The first trimester of pregnancy is a period of tremendous embryonic growth and development. Expectant mothers experience joy and anticipation but also great uncertainty and anxiety because of high failure and complication rates. The development of high-resolution endovaginal ultrasonography allows the pregnant uterus to be assessed earlier and with better resolution than ever before. The normal sequence of events in early pregnancy and the stepwise sonographic correlates are well described. The higher sensitivity and specificity of transvaginal ultrasound (TVUS) compared with transabdominal ultrasound (US) have resulted in the adoption of the transvaginal approach as the standard of care.
The practicing radiologist and obstetrician must be familiar with basic embryology and sonography of the first trimester to interpret studies accurately and counsel women about the status of their early pregnancies. This chapter will review the spectrum of US findings in the normal and abnormal first trimester. Ectopic pregnancy, retained products of conception, and gestational trophoblastic disease are covered elsewhere.
Embryology and Normal Anatomy
The first trimester of pregnancy encompasses the ovarian, conceptus, embryonic, and fetal phases of development. By convention it is based on menstrual dating. The first day of the last menstrual period (LMP) is an identifiable landmark for pregnancy dating, as no such marker exists for conception. For US purposes, gestational age and menstrual age are equivalent, with the first trimester beginning 2 weeks before fertilization, on the first day of the LMP, and concluding 12 weeks later. During the ovarian phase, weeks 1 to 2 of the first trimester and days 1 to 14 of the menstrual cycle, an ovarian follicle matures under the influence of follicle-stimulating hormone. A surge in luteinizing hormone results in ovulation usually on day 14. The ruptured follicle forms the corpus luteum in the ovary, which secretes progesterone to support a potential pregnancy. If implantation does not take place, the corpus luteum degenerates after approximately 14 days.
Fertilization occurs within the fallopian tube approximately 12 hours after ovulation, resulting in a zygote that undergoes several mitotic divisions over the next 4 to 5 days. The developing mass of cells reaches the uterus and subsequently organizes into a blastocyst with a central cavity, an inner embryoblast cell mass at one side of the cavity, and an outer trophoblast layer around the cavity. The blastocyst implants into the uterine lining by day 5. The embryoblast develops into the embryonic disk, and the trophoblast forms a primary yolk sac.
During the fourth menstrual week, there is rapid trophoblastic proliferation resulting in differentiation of the uterine decidual reaction and a primitive uteroplacental circulation. The primary yolk sac becomes smaller, eventually disappearing, as the secondary yolk sac forms. The bilaminar embryo develops adjacent to this, between the secondary yolk sac and the developing amnion. Over week 5, the embryo is converted from a bilaminar disk to a trilaminar structure with three germ layers (endoderm, mesoderm, and ectoderm), thereby bringing the conceptus period to an end and setting the stage for organogenesis in the embryonic period. The continued development of trophoblastic villi increases the surface area between the chorion and endometrium at the site of placentation. The menstrual period is usually missed during week 5, and it is only now that some of the developing structures of early pregnancy are able to be visualized with US.
The embryonic period spans weeks 6 to 10 and is a critical period of human development. The major organs develop, and the primordial heart can be seen beating around the sixth week. Disturbances during this time can give rise to major malformations in the developing embryo. As the trilaminar embryonic disk becomes a C-shaped embryo, it incorporates a portion of the yolk sac; the rest is extruded and becomes extraamniotic. The amnion expands to invest the umbilical cord and embryo. By the end of this period the major organ systems have formed and the embryo begins to take a human form with obvious limb buds.
The last 2 weeks of the first trimester represent the beginning of the fetal period, which is marked by rapid fetal growth and differentiation; the crown–rump length (CRL) doubles between weeks 11 and 14. The amniotic cavity continues to expand as the chorionic cavity shrinks. By the end of the first trimester the amniotic and chorionic membranes approximate, fusing early in the second trimester.
Normal First Trimester Ultrasound
Ultrasound Guidelines
US provides a safe and effective means of evaluating the first trimester of pregnancy. Published studies have failed to demonstrate adverse postnatal effects of B-mode US. Technical advances in endovaginal ultrasonography have made it possible to image embryonic and fetal structures earlier and with better resolution than ever before. Careful attention to the transvaginal technique is essential, using the highest frequency possible and image optimization to produce diagnostic images. The American Institute of Ultrasound in Medicine provides guidelines for the performance and recording of first trimester US examinations. At a minimum the evaluation should document whether a gestational sac is present, stating its location and whether it contains a yolk sac or embryo. The pregnancy should be dated, recording the CRL if an embryo is present and the mean sac diameter if not. Fetal number and the presence or absence of cardiac activity should also be documented. Finally the uterus, adnexa, and cul-de-sac should be assessed. Liberal use of video clips is extremely helpful.
Gestational Sac
Sonographically the gestational sac is the first landmark that can be visualized in pregnancy. It should be seen on TVUS when the serum quantitative human chorionic gonadotropin (hCG) level is greater than 2000 mIU/mL by the International Reference Preparation (IRP; approximately 4 to 5 weeks’ menstrual age). Exceptions occur in multiple pregnancy, ectopic pregnancy, and molar pregnancy. The sac first appears as the intradecidual sac sign , a small, round, well-defined fluid collection embedded in echogenic decidual tissue, eccentrically located adjacent to the hyperechoic line representing the endometrial cavity ( Figure 21-1 , A ). The intradecidual sac sign ( Figure 21-2 ) can be subtle and difficult to visualize. It is critical not to mistake a true gestational sac for a pseudosac , an endometrial fluid collection seen in ectopic pregnancy ( Figure 21-3 ). Unlike a gestational sac, the pseudosac is central within the endometrial cavity, is surrounded by a single layer of decidua, and may contain blood. A normal gestational sac is round or oval, located in the fundus or mid uterus, and is surrounded by echogenic decidual reaction. As the gestational sac grows, the double decidual sac sign is produced by the opposed layers of decidua capsularis, covering the sac, and the decidua parietalis, lining the endometrial cavity ( Figures 21-1, B , and 21-4 ). The two layers are separated by a thin hypoechoic rim of fluid in the endometrial cavity. The decidua basalis develops at the implantation of the gestational sac into the endometrium and will form the placenta. When definitively present, the double decidual sac sign reliably distinguishes an intrauterine pregnancy from a pseudosac. It is a transient sign, however, because the two decidual layers ultimately coapt and obliterate the endometrial cavity. Furthermore, there may be considerable interobserver variation in the detection of this sign; it is not a requirement to identify an intrauterine pregnancy; and it is often present after a yolk sac is identified, thus limiting its utility. Color Doppler imaging can demonstrate trophoblastic blood flow around the gestational sac. Doppler imaging is not routinely used in this setting, however, because of concerns regarding the effects of the increased energy output on the developing fetus.




Measurement of the sac is extremely important because sac dimensions are used to determine normal evolution of the early pregnancy and in dating. The mean sac diameter (MSD) is the mean of the three orthogonal measurements of the sac, not including the echogenic decidua ( Figure 21-5 ). The formula MSD (in millimeters) + 30 calculates the menstrual age in days. The MSD increases approximately 1 mm/day during the first 2 months of pregnancy, allowing assessment of adequate growth over time if an embryonic pole is not yet identified.

Yolk Sac
The yolk sac, which is actually the secondary yolk sac, is the first visible structure to form within the gestational sac. Its presence definitively confirms the presence of an intrauterine pregnancy. It should always be seen by TVUS when the MSD exceeds 10 mm, corresponding to a gestational age of approximately 5 to 5.5 weeks. A normal yolk sac is perfectly round and measures less than 6 mm in diameter ( Figure 21-6 ). It should be eccentric within the gestational sac, close to the wall to which it is attached by a stalk. The yolk sac will support the early pregnancy until the placenta takes over in the second trimester.
Embryo
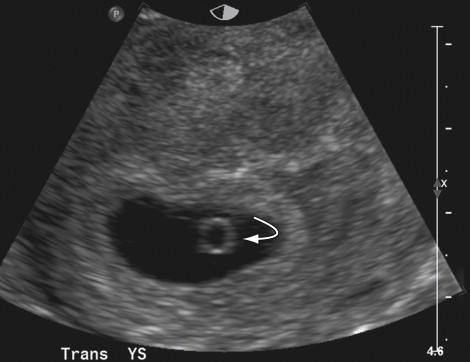
In a normal pregnancy, detection of the embryo is expected after the yolk sac, when the mean sac diameter exceeds 18 mm. This corresponds to a gestational age of approximately 6 to 7 weeks. The earliest sonographic sign of the embryo is the double bleb sign. The two blebs represent the amniotic sac adjacent to the yolk sac ( Figure 21-7 ). The embryo grows on the yolk sac but within the amniotic sac. The early embryo is seen as a disk of tissue between the two blebs (see Figure 21-7 ). As it grows, the embryo will appear as a focal thickening at the periphery of the yolk sac, referred to as the diamond ring sign ( Figure 21-8 ).












