Ultrasound in Prehospital and Austere Environments
The term “out-of-hospital ultrasound” refers to sonographic examinations performed in a wide variety of settings outside of traditional hospital departments, laboratories, and freestanding imaging centers. “Prehospital ultrasound” is synonymous, even though this term is mostly used in reference to EMS and tactical medicine applications. Prehospital ultrasound examinations are generally not performed by radiologists or clinicians; caregivers incorporate the use of ultrasound into the initial patient assessment at the point of care in the prehospital setting. The images obtained provide real-time morphologic and functional clinical information. In the emergency and critical care literature, “point-of-care ultrasound” most commonly refers to “bedside emergency ultrasound” since the scientific debate has been originally focused on patients being cared for in the ED; the resuscitation, operative, or recovery room; the intensive care unit; the diagnostic imaging department; or other medical and surgical wards. Diagnostic and therapeutic advances have allowed “critical care” to be taken outside of the hospital setting to the scene of illness and injury in a wide variety of settings (Table 4-1).
 TABLE 4-1. OUT-OF-HOSPITAL ULTRASOUND SETTINGS AND PROVIDERS
TABLE 4-1. OUT-OF-HOSPITAL ULTRASOUND SETTINGS AND PROVIDERS
In all of these settings, ultrasonography provides a visual extension of the clinical examination, permitting more accurate assessment of anatomic and physiologic integrity in complex states of illness and injury (Figures 4-1 and 4-2). Prehospital applications are generally incorporated into defined problem-based clinical pathways rather than organ-based categorizations (i.e., “shock assessment” rather than “liver assessment”).
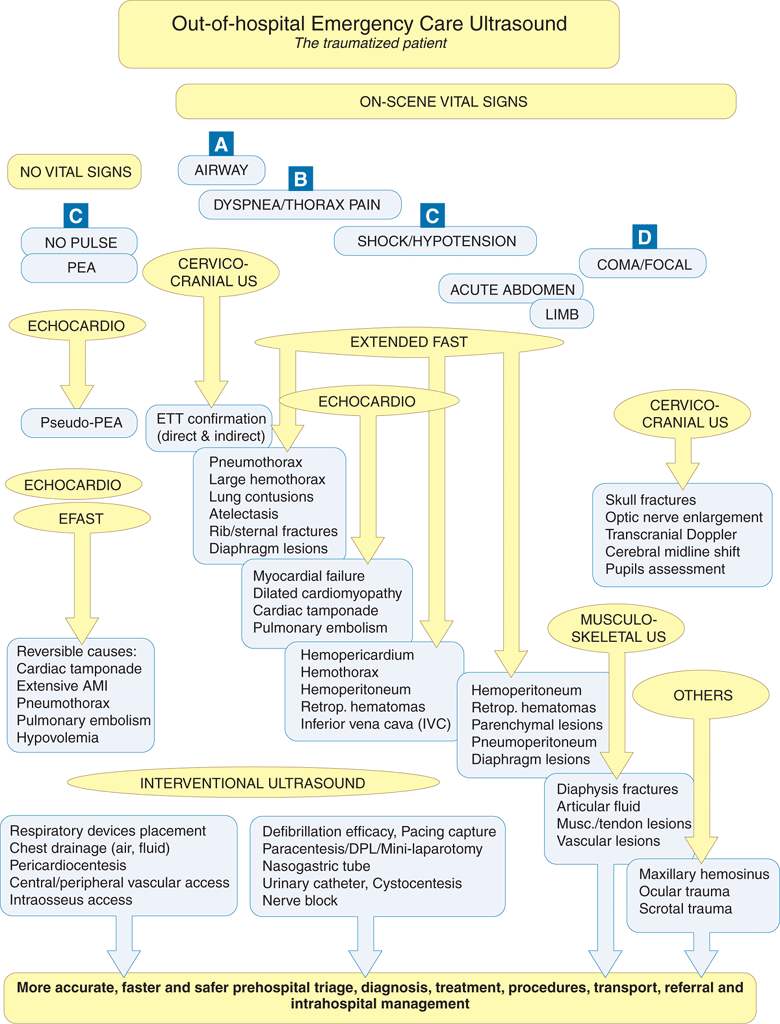
Figure 4-1. ABCD-conformed ultrasound applications in out-of-hospital setting.
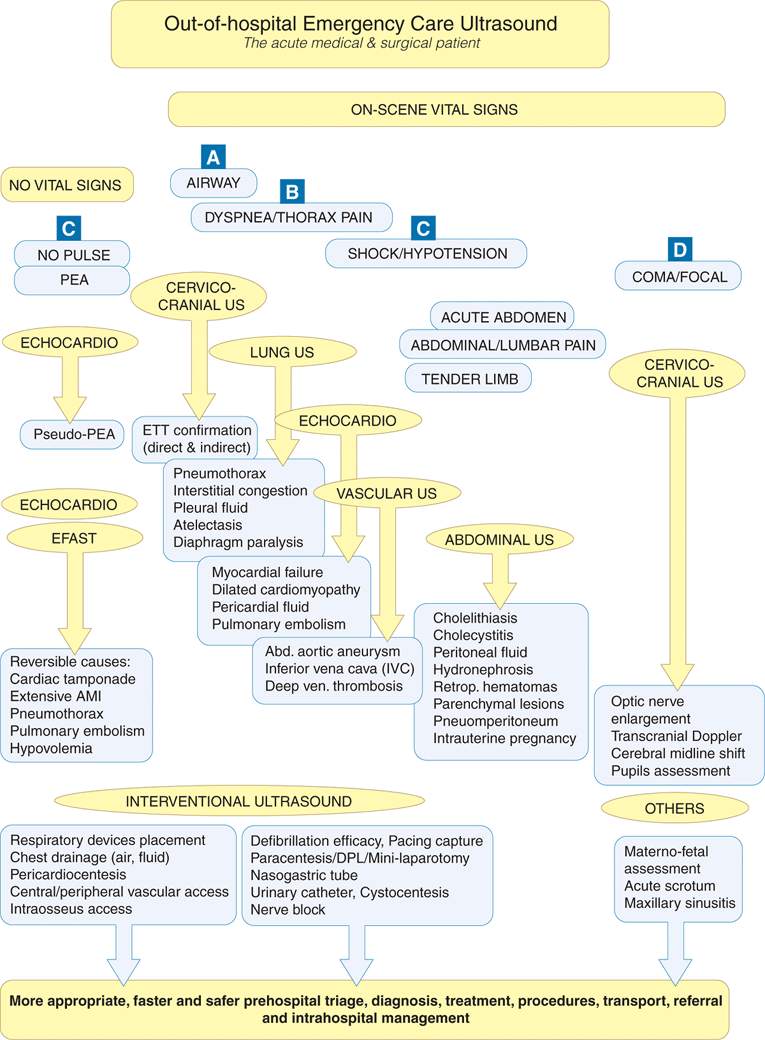
Figure 4-2. Current level 1 ultrasound applications in out-of-hospital setting: ABCD-conformed pathways for the acute medical and surgical patient.
Clinical accuracy and timeliness are essential for successful decision making and problem-solving in the prehospital environment. The prehospital use of ultrasonography can improve initial data gathering, which enhances the delivery of acute care in a timely and effective fashion. Efforts are being made to identify its most appropriate applications in the prehospital setting, the technical feasibility and reliability of its use, prehospital provider training and competency requirements, and the impact of prehospital ultrasound on patient outcomes and community health.1–10
To highlight the growing evidence in support of prehospital ultrasound, this chapter will review the experience of the German, Austrian, French, and American helicopter and ground-based EMS. This chapter will also review ultrasound in tactical medicine, remote telementored ultrasound, and the use of ultrasound in under-resourced settings.
Germany
The German emergency system takes advantage of a close alliance between emergency physicians and the rescuing service staff prior to transportation to the hospital. The overriding principle of on-scene care is “stay and play” in nontraumatized patients and “treat and run” in traumatized patients; however, this is in contrast to the “scoop and run” principle of most international prehospital systems. The implementation of ultrasonography into such a system is supported by the development of two major concepts and training programs: Prehospital Focused Assessment with Sonography for Trauma (P-FAST) and Focused Echocardiographic Evaluation in Life Support (FEEL) for emergency and critical care physicians, and partially paramedics. Those protocols are embedded as “understand, treat and run” into the prehospital workflow.
 PREHOSPITAL FOCUSED ASSESSMENT WITH SONOGRAPHY FOR TRAUMA
PREHOSPITAL FOCUSED ASSESSMENT WITH SONOGRAPHY FOR TRAUMA
P-FAST is related to prehospital trauma care. Clinical estimates of intraperitoneal bleeding at the trauma scene are difficult to accurately assess. A blunt trauma patient with normal vital signs and an unremarkable physical examination may have massive intraperitoneal bleeding that requires urgent operative management for hemorrhage control. Data from several studies support the role of prehospital ultrasound in enhancing detection of intraperitoneal hemorrhage.10,11
The 2001 Frankfurt/Main pilot study and a subsequent prospective multicenter study of P-FAST investigated its feasibility in trauma care.10,11 Five air rescue centers in southwestern Germany and one ground ambulance rescue team in Frankfurt/Main took part in these studies. The entire P-FAST examination took about 2 minutes when results were negative, whereas positive intraperitoneal sonographic findings could be detected within seconds. Prehospital diagnosis of intraperitoneal injury by ultrasound was made approximately half an hour prior to arrival at the ED. In more than 90% of the cases, there was enough time to complete the P-FAST examination on the scene or during transportation. In a few cases, ultrasound could not be completed because of suboptimal conditions (e.g., subcutaneous emphysema, patient obesity, or lack of time). The P-FAST examination had a sensitivity of 93% for the detection of intraperitoneal hemorrhage. The investigators concluded that P-FAST had potential as a useful, reliable diagnostic tool in surgical triage at the trauma scene.11
All rescue teams involved in the multicenter study stated that P-FAST had an important impact on decision making. In approximately one-third of the cases, the findings of P-FAST had an influence on trauma management at the scene. Whenever intraperitoneal bleeding was detected, the prehospital phase of care was minimized to enable immediate transportation, either by ground or by helicopter. In contrast, if the findings of P-FAST were negative, the routine algorithm for trauma care at the scene was followed by completion of the primary and secondary surveys in accordance with the principles of advanced trauma life support (ATLS). The ultrasound findings led to a change in the choice of admitting hospital in approximately 20% of the cases. In addition, the results of P-FAST gave surgeons additional information that allowed appropriate planning of the hospital phase of care.
 FOCUSED ECHOCARDIOGRAPHIC EVALUATION IN LIFE SUPPORT
FOCUSED ECHOCARDIOGRAPHIC EVALUATION IN LIFE SUPPORT
FEEL is an ACLS-compliant echocardiographic assessment and also addresses the development of skills for acute and critical care physicians in time-dependent scenarios.1 The aim of FEEL is to elucidate treatable conditions and not to terminate CPR. Entities such as pulmonary embolism, pericardial tamponade, global left ventricular failure, and hypovolemia should be identified during the initial resuscitation. A major challenge is recognizing return of spontaneous circulation when no central pulse is palpable and differentiating pulseless electrical activity (PEA) states with or without wall motion. New evidence suggests that echocardiography can identify a “subclinical” return of spontaneous circulation (i.e., mechanical cardiac output).
The FEEL algorithm is a structured workflow within the ACLS clinical management approach that can be applied in real time. The 2010 American Heart Association resuscitation guidelines recommend high-quality CPR with minimal interruptions to reduce no-flow intervals. The 2010 European Resuscitation Council guidelines have now incorporated suggestions for ultrasound concepts for identification and treatment of reversible causes or complicating factors and training of ALS-conformed ultrasound.
Studies have evaluated the FEEL concept for its ease of implementation into the CPR process and its ability to identify characteristic pathologies.12–14 The FEEL examination is a 10-step procedure (Table 4-2) designed to be performed during CPR cycles in order to reduce unwanted interruptions. Prehospital indications for performing FEEL are listed in Table 4-3.
 TABLE 4-2. THE 10-STEP FOCUSED ECHOCARDIOGRAPHIC EVALUATION IN LIFE SUPPORT (FEEL) ALGORITHM
TABLE 4-2. THE 10-STEP FOCUSED ECHOCARDIOGRAPHIC EVALUATION IN LIFE SUPPORT (FEEL) ALGORITHM
 TABLE 4-3. PREHOSPITAL INDICATIONS TO PERFORM FOCUSED ECHOCARDIOGRAPHIC EVALUATION IN LIFE SUPPORT (FEEL)
TABLE 4-3. PREHOSPITAL INDICATIONS TO PERFORM FOCUSED ECHOCARDIOGRAPHIC EVALUATION IN LIFE SUPPORT (FEEL)
“Pre-resuscitation” care, shock assessment
Penetrating trauma, blunt trauma
Postcardiotomy due to cardiac surgery
Hypotension, shock of unknown origin
Unconsciousness, unresponsiveness
Acute severe dyspnea
Syncope in young adults
Vein thrombosis
AMI, mechanical complications of AMI
“Atypical” chest pain: suspected aortic-dissection, suspected
aortic abdominal or thoracic aneurysm, nontraumatic
cardiac rupture
Iatrogenic complications following invasive procedures
(e.g., insertion of an artificial pacemaker, pulmonary artery
catheter, and electrophysiologic investigative procedures)
Great-vessel disease
CPR
PEA
Bradycardia-asystole, pacemaker-ECG
Suspected cardiac tamponade
Early detection of return of spontaneous circulation
Effectiveness of chest compressions
Postresuscitation care
Hypotension, adaptation of vasopressors
A prospective, observational trial in the prehospital setting tested (a) the capability of FEEL to differentiate PEA states and (b) the feasibility of FEEL using a mobile, battery-powered ultrasound system. Trained emergency physicians applied the FEEL examination as described. A total of 230 patients were included, with 204 undergoing a FEEL examination during ongoing cardiac arrest (100) and in a shock state (104). Images of diagnostic quality were obtained in 96%. In 35% of those with an ECG diagnosis of asystole, and 58% of those with PEA, cardiac motion was detected, and associated with increased survival. Echocardiographic findings altered management in 78% of cases.12
 EDUCATION AND TRAINING
EDUCATION AND TRAINING
Before 2001, a uniform course to teach P-FAST was unavailable in Germany or other parts of Europe. Prior to the P-FAST studies, it was necessary to set up a structured educational program for emergency physicians and paramedics. A P-FAST course concept was developed on the basis of several studies that had been performed in the 1990s with respect to the use of ultrasound in the clinical setting. Some groups had investigated which type of education programs were required to gain competency in performing the FAST examination and had assessed the learning curve. The recommended duration of didactic training, including hands-on experience, ranged from 2 to 30 hours.
The main goal of the P-FAST training is to prepare participants for uncommon situations in trauma scenarios under field conditions. The 1-day course in P-FAST includes both didactic and hands-on training. The didactic session includes a general introduction to ultrasound, physics of ultrasound, and the causes and relevance of artifacts and shadows that may be encountered during an ultrasound examination. Participants are introduced to the rationale for performing ultrasound as part of trauma management and are taught how to integrate P-FAST into the prehospital algorithm for trauma care. Numerous images and videos provide an overview of the physiologic and pathologic situations. Hands-on training is the main focus of the course. Participants perform the P-FAST examination under the supervision of clinicians experienced with ultrasound. The ratio of instructors to students is 1:2 or 1:3. During the course, a trainee performs 30–40 ultrasound examinations under the supervision of the instructors.
In the first part of hands-on training, participants perform the standardized procedure of P-FAST on healthy and patient volunteers. Patient volunteers have positive findings for free intraperitoneal fluid secondary to peritoneal dialysis or ascites. In the second part of the hands-on training, students learn how to perform the ultrasound examination under difficult circumstances, such as on patients found in challenging prehospital conditions. In the third part, real-time scenarios are presented with healthy or patient volunteers found in critical situations following a traumatic event. These scenarios include surgical triage of three or more victims or volunteers trapped in the wreckage of a vehicle. Evaluation of the course program is consistent with data from other training evaluations in the literature, which have shown that these programs produce competent examiners and are associated with a steep learning curve. No significant differences were found between emergency physicians and paramedics in terms of sensitivity, specificity, and accuracy of P-FAST examinations.
