, Joon Woo Lee1 and Jong Won Kwon2
(1)
Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Kyonggi-do, Republic of Korea
(2)
Department of Radiology, Samsung Medical Center, Seoul, Republic of Korea
13.5 Baastrup’s Disease
13.6 Epidural Lipomatosis
13.7.4 Scheuermann’s Disease
13.7.5 Baastrup’s Disease
13.7.6 Epidural Lipomatosis
Abstract
In this chapter, we will describe uncommon degenerative disorder such as ossification of the posterior longitudinal ligament, ossification of the ligamentum flavum, diffuse idiopathic skeletal hyperostosis, Scheuermann’s disease, Baastrup’s disease, and epidural lipomatosis. They may be causes of spinal stenosis and result in neck or back pain. The imaging features of them will be discussed in this chapter.
In this chapter, we will describe uncommon degenerative disorder such as ossification of the posterior longitudinal ligament, ossification of the ligamentum flavum, diffuse idiopathic skeletal hyperostosis, Scheuermann’s disease, Baastrup’s disease, and epidural lipomatosis. They may be causes of spinal stenosis and result in neck or back pain. The imaging features of them will be discussed in this chapter.
13.1 Ossification of the Posterior Longitudinal Ligament (OPLL)
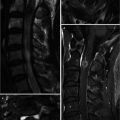
Ossification of the posterior longitudinal ligament (OPLL) is a pathologic condition in which the posterior longitudinal ligament of the cervical (C2–C5) or thoracic (T4–T7) spine is ossified and thickened. OPLL usually occurs in old patients and is very rare under age 40. Large OPLL can result in myelopathy or radiculopathy because of compression on the spinal cord or nerve roots. OPLL may be only located at the vertebral body levels without involvement of disk levels (segmental type), or it may continuously extend over several levels (continuous type). Continuous OPLL is significantly thicker, and the degree of spinal cord compression is more severe than segmental type.
Plain radiographs can demonstrate OPLL as vertical radiopaque bands behind the vertebral bodies. The posterior walls of the vertebral bodies can be mistaken for OPLL on the inaccurate lateral views. Anterior vertebral osteophytes are frequently accompanied. Axial CT images can distinguish OPLL from the vertebral body by a thin radiolucent zone and can depict the degree of central canal narrowing. Sagittal reformation of CT scan demonstrates overview of the flowing OPLL. MR can demonstrate the effect of OPLL on the spinal cord and detect compressive myelopathy. The signal intensity of OPLL is usually low on T1- and T2-weighted images but can be variable depending on the degree of maturation and the acquisition of marrow cavity. However, ossification cannot be completely differentiated from hypertrophied ligament with MR imaging (Yamashita et al. 1990), and MR can exaggerate the degree of spinal canal compromise.
13.2 Ossification of the Ligamentum Flavum (OLF)
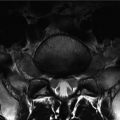
Ossification of the ligamenta flava (OLF) or ossification of the yellow ligament (OYL) generally occurs in the thoracic spine and mainly has been reported in the Asian population. The lower thoracic spine (T9–T12) is the most common location, and the cervical spine can be affected. Thickening of the ligamenta flava is frequently accompanied by facet joint arthropathy and is thought to be degenerative changes. OLF has a high incidence in elderly patients and predominantly affects males. Histologically OLF typically shows mature bone. Unilateral OLF is frequent and generally cause no clinical symptom, being detected incidentally. However, bilateral OLF can cause progressive thoracic myelopathy. OLF is incidentally detected in the thoracolumbar junction when reading the lumbar spine MRI, and the included lower thoracic spine should be closely observed. Axial MR imaging directly depicts the effects of spinal cord or dural compression posteriorly when present. CT shows the characteristic V-shaped, intense, radiodense lines with anterior concavity located in the posterior epidural space.
13.3 Diffuse Idiopathic Skeletal Hyperostosis (DISH)
Diffuse idiopathic skeletal hyperostosis (DISH) is a pathologic condition of diffuse ossification in the tendon insertions, ligaments, and fasciae in both the axial and the appendicular skeleton. The cause of DISH is unknown, and it mostly affects elderly (over the age of 50) men (Weinfeld et al. 1997). So DISH is thought of a kind of degenerative disorder. Many patients with DISH are asymptomatic. If present, the symptoms associated with DISH are intermittent spinal stiffness, restricted mobility, and nonspecific back pain. Dysphagia from esophageal compression can develop secondary to large anterior cervical osteophytes.
