LEARNING OBJECTIVES
1. Recognize a unilateral hyperlucent hemithorax on a chest radiograph or computed tomography (CT).
2. Describe the common causes of a unilateral hyperlucent hemithorax on a chest radiograph or CT.
3. List an appropriate differential diagnosis when a hyperlucent hemithorax is seen on a chest radiograph or CT and suggest a specific diagnosis when certain associated findings are seen (e.g., absence of a breast after mastectomy, absence of a pectoralis muscle in Poland syndrome, unilateral or asymmetric bullous disease/emphysema, or air trapping on exhalation imaging in a patient with Swyer–James syndrome or an endobronchial foreign body).
The most common chest radiographic causes of a unilateral hyperlucent hemithorax do not reflect an intrinsic abnormality of the lung itself. Improper patient positioning is the most common cause. A slight degree of patient rotation will result in disparity in overall lung opacity on the posteroanterior (PA) chest radiograph (Fig. 14.1). By the same mechanism, scoliosis, if severe, may cause asymmetry of lung density. Mastectomy results in asymmetry of soft tissues overlying the lungs and relative radiolucency on the side of breast removal (Fig. 14.2). This common cause of unilateral hyperlucent hemithorax is easily overlooked unless the observer is methodical in always evaluating soft tissues on a chest radiograph. Marked asymmetry of breast tissue can also result in one hemithorax being more lucent than the other, although this is not commonly seen on chest radiography (Fig. 14.3). Absence of the sternocleidomastoid muscle results in hyperlucency of the upper hemithorax (Fig. 14.4). Absence of the pectoralis muscle also results in hyperlucency of the ipsilateral hemithorax (Figs. 14.5 and 14.6). When associated with ipsilateral syndactyly, brachydactyly, and rib anomalies, the condition is called Poland syndrome.
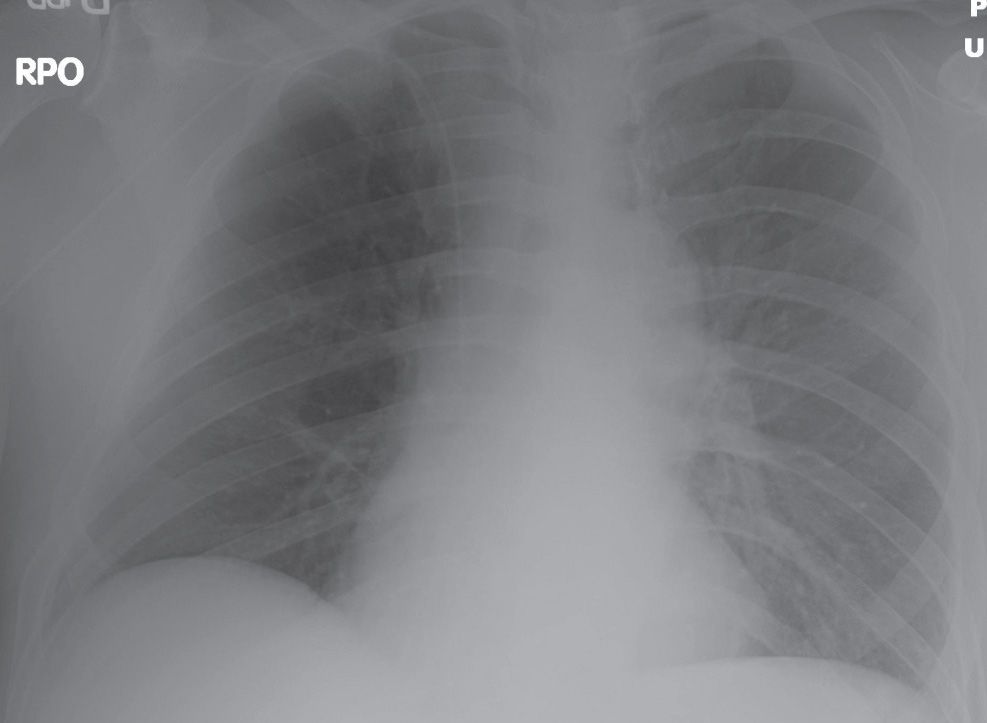
FIG. 14.1 • Rotation. Right posterior oblique chest radiograph shows relative lucency of the right hemithorax compared with the left.
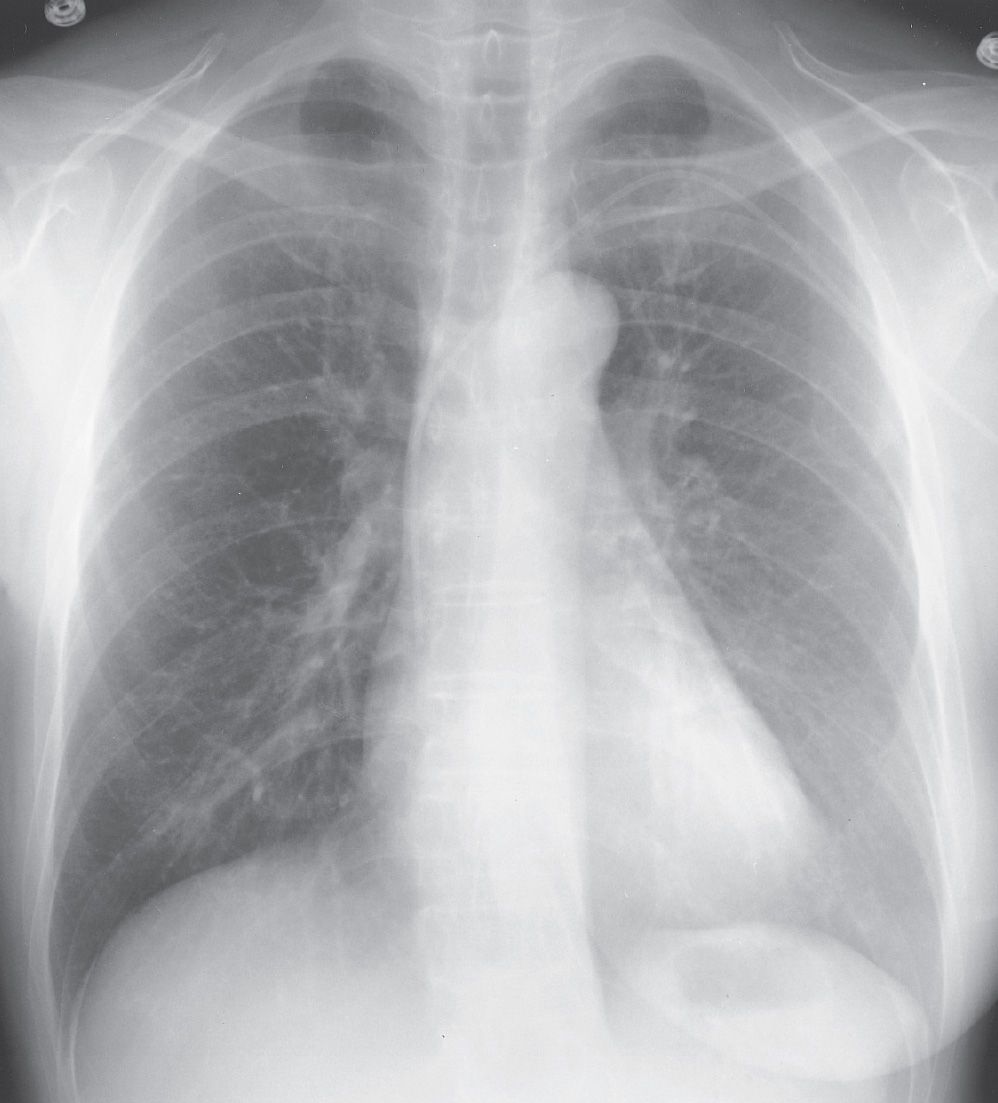
FIG. 14.2 • Mastectomy. PA chest radiograph of a woman after right mastectomy for breast cancer shows a breast shadow on the left but not the right; as a result, the right lung appears relatively hyperlucent compared with the left.
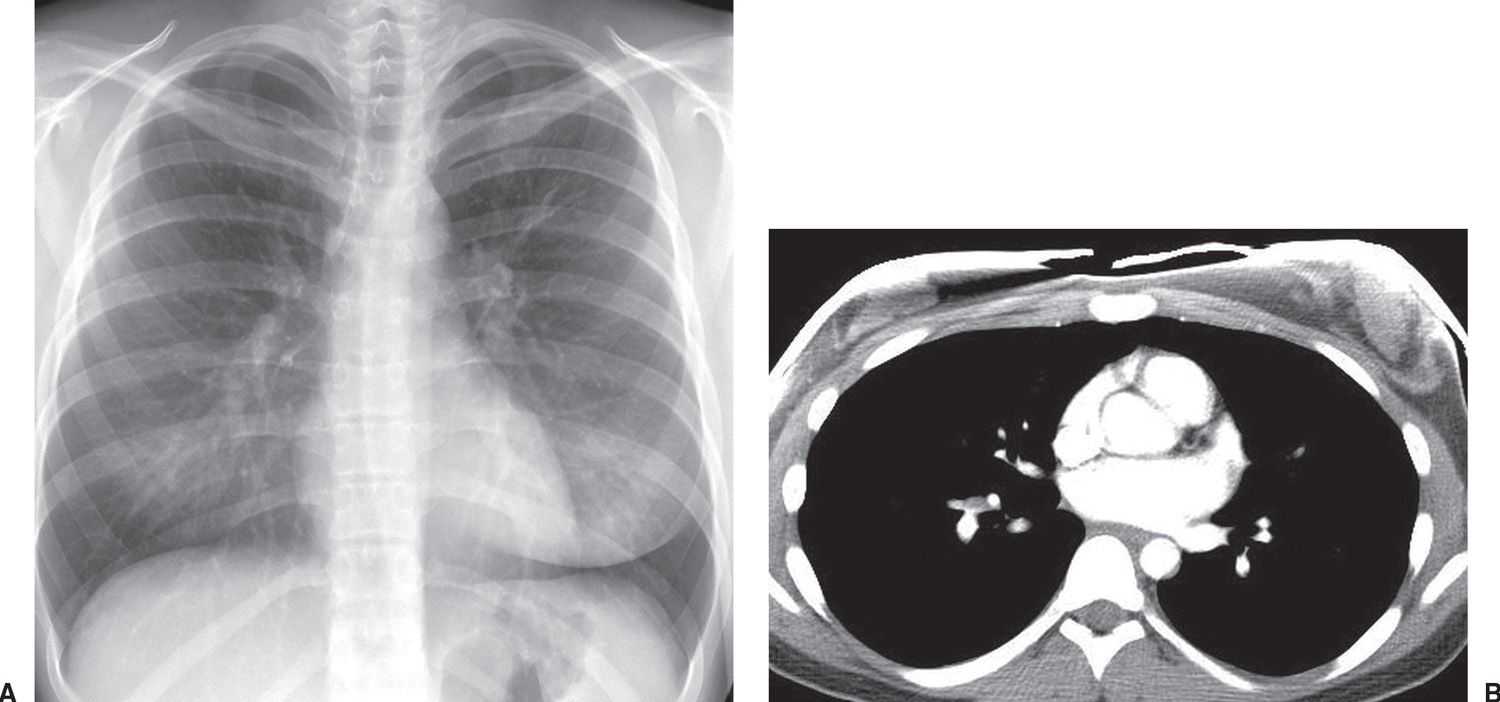
FIG. 14.3 • Asymmetric breast tissue. A: PA chest radiograph of an 18-year-old woman shows relative hyperlucency of the right hemithorax. The breast shadow on the right is diminutive compared with the breast shadow on the left. B: CT confirms decreased breast tissue on the right compared with the left. Anterior chest wall artifact is a result of breast shields placed on the patient.
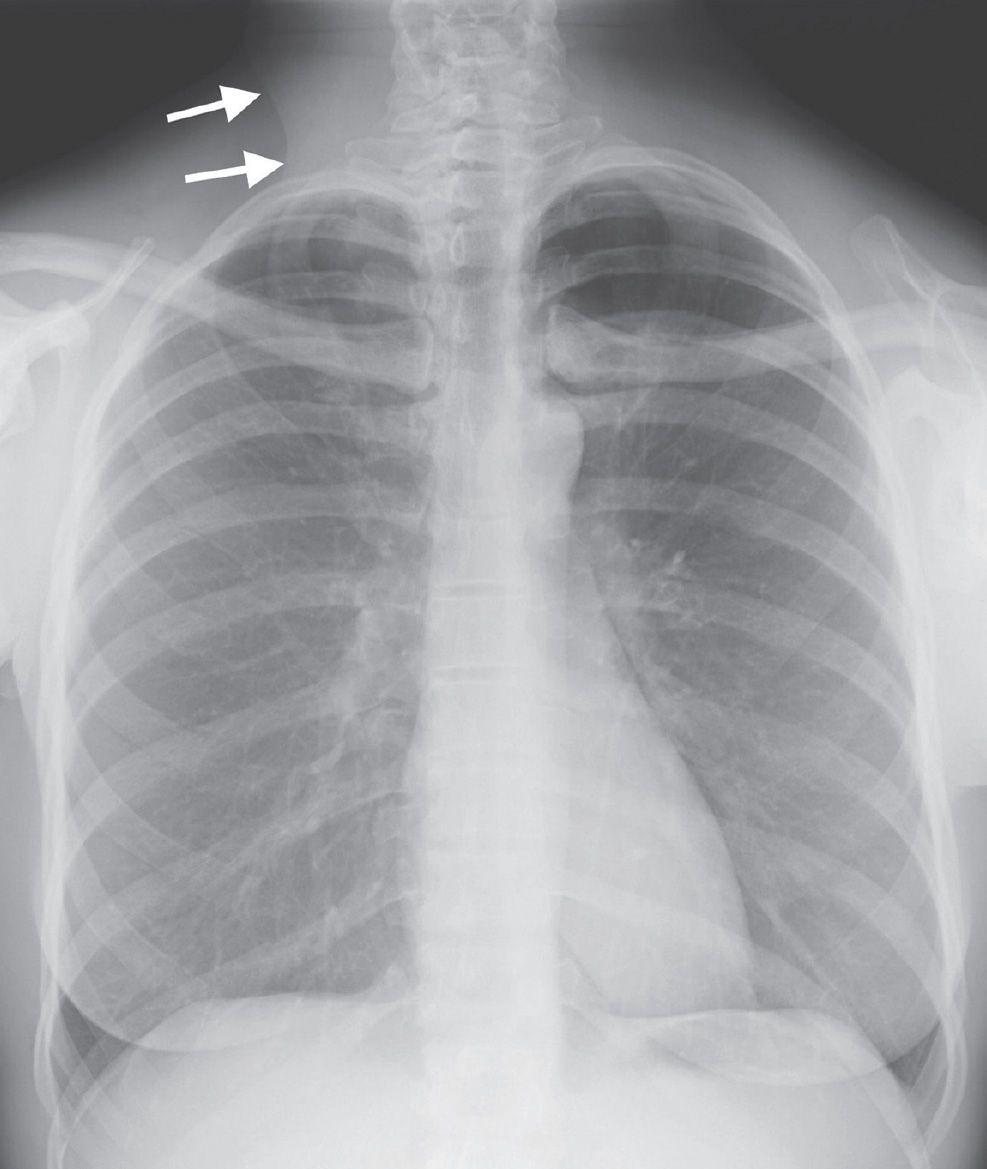
FIG. 14.4 • Absence of sternocleidomastoid muscle. PA chest radiograph of a 47-year-old woman with thyroid carcinoma who underwent left radical neck dissection shows hyperlucency of the left upper hemithorax. Note the normal sternocleidomastoid muscle shadow on the right (arrows) and absence of the shadow on the left.
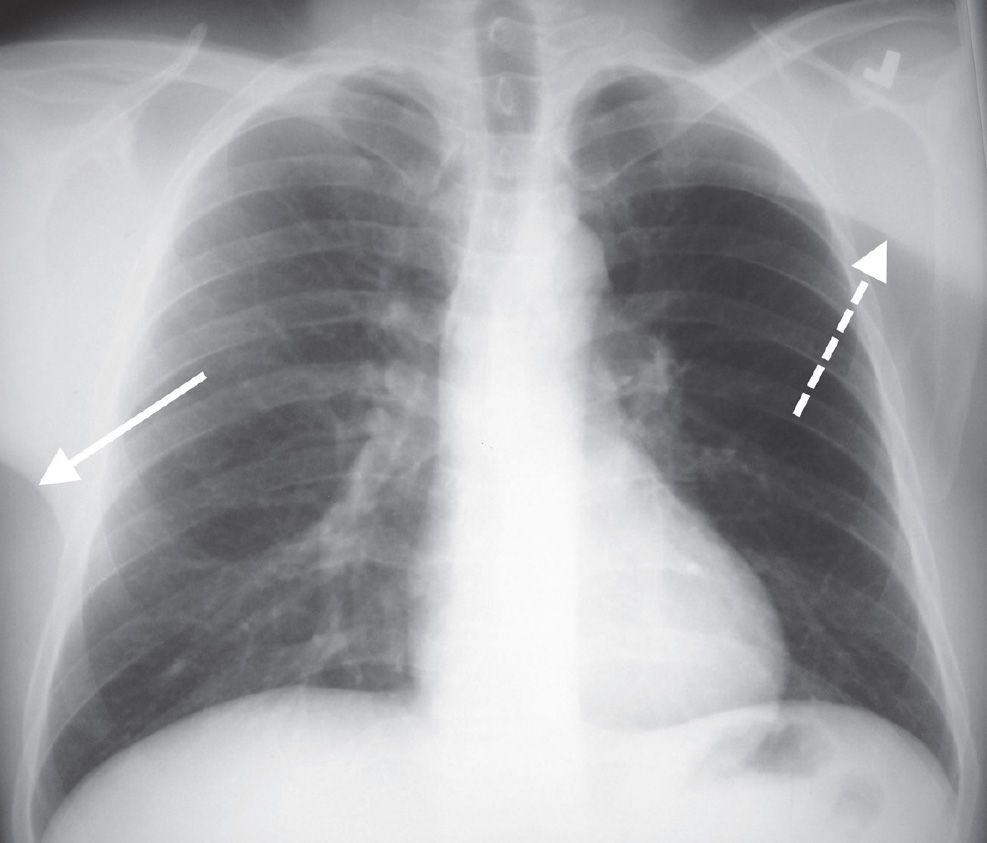
FIG. 14.5 • Absence of pectoralis muscle. PA chest radiograph shows relative hyperlucency of the left hemithorax because of the absence of the left pectoralis muscle. Note the normal pectoralis muscle shadow on the right (solid arrow) and abnormal elevation of the skin fold on the left (dashed arrow).
A large pneumothorax results in hyperlucency of the ipsilateral hemithorax and can be recognized by observing the displacement of the visceral pleural line, absence of lung markings distal to the displaced pleural line, and contralateral shift of the mediastinum (Fig. 14.7). Patients who have had pulmonary resections or who have lobar atelectasis may also show lucency of the residual aerated lung in the involved hemithorax because of compensatory hyperexpansion. A common cause of hyperlucent hemithorax in some hospitals is unilateral lung transplantation for pulmonary emphysema, where the native emphysematous lung is radiolucent relative to the lung transplant, which receives the bulk of the pulmonary perfusion (Fig. 14.8). In some cases of hyperlucent hemithorax, the lucent side is normal and the opposite side is abnormally radiopaque. Diffuse pleural thickening on the more opaque side or pleural fluid layering posteriorly on a supine radiograph are frequent causes (Fig. 9-8B).
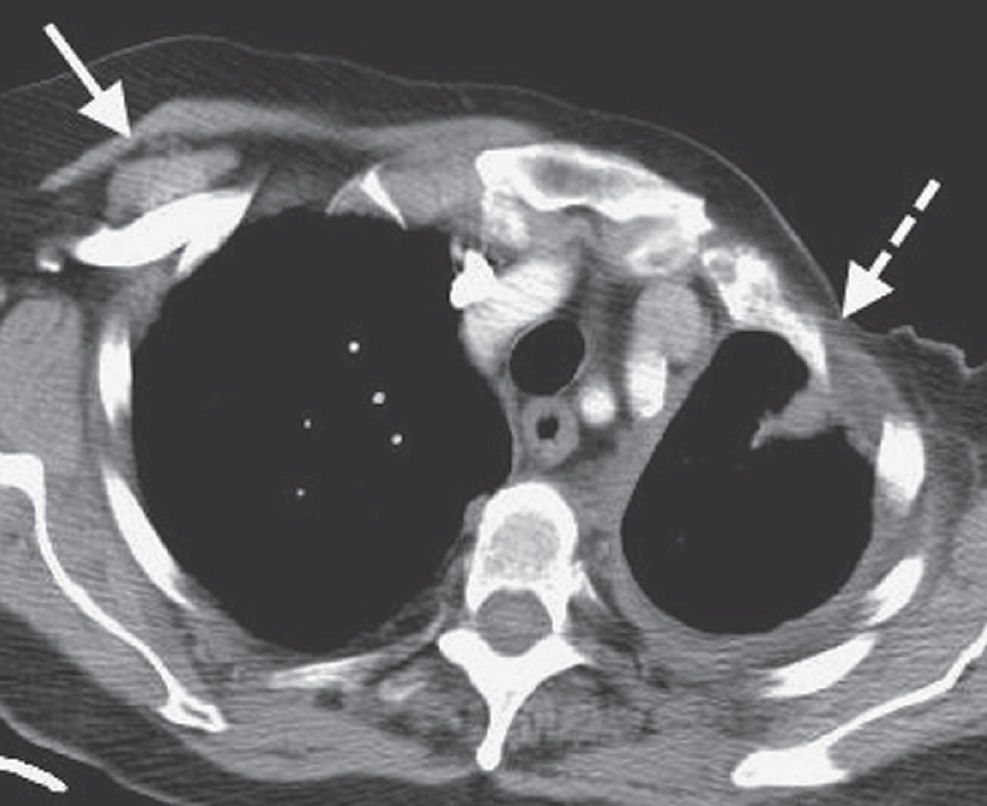
FIG. 14.6 • Absence of pectoralis muscles. CT of a woman who underwent left radical mastectomy for breast cancer shows pectoral muscles on the right (solid arrow) and absence of pectoral muscles on the left (dashed arrow).
The origins of true unilateral hyperlucent lung will be the focus of this chapter. After faulty radiologic technique and chest wall or pleural abnormalities are excluded as possible sources, the causes of unilateral hyperlucent hemithorax can be categorized into those primarily related to airway obstruction and those primarily related to decreased pulmonary blood flow (Table 14.1).
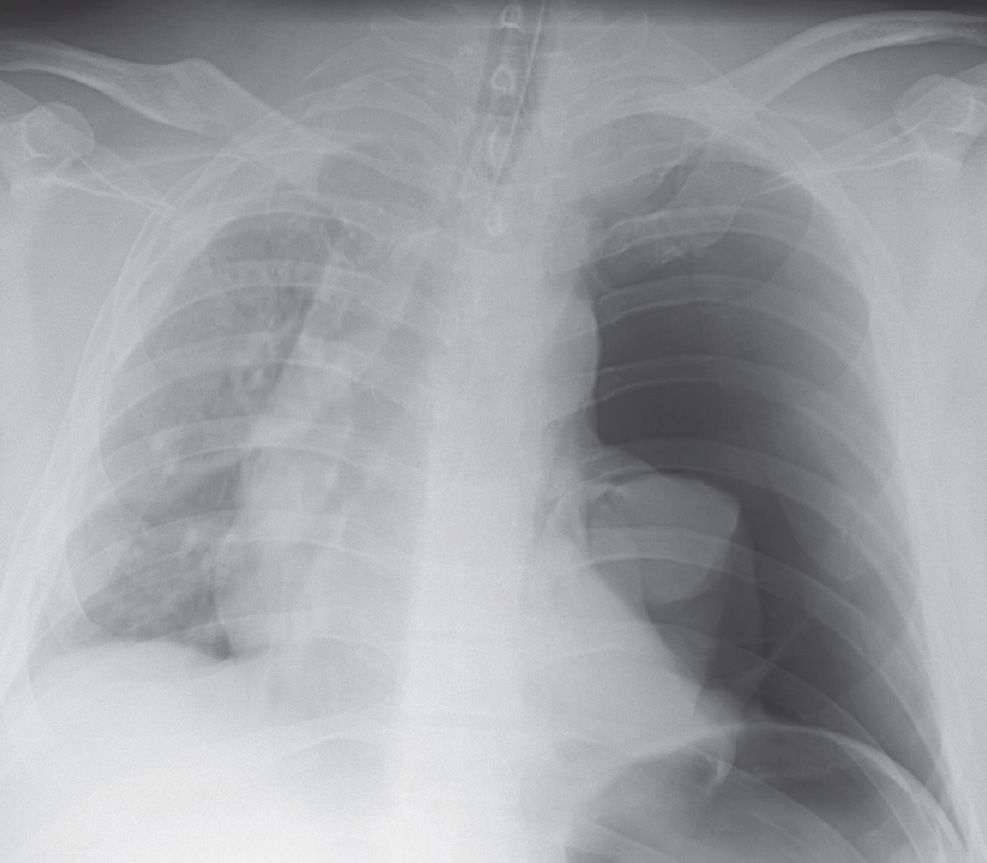
FIG. 14.7 • Tension pneumothorax. Anteroposterior (AP) supine chest radiograph of a 35-year-old man involved in a motor vehicle crash shows a large left pneumothorax, collapse of the left lung, and mediastinal shift to the right. The left hemithorax is hyperlucent compared with the right.

FIG. 14.8 • Left lung transplant. PA chest radiograph of a 62-year-old woman with a left lung transplant shows a hyperlucent right lung. The native right emphysematous lung is hyperlucent and hyperexpanded, causing mediastinal shift to the left.
AIRWAY OBSTRUCTION AS A CAUSE OF UNILATERAL HYPERLUCENT LUNG
The hallmark of airway obstruction on chest radiographs is the finding of air trapping. An exhalation-phase chest radiograph will usually show whether air trapping is present; this is manifested as failure of the lung to decrease in volume and failure of the lung to increase in opacity on exhalation compared with inhalation. In some cases, the mediastinum shifts to the side that is not trapping air on exhalational views. Air trapping occurs when an endobronchial lesion, usually a foreign body in a large airway, causes a ball-valve type of obstruction. The foreign body does not completely obstruct the bronchus in which it is lodged. During inhalation, the bronchial diameter normally increases, allowing air to pass around the foreign body and enter the lung distal to the obstruction. During exhalation, the bronchial diameter normally decreases, and the air is trapped within the lung distal to the obstruction. This allows a foreign body or tumor that does not completely obstruct a bronchus during inhalation to do so during exhalation. As a result, the lung, lobe, or segment distal to the obstructing lesion becomes increasingly distended until the pressure within it prevents more air from entering. In children, this type of ball-valve obstruction usually results from the aspiration of food, commonly a peanut, or a toy or coin. In adults, this type of obstruction can result from aspiration of foreign bodies but also, more important, from an endobronchial tumor (Fig. 14.9). Extrinsic masses, such as enlarged nodes or an enlarged heart, can obstruct a bronchus in a similar fashion.
Constrictive bronchiolitis is a syndrome of airflow limitation caused by bronchiolar and peribronchiolar inflammation and fibrosis, as was discussed in Chapter 13. In adults, it is most often idiopathic in etiology, but is also associated with lung and bone marrow transplantation as well as a variety of other insults to the lung. The Swyer–James, or MacLeod, syndrome is a form of constrictive bronchiolitis that occurs following an insult to the developing lung (1). In this syndrome, unlike in large, central airway obstruction, small bronchi and bronchioles are affected, and the lung served by abnormal airways remains inflated by collateral air drift. By definition, the airway disease as assessed by the chest radiograph is predominantly unilateral, giving rise to the key finding of unilateral hyperlucent lung. In practice, constrictive bronchiolitis is often bilateral and patchy. The injury to the immature lung, which occurs during the first 8 years of life, commonly follows a viral infection. Bronchi and bronchioles from the fourth generation to the terminal bronchioles have submucosal fibrosis, which causes luminal irregularity and occlusion. Pulmonary tissue is hypoplastic, including the pulmonary artery and its branches, which are reduced in both size and number. Lung distal to diseased airways is hyperinflated and supplied by collateral air drift. Sometimes panacinar emphysematous changes are present. Patients are typically asymptomatic, often presenting as adults with an incidental abnormal chest radiograph.
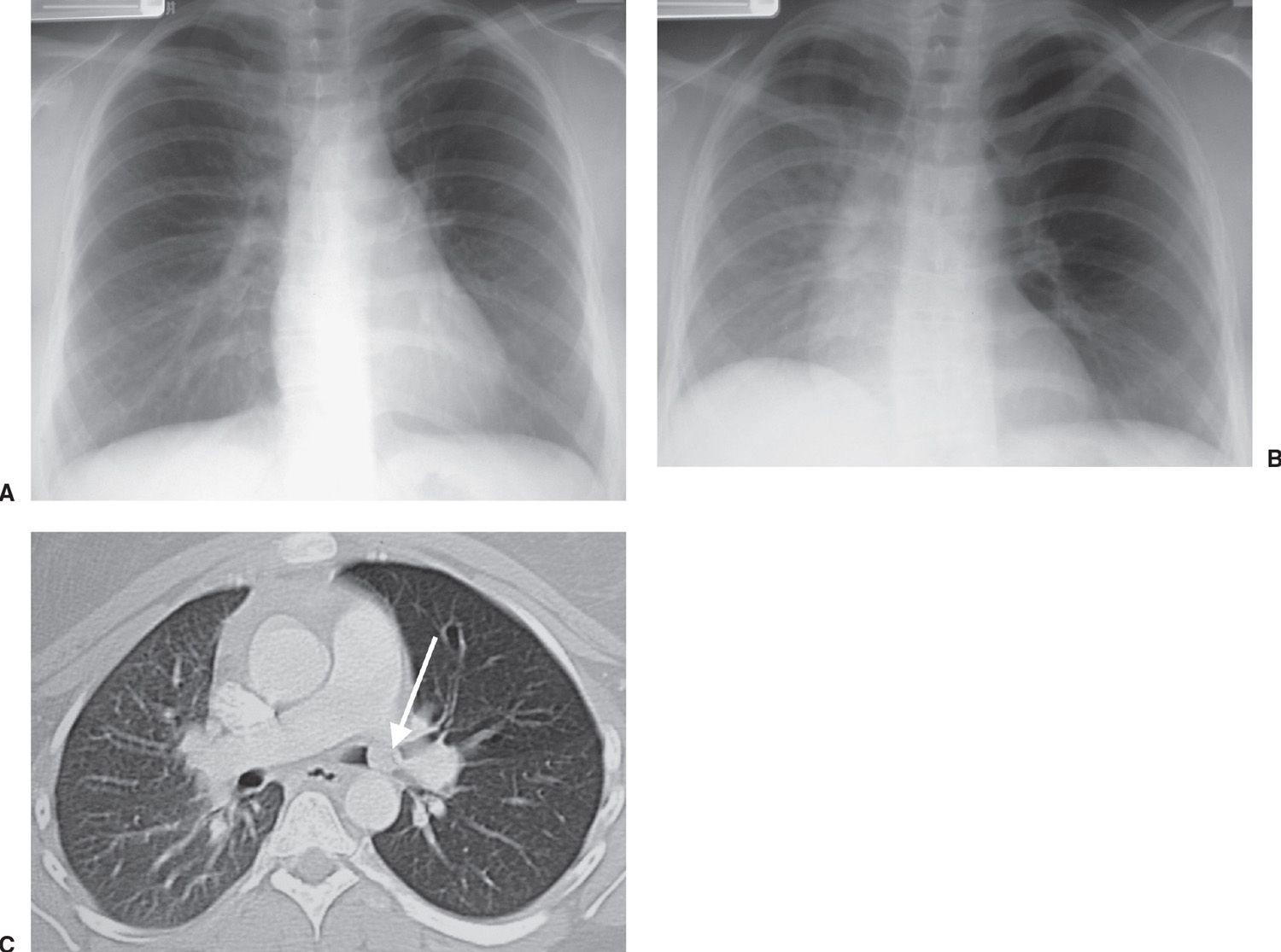
FIG. 14.9 • Carcinoid tumor. A: PA inspiratory chest radiograph of a 24-year-old woman with a prolonged history of wheezing, shortness of breath, cough, and recurrent pneumonia appears normal. The patient was treated for asthma with no relief in symptoms. B: PA exhalational view shows air trapping in the left hyperlucent lung and mediastinal shift to the right. C: CT shows a mass (arrow) in the left main bronchus. This mass results in a ball-valve obstruction, where air enters the lung during inhalation but cannot exit the lung during exhalation. Note that the left lung is hyperlucent relative to the right lung as a result of air trapping.
Table 14.1 CAUSES OF UNILATERAL HYPERLUCENT HEMITHORAX
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