A 1-day course was established on focused echocardiography for emergency physicians and critical care physicians who had no previous experience in performing echocardiography.13 The course emphasizes basic echocardiography, rapid evaluation, and communication skills. In addition, a real-time 3D-ultrasound simulation combined within a full-scale ACLS training system as well as web-based learning and tests are included. We also evaluated an emergency physician’s ability to obtain a correct subxiphoid 4-chamber view and to interpret a 5-second echocardiogram of normal and pathologic findings. We found that emergency physicians could learn to identify some simple pathologic findings on very short video clips, and for the combined ultrasound and ACLS trainer there were high positive ratings. In 2011, P-FAST and FEEL became incorporated into the nationwide certified training programs of the German Society of Ultrasound in Medicine (DEGUM) and German Society of Anesthesiology, Intensive and Emergency Care (DGAI) as extended-FAST (E-FAST) (including lung ultrasound) and cardiosonography modules.
 MOBILE ULTRASOUND DEVICES
MOBILE ULTRASOUND DEVICES
Prior to the German P-FAST multicenter study, the fire department of the city of Frankfurt and the Department of Trauma Surgery at the University of Frankfurt used a device based on Esaote Tringa. The compact ultrasound machine SonoSite 180 Plus is used by the German Army and in the MedEvac system operating worldwide. The SonoSite NanoMaxx is standard of care in an increasing number of prehospital care services. Up to 35 German air rescue helicopter services, Lufthansa German Airline, and fire department-based emergency services of several metropolitan areas are equipped with General Electric Vscan.
These mobile devices can be held with one hand; the adjustments necessary during an examination can be made with the thumb. It is now very well received that our concepts also apply to many acute care settings for point-of-care exams within the hospital.
 PROPAGATION OF PREHOSPITAL ULTRASOUND IN AIR AND GROUND RESCUE SERVICE
PROPAGATION OF PREHOSPITAL ULTRASOUND IN AIR AND GROUND RESCUE SERVICE
Since 2003, the German Air Rescue Organization (Deutsche Rettungsflugwacht) has incorporated P-FAST into the algorithm for trauma management. By 2012, 35 helicopters and 3 fixed-wing aircrafts were equipped with portable ultrasound devices and most of the emergency physicians and paramedic crews were trained. The other main provider of air rescue services, the German Automobile Club, also partially adopted P-FAST.
Some air rescue centers of the German federal police have implemented P-FAST; in addition, the German Air Force also have equipped their international mobile medical crews and supplied their aircraft for multinational flights with mobile ultrasound devices. Their crews have been trained in our courses.
P-FAST and FEEL have been integrated into ground-based services as well. The region of Darmstadt adopted the prehospital FEEL examination in 2002. In Frankfurt/Main, the five ground-based ambulances staffed by emergency physicians have been equipped with portable ultrasound devices with financial support from the city’s public health department.
Austria
In Austria, physicians, who staff ambulances, treat prehospital patients. As a result, prehospital portable ultrasound as well as other specialized point-of-care diagnostic tools, such as blood gas analysis systems, invasive blood pressure monitoring, and fiberoptic bronchoscopy, have become available. The first emergency vehicle in Graz was equipped with portable ultrasound (SonoSite 180 Plus) in 2000. Today, up to three emergency vehicles in Graz are equipped and some other emergency systems have also implemented its use. While prehospital ultrasound was almost exclusively applied to detect free intraabdominal fluid in trauma patients in the initial years, its applications have been extended. An increasing number of emergency physicians have begun using prehospital ultrasound for differentiation between cardiac and pulmonary causes of dyspnea with the evaluation of B-lines, the prediction of outcome in cardiac arrest patients, the detection of pneumothorax, and ultrasound-guided venous and arterial line insertion. A report published by the Graz group studied the prognostic value of prehospital emergency echocardiography in cardiac arrest and the ability of optic nerve ultrasound to detect elevated intracranial pressure.14 Although prehospital emergency ultrasound is still in its infancy in Austria, the results and improvement in patient care have been promising and groundbreaking.
France
The feasibility and usefulness of prehospital ultrasound have expanded since the early 1980s in France. Bulky ultrasound machines requiring very skilled operators were used back then; as a result, they had limited applicability to most prehospital systems. In the early 1990s, technological advances produced lighter ultrasound machines that were much more practical to use in the prehospital setting.
French prehospital clinicians have been interested in broad applications of prehospital ultrasound. Investigators have studied the detection of free intraperitoneal fluid, assessment of cardiac function in shock and arrest states, evaluation of thoracic injuries, detection of deep venous thrombosis, assessment of long diaphysis fractures, and detection of optic nerve enlargement.
The methods of training and the level of performance of emergency physicians using ultrasound in prehospital settings in France were evaluated. The ultrasound training was scheduled for one half-day session that included didactic and practical instruction. Like our German colleagues, didactic sessions reviewed the guiding principles of ultrasonography and normal and pathological images. The practical training consisted of performing examinations on healthy subjects or on patients with pertinent findings on ultrasound examinations (e.g., patients with ascites). The training focused on examinations pertinent to the French prehospital setting, which included the assessment for pneumotho-races, pleural effusions, abdominal or pericardial effusions, or deep venous thrombosis of the lower limbs.
Eight physicians of the SAMU 93 (EMS department) were trained on the emergency use of a portable ultrasound device (SonoSite 180). The number of training sessions varied from 1 to 6, according to the experience level of the operators. Each operator determined a clinical diagnostic probability (before ultrasonography) noted on an analog visual scale from 0 (absence of lesion) to 10 (presence of lesion). According to the same principle, the operator determined a second probability after ultrasound. The hospital follow-up of the patients made it possible to obtain the final diagnosis (0 for absent and 10 for present lesion) that was compared with the pre- and posttest probabilities.3
The initial analysis of 83 ultrasound examinations carried out on 40 patients revealed a median time of examination of 5 minutes, 100% sensitivity, 98% specificity, a positive predictive value of 92%, and a negative predictive value of 100%. In our analysis of the learning curve for ultrasound proficiency by prehospital providers, we found that the number of ultrasound examinations required to achieve desired proficiency was approximately 25 examinations.
The absolute difference between the probabilities before and after ultrasound was calculated and compared with the final diagnosis (0 or 10). When ultrasound had brought the operator closer to it, a positive value was allotted to the obtained number; conversely, a negative value was allotted when ultrasound had moved the operator away from the final diagnosis. For example, if a diagnostic probability was 3 before and 8 after ultrasonography, the absolute difference was 5 (8 – 3). If the final diagnosis was positive (presence of a lesion), ultrasound would have brought the operator closer to the final diagnosis. The value allotted to ultrasound would then be + 5. Conversely, if the final diagnosis was negative (absence of lesion), ultrasound would not have been helpful in making the final diagnosis. The value allotted to ultrasound would then be – 5.
The results of 302 ultrasound examinations were analyzed. The median impact of ultrasound on the final diagnosis was +2. The diagnostic performance was improved by ultrasound in 67% of the cases; it was not modified in 25% of the cases and it was degraded in 8% of the cases. Our results were consistent with the use of ultrasound as a “complement” to the clinical assessment.3
In France, prehospital ultrasound has established itself as a legitimate clinical adjunct. Just as the stethoscope serves as an extension of the physician’s ears, the ultrasound transducer serves as an extension of her hands and eyes. If the indications are focused, the procedure is codified, and the operators are properly trained, then the level of performance approaches that of a medical imaging expert. The rapidity of the examinations provides additional diagnostic information without delaying transport or definitive care. As experience with this modality increases and technological advances produce improved portability and resolution, we believe that the use of ultrasound will gain broad acceptance in prehospital venues around the world.
United States of America
The advancement of prehospital ultrasound in the United States has been significant. While no large randomized prehospital study has yet to be completed in the United States, the body of literature is increasing. Four broad areas are utilizing prehospital ultrasound: helicopter EMS, ground EMS, tactical, and tele-transmission of ultrasound. While the American EMS system has not swayed from expeditiously transporting ill or injured patients to the receiving medical center for definitive care, ultrasound may expand the traditional tools that prehospital providers use in their care of patients.
 AIR AND GROUND MEDICAL TRANSPORT
AIR AND GROUND MEDICAL TRANSPORT
Point-of-care ultrasound use in helicopter EMS is growing. This growth is not surprising given the critical and time-sensitive nature of helicopter EMS patients. Helicopter EMS transport in the United States has consistently grown each year for the past two decades. Approximately 867 rotor-wing air ambulances currently operate out of 714 bases across the country.15 For millions of rural Americans prompt emergency care is only accessible through the use of helicopter EMS.
Numerous United States helicopter EMS programs are now utilizing or have utilized ultrasound. Some programs include Oregon Health & Science University, Portland, Oregon; MetroHealth Medical Center, Cleveland, Ohio; Medical College of Georgia, Augusta, Georgia; University of San Diego, San Diego, California; several USA-based military helicopter EMS programs; and Life Link III, Minneapolis, Minnesota.
It has been demonstrated that the FAST examination can be performed rapidly and with relative ease in the helicopter.8 Using a SonoSite 180 ultrasound machine with a 3.5 MHz transducer, 10 flight clinicians performed 21 FAST examinations on 14 patients. Nine patients were simulated. They reported no effect on avionics and were able to complete the standard FAST examination in a mean time of 3 minutes. In 2004, Heegaard and coinvestigators applied a focused template for didactic ultrasound training with additional hands-on training in an ED.2 They found that flight clinicians could perform a wide variety of ultrasound examinations with good long-term retention (>90%) over 1 year. Ultrasound examinations were performed proficiently in the helicopter, although time and space constraints limited the clinicians’ ability to perform the complete FAST examination. One study analyzed the use of ultrasound to perform a screening examination on obstetric patients transported by helicopter.7 The Fetal Evaluation for Transport with Ultrasound (FETUS) is a screening examination that evaluates fetal heart rate, position, and movement and general condition of the placenta. The examination can be performed serially in flight with no acoustic distortion from rotor noise. In 2011, a study examined the feasibility of using M-mode to detect pneumothoraces during helicopter transport.16 Earlier studies on helicopter EMS ultrasound in the United States utilized the SonoSite 180, a 2.4-kg compact ultrasound machine with 3.5 MHz transducer. One helicopter EMS program (Life Link III, Minneapolis, Minnesota) utilized the SonoSite iLook ultrasound machine (1.4 kg) with a 3.5 MHz transducer, which was mounted in the helicopter for ease of use. Other studies have been utilizing newer generation ultrasound machines that have both M-mode and video recording capability.
Ultrasound use in ground ambulances has gained traction. In 2010, Heegaard reported on 104 FAST and abdominal aortic ultrasound examinations performed by 9-1-1 paramedics in the prehospital environment (Figure 4-3).17,18 Of the FAST exams performed, 7.1% were positive for intraperitoneal/pericardial fluid. Paramedics were unable to obtain adequate images in 7.7% (8/104) patients. All exams recorded 6-second video clips of each portion of the exam. FAST and aortic ultrasound exams performed by the paramedics had a 100% agreement with an independent emergency medicine physician ultrasound expert.
Figure 4-3. Flow diagram of patients included in Ultrasound study. AA, abdominal aortic; FAST, Focused Assessment with Sonography for Trauma; HCMC, Hennepin County Medical Center; PM, paramedic; PO, physician overreader. Reprinted with permission from Heegaard W, Hildebrandt D, Spear D, Chason K, Nelson B, Ho J. Prehospital ultrasound by paramedics: results of field trial. Acad Emerg Med 17(6):624–630, 2010.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 GERMANY
GERMANY AUSTRIA
AUSTRIA FRANCE
FRANCE UNITED STATES OF AMERICA
UNITED STATES OF AMERICA TACTICAL MEDICINE
TACTICAL MEDICINE REMOTE TELEMENTORED ULTRASOUND
REMOTE TELEMENTORED ULTRASOUND ULTRASOUND IN UNDER-RESOURCED SETTINGS
ULTRASOUND IN UNDER-RESOURCED SETTINGS
