These quizzes were set up in the prior edition to simulate the oral boards in radiology. The oral boards have been discontinued, but you may find it interesting to “work against the clock.” These cases are more difficult and should be a challenge for radiology residents. If you are not a radiologist, try them or go out for a beer.
Instructions
There are three sessions (A, B, and C). Each session should take approximately 25 minutes. Time yourself, and try to complete as many cases as you can in the 25 minutes. If it takes longer, don’t worry or just ignore the clock completely.
For each case, you will be given a very brief history and a list of images available. Always describe the chest x-rays thoroughly before continuing to the cross-sectional images, if provided.
Once you have seen all the images, you may go back and forth between them. When you have finished the case, click “show” for the Findings and Diagnosis. Additional images may be presented with the explanation.
Remember, there may be more than one right answer. You are not expected to get every case perfectly correct. Good, clear, radiographic descriptions and differential diagnosis are more important than “blurting out the right answer without a clue as to why.”
Section A
Case A-1
History:
68-year-old male construction worker.


Images:
AP scout and CT
Findings:
The AP (A) image shows multilobular densities along the left chest wall and adjacent to the aortic knob. There are no rib lesions and the left costophrenic angle is blunted.
The CT (B) shows thick nodular pleura both medially and laterally. It is the same density as muscle, approximately 40 HU.
Diagnosis:
Diagnosis is mesothelioma. This man worked in a ship yard for years. He had heavy asbestos exposure.
Case A-2
History:
Older woman with recent onset of cough and low-grade fever.


Images:
Chest PA (A) and lateral (B).
Findings:
The lung volumes are large. There is a large mass in the left hilum. The hemidiaphragm is slightly elevated and there is a juxtaphrenic peak. The overall density of the left lung is greater than the right and the trachea is shifted slightly to the left. On the lateral film, the major fissure on the left is shifted anteriorly, delineating the collapsed left upper lobe and lingula.
Diagnosis:
Left hilar tumor, obstructing the left upper lobe bronchus, causing collapse of the left upper lobe and lingula. This was a small cell carcinoma.
Case A-3
History:
Young man in automobile accident 2 days ago. Recently returned from the operating room for repair of liver laceration.

Image:
AP chest.
Findings:
There are surgical sponges or drains in the right upper quadrant. The lungs are diffusely and homogeneously consolidated. The heart is not enlarged. The mediastinum is at the upper limits of normal, probably okay on a supine film. Curiously, both costophrenic angles are extremely dark and the upper diaphragms are lucent. The endotracheal tube, jugular catheter, and nasogastric tube are in good position.
Diagnosis:
ARDS caused by multiple trauma and transfusions. Bilateral pulmonary contusions are possible but less likely. Bilateral pneumothoraces on the supine x-ray. This is a bilateral deep sulcus sign.
Case A-4
History:
The patient is very dyspnic following evacuation of a subdural hematoma and coiling of the hepatic artery for a liver laceration.


Images:
AP portable chest ( Image A ).
Findings:
The right hemi-diaphragm is silhouetted. The right heart border is visible. There is collapse of the right lower lobe.
The left hemi-diaphragm is also silhouetted. The descending aorta is not visible behind the heart and the area behind the heart is uniformly dense. The proximal left lower lobe bronchus is seen but stops suddenly (see Image B) (click to see) .
Diagnosis:
Bilateral postoperative collapse of the lower lobes. There is no air bronchogram on the right indicating that mucus fills all of the bronchi. On the left, there is a discreet mucous plug in the proximal left lower lobe bronchus.
Case A-5
History:
Four patients with heart disease. Challenge: What is enlarged?





Images:
Four PA chest films.
Findings:
- A.
The left ventricle is prominent with the apex laterally and inferiorly. The cardiothoracic ratio is greater than 50%. The left atrium is concave. The main pulmonary artery is not seen and the aortic arch appears normal.
- B.
The main pulmonary artery protrudes laterally. The aorta, the left atrium, and the left ventricle appear normal.
- C.
There is a focal mass at the level of the aortic arch. This is a saccular aneurysm ( Image E ).
- D.
The heart bulges far to the right of the spine. The left ventricle is not enlarged. Pulmonary arteries are questionably enlarged and the aorta is somewhat tortuous.
Diagnosis:
- A.
Left ventricular enlargement. History of myocardial infarctions.
- B.
Large pulmonary artery in a patient with pulmonary artery hypertension.
- C.
Tortuous aortic shadow. The patient had an aortic dissection.
- D.
Enlarged right heart from tricuspid disease.
Case A-6
History:
One week post right upper lobectomy. New fever.


Images:
Chest PA and lateral view.
Findings:
The right costophrenic angle is blunt. There is a generalized increased density throughout the right hemithorax. One the lateral view, the density parallels the sternum, in the pleural space where the right upper lobe has been removed. Did you notice the air fluid level within it? You should have, the pen in the patient’s pocket points directly to it in the PA image. It is also visible behind the sternum on the lateral.
Diagnosis:
Empyema from a bronchopleural fistula after right upper lobectomy.
Case A-7
History:
A 70-year-old smoker.


Images:
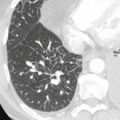
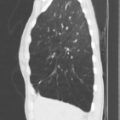
Two high-resolution CTs.
Findings:
Peripheral basilar honeycombing, ground-glass opacification, and traction bronchiectasis.
Diagnosis:
Usual interstitial pneumonitis.
Case A-8
History:
A 22-year-old male with hemoptysis.




Images:
Three coronal (A-C) and one axial (D) CT (contrast-enhanced).
Findings:
Tubular, branching structure in the anterior basal segment of the LLL. Axial image shows low-density branching structure.
Diagnosis:
Bronchiectasis and mucoid impaction. Size of bronchus suggests longstanding disease. An endobronchial tumor, foreign body, or segmental bronchial stenosis must be excluded.
Case A-9
History:
A 60-year-old female, preoperative examination.


Images:
Chest PA and lateral.
Findings:
The trachea is deviated to the left above the clavicles. Perhaps there is minimal tracheal narrowing as it enters the thorax. The lungs are otherwise clear. On the lateral, the upper retrosternal space is dense.

An ultrasound at the base of the neck shows an enlarged right lobe of the thyroid ( Image C ).
Diagnosis:
The diagnosis is goiter. This had been growing for many years. Although it did not appear to compromise the patient’s trachea, this was an important piece of information for the anesthesiologist who was about to intubate the patient for general anesthesia.
Section B
Case B-1
History:
Chest trauma.

Images:
AP chest.
Findings:
There is some minor atelectasis at the right base. There is no pneumothorax. There is a fracture of the eighth, right, posterior rib and subcutaneous emphysema in the right flank. ( Click for answer )