DISH predominantly involves the thoracic spine (T7–T11), and hyperostosis is predominantly right sided. Descending aorta pulsation is presumed to have an inhibiting effect on the left side of the spine. The thickness of the ossification is considerably varied. The osteophytosis across the intervertebral disk space shows irregular and bumpy spinal contour on lateral radiographs.
In the cervical spine (C4–C7), hyperostosis occurs along the anterior aspect of vertebral bodies. The elongated osteophytes may extend across the intervertebral disk space and are seen as either irregular and bumpy or homogeneous and smooth. Ossification of posterior longitudinal ligament of the cervical spine can be accompanied with DISH. Ossification of the stylohyoid ligament or elongation of the styloid process can be seen. Lumbar spine is affected in the upper lumbar region. The findings of DISH in the lumbar spine are similar to that in the cervical spine. Sagittal reformatted CT images easily demonstrate the typical findings.
DISH is predominantly a radiographic diagnosis and should be satisfied with the following radiographic criteria. Firstly, there should be flowing calcifications and ossifications along the anterolateral aspect of at least four contiguous vertebral bodies. Secondly, there is relative preservation of intervertebral disk height in the involved segment without radiographic changes of degenerative disk disease such as vacuum phenomenon and subchondral sclerosis. Lastly, there is absence of apophyseal ankylosis or sacroiliac joint erosion, sclerosis, or bony fusion. Each criterion is used to distinguish DISH from other spinal diseases: spondylosis deformans, intervertebral osteochondrosis, and ankylosing spondylitis (AS). The syndesmophytes of ankylosing spondylitis are thin and vertical ossification within the annulus fibrosus, whereas the spinal osteophytes of spondylosis deformans are triangular in shape and arise several millimeters from the diskovertebral junction. However, as DISH and AS are not rare diseases, they can occur in the same person by chance. In such a case, the radiography shows concomitant findings typical of AS (sacroiliac joint erosions, joint space narrowing, osteitis, and ankylosis) and DISH (anterior capsular bridging of the sacroiliac joint and bulky osteophytes).
DISH can have extraspinal manifestations as hyperostosis in the tendon and ligament insertion sites, including enthesophytes involving the iliac crest, ischial tuberosity, greater trochanter, acetabular margin, patella, and posterior and plantar surface of calcaneus.
13.4 Scheuermann’s Disease
Scheuermann’s disease is characterized by thoracic or thoracolumbar kyphosis, caused by a wedge-shaped deformity of three or more vertebrae (Lowe 1990). It refers to osteochondrosis of the secondary ossification centers of the vertebral bodies. The findings of Scheuermann’s disease are abnormal thoracic kyphosis, vertebral body wedging, disk space narrowing, Schmorl’s nodes, and irregularities of vertebral endplates on lateral radiographs. Scheuermann’s disease, however, can manifest as vertebral irregularity without wedging in the lumbar spine. The anterior-posterior diameter of the vertebral bodies may be increased. Scoliosis can be accompanied. Advanced degenerative disk disease such as vacuum phenomenon or subchondral bony sclerosis is often present in adults.
13.5 Baastrup’s Disease
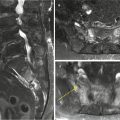
Baastrup’s disease or kissing spine is caused by chronic contact between adjacent spinous processes. It may cause sclerosis, flattening, and cystic erosions of the opposing superior and inferior surfaces of the spinous processes, which can be seen on lateral radiographs or sagittal reformatted CT images (DePalma et al. 2004). The Baastrup’s disease most commonly occurs in the lumbar spine (especially at the L4–5 level followed by the L3–4 level). Spine hyperextension or excessive lumbar lordosis leads to close approximation and contact of the spinous processes. Degeneration of the intervening ligaments results in interspinous pseudoarthrosis. The Baastrup’s disease is also thought to be associated with chronic active inflammation of adjacent facet joint (facet synovitis).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree