© Springer International Publishing Switzerland 2017
Mira Milas, Susan J. Mandel and Jill E. Langer (eds.)Advanced Thyroid and Parathyroid Ultrasound10.1007/978-3-319-44100-9_4040. Ultrasound for Endocrinologists: What I Learned from Lifetime Practice
(1)
Division of Endocrinology, Diabetes and Metabolism, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA 19104, USA
Keywords
Ultrasound imagingEndocrinologyEndocrinologistsReflections on ultrasound imaging of the thyroid and the neck over more than two decades of use as an endocrinologist trigger both exhilaration and humility, which are persistently coupled as I continue to practice of the art of imaging. Throughout my career, I have been fortunate to partner with and learn from skilled and dedicated colleagues from multiple specialties to provide optimal care for my patients.
40.1 Exhilaration
40.1.1 What You Can See
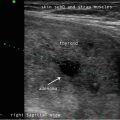
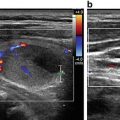
Anatomy is awesome. There is the thrill of visualizing the intricacies and three-dimensional relationships of the neck structures which may particularly resonate with those physicians in disciplines where these spatial relationships have not been encountered since first year medical school anatomy. Ultrasound (US) demonstrates transverse processes of the cervical vertebrae, vagal nerves, the esophagus, great vessels and smaller ones, the vocal cords, salivary glands, the thymus, the origin of the superior thyroidal artery from the carotid and the inferior thyroidal artery the traverses the great vessels to originate from the thyrocervical trunk. And US allows unforeseen detection of nonthyroid pathology—sarcoidosis based upon lymph node appearance, Sjogren’s because of heterogeneity of the salivary glands, thyroglossal duct cysts, lymphomas, and other malignancies associated with metastatic cervical adenopathy .
Sonographic imaging of the thyroid enhances our understanding of pathophysiology. We can diagnose autoimmune thyroid disease based upon parenchymal heterogeneity and detect thyroid nodules that we otherwise cannot palpate, measuring a few millimeters to over 3 cm. The compendium of literature informs us about the association of a nodule’s malignancy risk with its sonographic appearance. For patients undergoing thyroid surgery, imaging of cervical lymph nodes can optimize the surgical procedure by detecting nonpalpable metastatic disease.
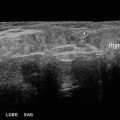
As an educator, sonographic imaging complements physical diagnosis. US delineates the anterior contour of the thyroid gland, making evident what should be detected on a physical examination. An irregular thyroid contour as found in Hashimoto’s thyroiditis translates to the firm gritty sensation felt on exam. And US makes it clear that the 2 cm nodule thought to be palpable by another clinician is clearly not because there is no forward displacement of the anterior surface of the thyroid. Conversely, US confirms that the 8 mm isthmus nodule located only 6 mm below the skin surface should be evident on a physical examination .
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree