Introduction
The craniovertebral junction is designed to be strong in order to maintain the head on the shoulders. This junction is also supple and mobile to allow for looking at the world in all directions. While mobility and stability are the hallmarks, the architecture is immaculately tuned to provide a wide space for free traversing of critical neural and vascular structures. A large complex of ligaments and bones provide infrastructure to the muscles that power the movements. The human spinal pillar has a Y-shaped configuration. The rostral “V” of the “Y,” which is composed of suboccipital bone, atlas, and axis vertebrae, constitutes the craniovertebral junction. The occipitoatlantal joint is the center for stability. The occipitoatlantal joint, by its constitution and by the strength of its ligaments, is one of the strongest joints of the body. The atlantoaxial joint is the center for mobility. The flat and round atlantoaxial articulation that facilitates circumferential movements also makes this joint prone for instability. The term craniovertebral instability can be synonymous with atlantoaxial instability because, whereas atlantoaxial instability is relatively common, occipitoatlantal instability is significantly infrequent and is rarely identified in cases with severe trauma and in “syndromic” children.
Investigations for Atlantoaxial Instability
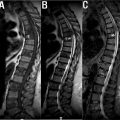
Plain radiology was used to investigate and diagnose atlantoaxial dislocation until computer imaging radically changed preoperative investigations. Lateral radiographs with the head in flexion and extension were the most frequently conducted investigation. ( Fig. 1 ) On the basis of this investigation, atlantoaxial dislocation is diagnosed when the atlantodental interval (distance between the posterior limit of anterior arch of atlas and the anterior border of odontoid process) was more than 3 mm on flexion of the head. In children, the atlantodental interval of 3 to 5 mm is sometimes considered to be within the range of normalcy. The dislocation was considered reducible when the atlantodental interval returned to normal on head extension; it was considered irreducible or fixed or partially reducible when the atlantodental interval did not or incompletely return to normal on head extension.

Computer-based imaging : Introduction of computer-based imaging of CT scan and MRI in the later quarter of the previous century has improved the understanding of the craniovertebral junction pathology and has helped in the identification of the optimum format of treatment. 3-D models are the latest introduction in the investigative armamentarium. This investigation aids understanding of the anatomy in the upper cervical spine and in selection of the best site and direction of screw insertion. This investigation is particularly useful in the treatment of complex craniovertebral junction abnormalities.
Atlantoaxial Facetal Instability
A new classification of atlantoaxial dislocation was based on evaluation of the alignment of the facets on lateral profile imaging with the head in neutral position. Visualization of the facets is not always clear in the imaging based primarily on plain radiography. Both CT scan and MRI clearly depict the status of the facets.
Horizontal facetal instability
Anterior atlantoaxial facetal (or type 1 ) dislocation : The alignment of the facets, weight of the head, and dominance of flexion movements more often result in an anterior facet dislocation of the atlas over the facet of axis ( Fig. 2 ). Such dislocation is characterized by an increase in the atlantodental interval, and can result in the compression of the dural tube and neural structures by the odontoid process. As there is neural compression and deformation, such dislocations are usually associated with acute symptoms.

Posterior atlantoaxial (type 2) facetal instability
Posterior atlantoaxial facetal dislocation (type 2) occurs when the facet of the atlas is located posterior to the facet of axis ( Fig. 3 ).

Type 3 facetal instability
Type 3 atlantoaxial facet dislocation is when the facetal surfaces of the atlas and axis are aligned ( Figs. 4 and 5 ). However, other clinical and radiological parameters suggest instability. Instability is confirmed in such cases by an intraoperative observation of the status of the facets on direct manual handling of bones.


Central or axial atlantoaxial instability: In types 2 and 3 atlantoaxial facetal dislocations, the atlantodental interval may be normal or relatively unaffected, and the odontoid process may not displace into the spinal canal or cause neural compression. Such types of atlantoaxial instability are classified as “central or axial” atlantoaxial instability. Identification of central atlantoaxial facet instability is based on clinical suspicion and subjective observations. Understanding that central instability occurs in these cases can provide a critical opportunity for curative treatment in the form of a stabilization procedure.
The concept of “central or axial” atlantoaxial instability, wherein there can be atlantoaxial instability, even in the absence of altered atlantodental interval or evidence of neural compression, has expanded the scope of treatment. As neural compression is not early or a primary issue in these cases, the presenting symptoms are usually longstanding. Several commonplace clinical entities like basilar invagination, Chiari formation, syringomyelia, cervical myelopathy related to cervical spondylosis, and ossified posterior longitudinal ligament can present with pathology related to central or axial atlantoaxial instability.
Lateral atlantoaxial facetal dislocation occurs when the facets of atlas are dislocated lateral to the facets of axis ( Fig. 6 ). Fracture of the anterior and posterior arches of the atlas due to trauma or infection or bifid/trifid constitution of the arches can result in lateral dislocation of the facets of atlas over the facets of axis. Bifid anterior and posterior arches of the atlas are frequently associated with atlantoaxial dislocation and basilar invagination. Although it is difficult to measure, the bifidity of the arches can have a dynamic constitution resembling an opened or closed door. The posterior door or bifid opens upon flexion of the neck and accommodates to an extent the abnormal intrusion of the odontoid process into the spinal canal. The door closes upon extension of the neck when the odontoid process returns to its normal position.

Rotatory atlantoaxial dislocation: Depending on the location of the facets, rotatory atlantoaxial dislocation can be of various types. The more common type of rotatory dislocation occurs when the facet of atlas is dislocated posterior in relation to the facet of the axis on one side and anterior in its relationship on the contralateral side ( Fig. 7 ). The dislocation can result in painless torticollis in young children. The head is in a “cock robin” position. As there is no pain or neural deficit or symptom, and the main complaint is abnormal neck posture, the management of such cases needs to be precise and based on the understanding of biomechanics of the region.

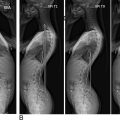
Vertical mobile Atlantoaxial Dislocation: Vertical mobile atlantoaxial dislocation occurs when the odontoid process moves up or rostrally in relationship to the anterior arch of atlas with flexion of the head and returns to its normal position on neck extension ( Fig. 8 ). The movements of the odontoid process resemble a piston. Ultimately, incompetence of the facet joint is the etiology of vertical atlantoaxial dislocation.

Acute and Chronic “Mobile and Reducible” Atlantoaxial Dislocation ( Fig. 9 )
Acute atlantoaxial dislocation often results from moderate to severe trauma that is associated with sudden mechanical stretch on the ligaments, leading to their disruption or incompetence. In chronic or longstanding atlantoaxial dislocation, the neural structures adapt to and tolerate the abnormal movements of the odontoid process. The exact etiology of chronic atlantoaxial dislocation may also remain uncertain. Although a history of trauma is usually present, the majority of etiologies (particularly in the pediatric age group) are related to developmental defects or genetic syndromes that result in abnormal ligamentous laxity. Compared with patients with a trauma-related acute dislocation, the mobility of the facets is usually significantly higher in patients with chronic dislocation, due to ligamentous laxity.