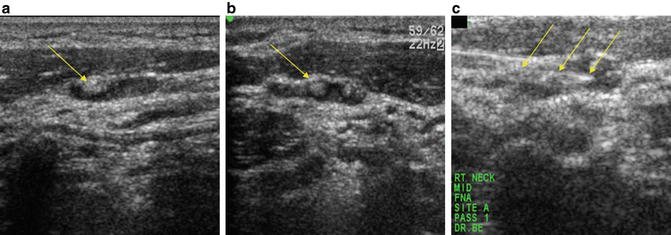
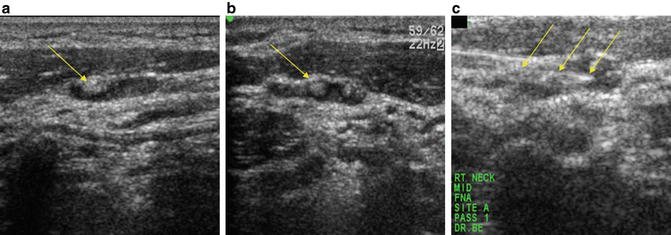
Fig. 22.4
(a) Gray-scale US . Abnormal-appearing 1.1-cm right mid-neck lymph node, in the longitudinal plane, with a displaced hilum causing concern for metastasis (arrow). (b) Gray-scale US. Abnormal-appearing 1.1-cm right mid-neck lymph node, in the transverse plane, with a displaced hilum causing concern for metastasis (arrow). (c) Gray-scale US. US-guided FNA of the right mid-neck lymph node with the biopsy needle tip within the lymph node (arrows)
22.2.5 Case 5: Absent Hilum in a Metastatic Lymph Node
The hilum may be absent in a metastatic lymph node due to infiltration of metastasis.
Clinical Scenario: A 72-year-old male with a 3-year history of 0.6-cm right PTC and a new palpable left mid-neck lymph node. Ultrasound was requested to assess the jugular territory lymph nodes.
Imaging Features: Abnormal 0.5-cm left inferior neck lymph node (Fig. 22.5a) and 1.2-cm palpable left mid-neck lymph node (Fig. 22.5b) in the transverse planes with hilum absent in both lymph nodes.
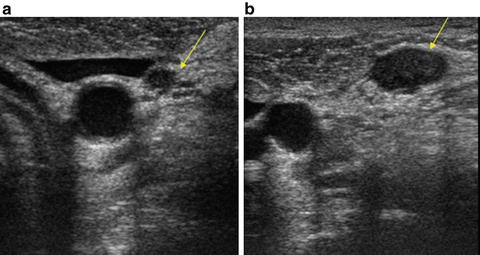
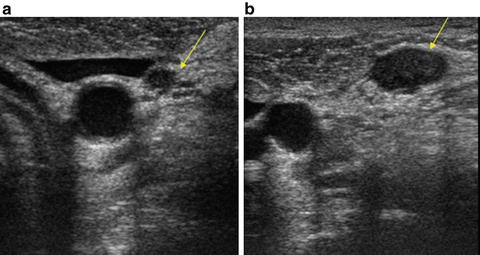
Fig. 22.5
(a) Gray-scale US . Abnormal 0.5-cm left inferior neck lymph node, in the transverse plane, with absent hilum causing concern for a metastatic lymph node (arrow). (b) Gray-scale US. Abnormal 1.2-cm left inferior neck lymph node, in the transverse plane, with absent hilum causing concern for a metastatic lymph node (arrow)
Diagnosis: US–guided FNA revealed anaplastic transformation of PTC in the left and right jugular territories.
22.2.6 Case 6: Disorganized Vascular Flow in a Metastatic Lymph Node
Vascular flow normally transverses the central echogenic hilum in a linear configuration. Metastatic infiltration of a lymph node may cause disorganization of the vascular flow.
Clinical Scenario: A 40-year-old female a with 2-year history of 2.5-cm right PTC and currently with a palpable right inferior jugular territory lymph node.
Imaging Features: Abnormal 0.8-cm right inferior neck lymph node, in the longitudinal plane, with disorganized vascular flow (Fig. 22.6a) and a 2.5-cm right superior jugular territory lymph node in the longitudinal plane with normal central hilar vascular flow for comparison (Fig. 22.6b).
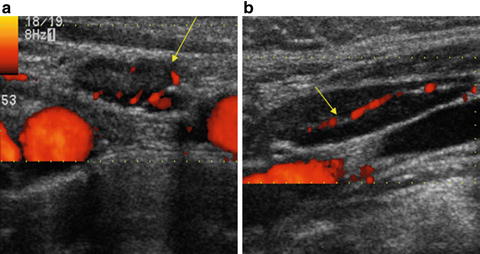
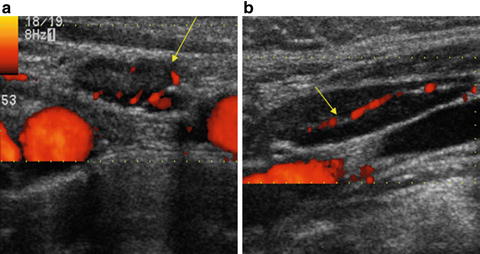
Fig. 22.6
(a) Power Doppler US . Abnormal 0.8-cm right inferior neck lymph node, in the longitudinal plane, with disorganized vascular flow causing concern for metastatic adenopathy . (b) Power Doppler US. Comparison of superior jugular territory lymph node in the longitudinal plane with normal central hilar vascular flow
Diagnosis: US–guided FNA revealed papillary thyroid cancer.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree